News 4/16/21
Top News
Mayo Clinic launches Remote Diagnostics and Management Platform, which offers AI-powered algorithms and care protocols to help clinicians deliver care remotely.
Mayo also formed two portfolio companies with partners to support its efforts: Anumana (digital sensor diagnostics analysis) and Lucem Health (connecting remote patient telemetry devices with algorithms and for integrating insights into clinical workflow).
The companies raised Series A funding rounds in conjunction with the announcement of $25.7 million and $6 million, respectively.
Mayo Clinic Platform President John Halamka, MD says he expects its work to generate other algorithm companies as society moves from episodic care to continuous care using signals, data, and AI.
In unrelated news, John is wearing a blue dress shirt, tie, and round black glasses in the video above, sporting some new personal branding after decades of the black jacket / black tee combo with wire frames.
Reader Comments

From History Reader: “Re: healthcare IT company names. I’ve been trying to remember the one named after a lizard and I’m stumped.” That would be Axolotl, the HIE platform vendor that was acquired in 2011 by UnitedHealth Group-owned Ingenix, which was later rolled up with several other divisions under the Optum nameplate. It was one of my favorite names and made for some fun HIMSS conference giveaways.
From Clicker Quicker: “Re: sponsors. What have you changed to attract the support of new companies?” I haven’t changed much of anything in my nearly 18 years of writing HIStalk. I just keep showing up, which in life is often enough to beat the competition. But health IT has a lot of new, well-funded digital health players who are anxious to gain a toehold and thus come a-calling. The herd-thinning that I would have predicted a year ago due to vendor consolidation was more than offset by this creation of new digital health subcategories. I haven’t seen this much vendor activity since the early days of Meaningful Use, when the investment amounts featured fewer zeroes.
From WebinAren’ts: “Re: webinars. How do sites guarantee the number of attendees? Been wondering that.” Beats me, since attendee count will be driven by the topic, abstract, presenters, and the annoyance level of the signup page, none of which are controlled by whoever is promoting the webinar. Although a chief marketing officer told me once that they advertised with an organization that guaranteed high number of leads, drew a tiny fraction of that as webinar attendees, and then were just given a bunch of random names that had been dumped from a different database to make up the difference, which hardly counts as a lead.
HIStalk Announcements and Requests
Welcome to new HIStalk Platinum Sponsor Sonifi Health. The Sioux Falls, SD-based personalized patient engagement company offers the technology and service platform for a smarter hospital: interactive TV with a mobile solution, streaming to patient room TVs using personal devices and subscriptions, digital whiteboards with staff information and patient goals, EHR-powered digital door signs, digital signage for public or staff spaces, and an interactive patient status board. These provide a better patient experience, deliver patient education, and improve quality and safety. The company provides a complete solution, using the client’s existing infrastructure to deliver a white-label solution to hospitals, cancer centers, ambulatory clinics, outpatient surgery centers, post-acute rehab facilities, and senior living / LTC facilities in serving 500 million end users annually around the world with 600 employees, 200 field technicians, and a 24/7 US-based call center. Clients include Stanford Health Care, University of Florida Health, Cedars Sinai, Texas Health Resources, and Adventist Health. The company offers integration with 30 systems, including Epic, Cerner, Meditech, Hillrom, Healthwise, Vocera, Cbord, Staywell, and Elsevier. Thanks to Sonifi Health for supporting HIStalk.
I found this Sonifi Health overview on YouTube.
Webinars
April 20 (Tuesday) noon ET. “The Modern Healthcare CIO: Digital Transformation in a Post-COVID World.” Sponsors: RingCentral, Net Health. Presenters: Dwight Raum, CIO, Johns Hopkins Medicine; Jeff Buda, VP/CIO, Floyd Medical Center. A panel of CIOs from large health systems will discuss how the digital health landscape is changing and what organizations can do now to meet future patient needs. Moderator Jason James, CIO of Net Health, will guide the panelists through topics that include continuum of care and telemedicine, employer-provided care delivery, consumerization of healthcare, and sustainability and workforce management.
April 21 (Wednesday) 1 ET. “Is Gig Work For You?” Sponsor: HIStalk. Presenter: Frank L. Poggio, retired health IT executive and active job search workshop presenter. This workshop will cover both the advantages and disadvantages of being a gig worker. Attendees will learn how to how to decide if gig work is a good personal fit, find the right company, and protect themselves from unethical ones.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
UnitedHealth Group posts Q1 results: revenue up 9%, adjusted EPS $5.31 versus $3.72, beating Wall Street estimates for both. The company’s market capitalization is $369 billion.
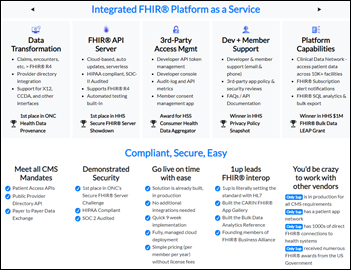
Boston-based 1upHealth raises $25 million in a Series B funding round. The 70-employee company offers a FHIR API solution for patient and provider connectivity for payers (EHR integration, population health analytics, member data access); providers (aggregating data from external sources, clinical trials support, patient-facing applications, payer integration, and medical research); and app developers (EHR-connected SMART tools, cost billing, and clinical trials recruitment).
NantHealth obtains $137 million in financing from existing investors. NH shares dropped 12% on the news, valuing the Patrick Soon-Shiong-controlled company at $289 million.
Jay Parkinson, MD, MPH announces in a blog post that Crossover Health shut down Sherpaa — the virtual primary care and technology company he founded and then sold to Crossover two years ago — at the end of last year. Parkinson has left Crossover, saying that he was too early with Sherpaa, he is burned out, and he is frustrated at seeing newer companies use his ideas to raise large amounts of investor cash. I’m not sure what happened to Hello Health and Myca, EHR-related vendors with which he was once associated.
The Santa Barbara, CA newspaper profiles local tech firm Evidation Health, whose platform monitors a user’s health data to send nudges. The company’s most recent funding round values it at more than $1 billion. The company lists five co-founders among its eight-member executive team, which is surely a record.
Sales
- University of California Health extends its Sectra Enterprise Imaging solution with VNA, universal viewer, and worklist manager.
- St. Joseph’s Healthcare Hamilton selects Spok Go for secure digital communication and will collaborate with the company as a development partner, initially to optimize on-call scheduling.
- Edward-Elmhurst Health will work with Impact Advisors on innovation, business process optimization, and information services. Both organizations are headquartered in Naperville, IL.
- SIU Medicine chooses Emerge ChartScout, ChartSearch, and ChartGenie to create a consolidated, searchable database that harmonizes disparate EMR data.
People

