Stephen Hau, MS is chairman and CEO of Newfire Global Partners of Cambridge, MA.

Tell me about yourself and the company.
I’m a serial entrepreneur and an experienced company operator. Much of my misspent youth was dedicated to building companies and bringing innovation into the marketplace. Today, at nearly 50, I’m the CEO and chairman of Newfire Global Partners, a company that, you guessed it, helps clients build companies and bring innovation to the marketplace.
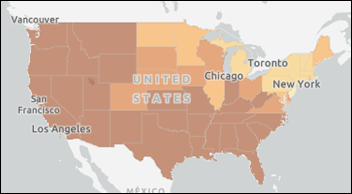
Newfire is headquartered in Cambridge, Massachusetts, with nearly 400 team members worldwide in Europe, the Americas, and Asia. Our services include advisory work, staff augmentation, managed services, pivots and turnarounds, and de novo starts. About 80% of our business is in healthcare, spanning provider, payer, consumer, and life sciences. Much of our work includes elements of data engineering, data science, and replatforming. We are expanding our US footprint, opening an office in Canada, and exploring operations in Singapore to support our global supply chain of the best talent. We envision having thousands of team members within the next three years.
What are the challenges and benefits of operating in several countries?
When we started the company, it was quite organic. A company that I was associated with was getting acquired. The acquiring company, which was much larger, decided to release the engineers, who were in Eastern Europe. They were great engineers, so I sent out 50 job offers, and about 35 of them stayed. I just thought they were great engineers. I didn’t even have work for them, but I have lots of friends who are venture capitalists, private equity people, and CEOs who run technology companies, so we just did some matchmaking.
Over the course of the last few years, it’s grown from 35 to now nearly 400 people. We’ve chosen our locations strategically. I like certain profiles in Eastern Europe, especially in areas around data science and engineering. We have dual offices in Ukraine and Croatia. We have an office in Costa Rica and of course we operate in the United States. We have an office in Kuala Lumpur, Malaysia, and we’re probably opening an office in Singapore. Having these locations also provides redundancy. For a lot of our customers, I represent a key part of their supply chain, so we have gone to great lengths to protect that pipeline chain to have as much diversity as possible.
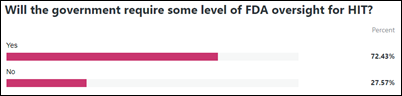
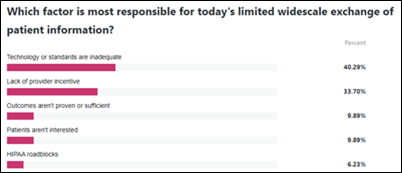
How are digital health companies working around any limitations they find in interoperability and data maturity?
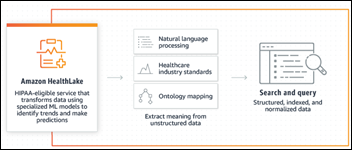
Our customers represent a subset of the market, but if I generalize from my personal experiences, interoperability is key. New companies in this space discover the challenge pretty quickly. More experienced folks appreciate that it’s just part of the cost of doing business in this space. The good news is that maturity of tools and options exists. FHIR is not yet a perfect solution, but it has given a lot of technological optionality and advantage to digital health companies, especially new entrants.
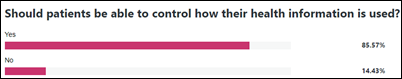
In terms of data maturity, that is a common theme that we see across clients that we work with. A common theme in healthcare is data, data, data. People incorporate data as their primary strategy, or they may be a company that has been operating for a while and see data as a new opportunity. In both situations, there is a challenge of data maturity and sometimes what I call data liquidity, which is having data in computable form that can be used to fuel things like predictive analytics and machine learning and so forth.
For data maturity, there are many elements to support clients. Some of it includes things that are not particularly glamorous, such as data cleansing, which quite frankly is extremely manual. What a lot of people don’t realize is that in this vision of a data-driven future, there is a lot of behind the scenes work that requires a fair amount of manpower.