Loyal promotes Steph Geissinger to chief customer officer.


I missed this earlier: SOC Telemed promoted President John Kalix to CEO went it went public via SPAC late last year. Former CEO and long-time industry investor Steve Shulman moved to board chair.

Senior independent living company InnovAge hires Alice Raia, MSM (Kaiser Permanente) as CIO.
Announcements and Implementations
Digital health vendor K Health, insurer Anthem, and investment firm Blackstone form Hydrogen Health, which will use K Health’s AI technology to develop solutions for consumers, employers, and insurers. K Health co-founder and CEO Allon Bloch, MBA will additionally serve as the new company’s CEO.

EClinicalWorks announces implementation of its Vaccine Administration Management Solution, which is supporting COVID-19 vaccine administration in 29 states, with online appointment booking, patient reminders, contactless check-in, documentation, data transmission to vaccine registries, and inventory management.
Investor-owned hospital operator LifePoint Health and patient management software vendor Eon sign a five-year deal to develop Healthy Person Program, which will focus on early disease detection, timely notification to providers of findings and patients, and improved patient follow-up, starting with aortic aneurysms. Eon emphasizes use of its computational linguistics models to capture incidental findings, which it says is the #1 way to boost hospital earnings by keeping patients within the system. Founder and co-CEO Akrum Al-Zubaidi, DO is a pulmonologist who founded lung cancer screening technology company Matrix Analytics in 2014, which was renamed Eon in 2018.

CHIME, which recently ended its participation in the HIMSS conference, partners with the HLTH conference to offer Vive, an annual “reimagined health technology event” whose first conference will be held March 6-9, 2022 in Miami Beach. It will offer digital health innovation content, CHIME’s Spring Forum, an exhibit hall, and a matchmaking program that pairs potential buyer attendees with vendors. Some of the 18 title sponsors are also exhibiting at HIMSS21, but notable companies that will be only at Vive, at least according to HIMSS21’s exhibitor list so far, include Allscripts, Cerner, and Meditech. In an interesting adjacency of time and space, Vive will convene eight days before and 230 miles away from HIMSS22 in Orlando.
Government and Politics
The VA reaffirms that it will not bring its second Cerner site live in Columbus, OH until it has completed a strategic review of the project and shared the results with Congress, following concerns from users at the first site in Spokane, WA.
HHS tells hospitals to stop hiding their federally required pricing transparency information by adding website code to make it invisible to web searches.
COVID-19
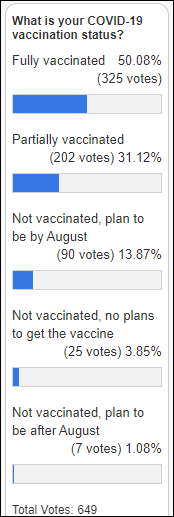
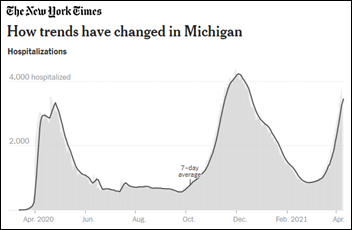
CDC reports that 48% of the eligible US population has received at least one dose of COVID-19 vaccine and 30% are fully vaccinated. US cases, hospitalizations, and deaths are trending up.
CDC’s independent immunization review group declines to make a recommendation on the use of Johnson & Johnson’s COVID-19 vaccine, which was paused this week after reports that six people developed severe clotting problems shortly after being vaccinated. Some committee members said they didn’t have enough information to make a recommendation or to suggest that the vaccine’s use be limited to certain populations. Experts say the group’s lack of action not only leaves J&J’s vaccine on the sidelines for what could be weeks, it also impacts vulnerable populations for whom the one-shot vaccine is their best hope of gaining COVID-19 protection. Still, observers expect the delay to last just a few days, with the more significant damage being vaccine hesitancy that is specific to the J&J product.
Moderna plans to make a COVID-19 vaccine booster shot available by fall, offering a third shot that will protect people from variants going into the fall and winter season.
Other
CHIME opens its Digital Health Most Wired survey. My early experience of multiple years of participating in (and winning) Most Wired before CHIME took it over in 2017 was that it was a kind of breezy and thus not something I found particularly brag-worthy, but a look at the 44-page, highly in-depth survey instrument shows that earning a high level of certification is a bigger deal than before.

Harvard Pilgrim, Kaiser Permanente, and Priority Health disclose enrollment numbers for their lower-cost, telehealth-first plans. Harvard Pilgrim sold one group account out of 60 pitched, KP of the Mid-Atlantic States expects 1,000 members, and Priority Health enrolled 5,000 members, 2,000 of whom switched from another of its policies. They note the challenges involved in offering telehealth-first health insurance:
- It may not be a good choice for people with limited mobile device access or poor Internet connectivity or data plans that can’t support video visits.
- Users need to be technically comfortable with updating apps and clinically comfortable taking their medical visits online.
- Healthcare.gov and other marketplaces don’t provide enough space to fully describe how telehealth-first plans work.
- New enrollees need to be contacted to make sure they understand what their plan involves and how to choose a new PCP.
- Health plans that try to launch their own telehealth service will be slowed down by individual state licensing for insurers and providers.
- Harvard Pilgrim and Priority Health partnered with Doctor On Demand, while KP developed its own program using its existing technologies and telehealth-comfortable clinicians.
Sponsor Updates
- EClinicalWorks publishes a podcast titled “Strengthening Patient Engagement During a Pandemic.”
- Ingenious Med publishes a new white paper, “How to Minimize Physician Burnout and Optimize Revenues: Lessons Learned from the Pandemic.”
- CHIME honors Ellkay CIO Marc Probst with its “CIO of the Year” award.
- Change Healthcare stockholders approve the previously announced combination with UnitedHealth Group’s OptumInsight.
- Healthcare Triangle partners with CareTech Solutions to offer Meditech customers hosting solutions and managed services.
- Everbridge wins 2021 Comparably Awards for best company outlook, best global culture, best sales team, and best place to work.
- Healthcare Growth Partners publishes “Health IT Q1 2021 Insights.”
- Healthwise partners with accounting and advisory firm Frazier & Deeter in a pilot program that will help HITRUST improve its assessment process.
- Healthcare IT Leaders, BD, and TrackMySolutions delivered COVID-19 testing for sports marketing firm IMG during Masters week.
- Impact Advisors will partner with nearby Edward-Elmhurst Health on innovation and transformation, business process optimization, and information services.
- LexisNexis Risk Solutions wins several Cybersecurity Excellence Awards.
- Meditech places among the top large vendors in a new KLAS report, “Vendor Performance in Response to the COVID-19 Crisis.”
- Microsoft adds NextGate’s Enterprise Master Patient Index to its Azure Marketplace.
Blog Posts
- Bring Your Own Device: The Evolution of Patient Engagement (GetWellNetwork)
- New Software Eliminates Guess Work in Troubleshooting and Documenting Remote Worker Issues (Goliath Technologies)
- Survey Says: 3 Purchase Strategies for Healthcare Communication Solutions (Halo Health)
- Benefits of Virtual Go-Live Support (Optimum Healthcare IT)
- The Evil Side of NPM (Health Data Movers)
- The Truth About the COVID-19 Vaccine: Separating Fact from Fiction (Healthwise)
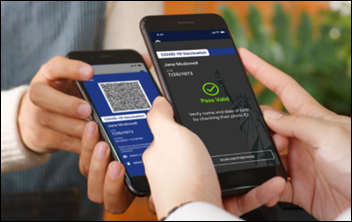
- In Healthcare, Digital Identity is More Important than Ever (Imprivata)
- Study: Clinical AI Reduces All-Cause Hospital Readmissions by 25% in 6 Months (Jvion)
- Building Consumer Relationships with Your Vaccine Rollout: A Conversation with Banner Health & Ochsner Lafayette General (Kyruus)
- Why is interoperability so important for healthcare organizations? (Lyniate)
- Improve Operating Room Operations with a Revitalized Perioperative Solution (Medhost)
- HCCs: Caring for At-Risk Patients Can Impact Your Bottom Line (Medicomp Systems)
- How Southern Ohio Medical Center uses Meditech Expanse Toolkits to provide safe, high-quality care (Meditech)
- How to Market Your PT Practice Offline (MWTherapy)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.

































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…