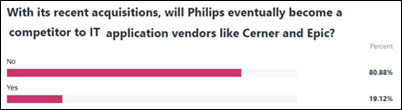
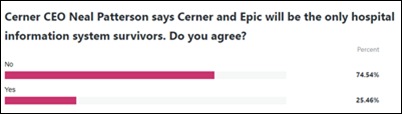
How do you see the ecosystem shaping up between big EHR vendors like Cerner and Epic and all those well-funded startups?
It’s an interesting dynamic for sure. It’s hard to predict how the future will play out. Obviously the existing EHRs have tremendous market share and there is a high switching cost to convert to something that is maybe more modern or innovative. Obviously it is difficult to innovate when you have so much installed base. Those are all challenges.
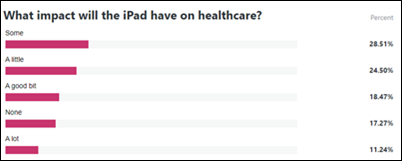
Some exciting new capabilities are being developed by new entrants into the market, companies that may only be four or five years old. Some of the tools can be tremendously helpful to the healthcare ecosystem and ultimately drive impressive outcomes to help patients and consumers. I’m a free market guy, so my hope is that the duality can coexist. The market will adjust to allow the innovative technology to be utilized and incorporated by the existing players.
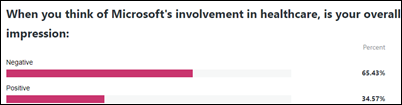
What influence do you see coming from big technology companies like Microsoft and Google, whose healthcare involvement seems to come and go?
These big horizontal players historically have come in, they’ve left, and sometimes they come back again. That highlights or spotlights the unique aspects of the healthcare ecosystem. In our own journey, we’ve seen the market from the provider perspective and the payer perspective. In some ways, they are two sides of the same coin of some of the problems that they’re trying to address. On the provider side, they think in terms of prior authorization, while on the payer side, they’re thinking in terms of utilization management.
This is an example of why it’s so difficult for a horizontal to come in and to think that there’s a “one size fits all.” These large players obviously bring tremendous resources and pretty cool innovation. But the reality is that it has to be focused on specific, achievable, valuable problems in our market to be relevant, then move the needle in a way that it can provide lasting value and then become a longstanding player in this space.
What are the keys to success for new health IT entrants?
I’m a believer that the investment fuels innovation. Obviously I’ve been a beneficiary of venture capital in my career. Where we are now comes down to outcomes. We gave a lot of new ideas and a lot of old ideas being reapplied. At this point, there is a real focus on what actually moves the needle. One example is that, over the last 10 or 15 years, we have seen a rise in consumerism, and that has led to many cool opportunities. We have seen a class of wellness applications or applications that allow consumers to support their own health. We have seen some great examples of companies that have made a positive impact.
The focus now is that people are shifting from acknowledgement of great ideas to whether they ultimately translate to improved patient outcomes. That will ultimately be a filter for many companies in the market to decide which companies survive and continue and which ones do not.
What does it feel like to see PatientKeeper still going strong 25 years after you founded it?
I started PatientKeeper in 1996 with Joe Bonventre, MD, PhD, a professor at Harvard Medical School. I started Shareable Ink 2008 with Vernon Huang, MD, who’s a former medical director at Apple. Both of my co-founders are physicians. Our teams did some amazing work and we had some fun. But at the same time, it’s a little bittersweet for me because I never got to use the products that we worked so hard to build because I’m not a clinician. I’m sure many of your readers can relate to that.
In contrast, what’s exciting about Newfire is that I have been a consumer of the services we provide. Our product is extremely relatable to me, which gives me an advantage in terms of how we support our customers.
What’s in the future for the company?
We are in a golden age for technology in healthcare. I have a privileged vantage point because I’ve gotten to work for the leaders — providers, payers, consumer, and life sciences. We are seeing some real opportunities for meaningful innovation. It is inspiring to watch the management teams of these companies turn ambition to reality. My hope for Newfire is that we will continue to be a trusted partner for our clients that supports them in their journey to bring innovation into the marketplace.






















































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…