News 10/6/21
Top News
Quality measurement and clinical intelligence platform vendor Apervita shuts down.
Chief Informatics and Innovation Officer Blackford Middleton, MD, MPH, MSc said in a LinkedIn post that the company was unable to complete a second funding round. It had raised $60 million since December 2012 through a Series A.
Apervita sold its value optimization business to Clarify Health in August 2021.
Reader Comments
From Executive Channel: “Re: females as VPs of HR, legal, and marketing. We would likely see the same phenomenon in IT if technology jobs weren’t dominated by men.” Health system support departments such as IT don’t contribute directly to profit and loss except as a cost center, which is why executives of those areas aren’t usually seen as prime candidates for broader roles in areas that have dozens or hundreds of insiders who are ready to move up the ladder. Most of the big bumps in CIO compensation and job responsibility over the years came from consolidation into ever-larger health systems and horizontal expansion of CIO responsibility in taking over other support departments such as biomedical engineering, telecommunications, informatics, analytics, and quality reporting (headcount and budget responsibility drive pay in health systems). The few former CIOs who are now COOs or CEOs of large health systems gained experience in other positions, which I would anecdotally observe usually involved only a short stay in IT as part of being moved around for executive grooming — a long stint as a CIO in a single health system likely means you’ve topped out there. It’s not quite the same in vendorland, where CTOs of tech-heavy startups are often co-founders in companies where technology is a core competency rather than a supporting function.
HIStalk Announcements and Requests
Welcome to new HIStalk Platinum Sponsor Interbit Data. The Natick, MA-based company’s software automation solutions ensure that clinicians and hospital staff have easy, secure, and reliable access to patient and financial information so they can get back to quality patient care and stay in touch. Its products integrate with any HCIS platform to distribute reports that help care teams stay informed. It is the pioneer and best-practice leader in downtime business continuity, providing reliable access to patient information at the point-of-care during downtimes, as well as during more challenging cyber crises. Using its software automation solutions, hospitals can be more efficient, streamline workflows, and improve overall patient care and safety. It provides secure, reliable, and cost-effective solutions that help 800 healthcare facility customers worldwide remain connected. Thanks to Interbit Data for supporting HIStalk.
I found this explainer video for Interbit Data’s NetDelivery on YouTube.
Webinars
October 6 (Wednesday) 2 ET. “Solving Patient Experience Challenges Through a Strong Digital Front Door.” Sponsor: Avtex. Presenters: Mike Pietig, VP of healthcare experience, Avtex; Jamey Shiels, MBA, VP of consumer experience, Advocate Aurora Health; Chad Thorpe, care ambassador, DispatchHealth. Patients expect healthcare providers to offer them the same digital experience they get when banking, shopping, and traveling. This webinar will describe how two leading healthcare providers created digital front doors that exceed patient expectations, improve patient outcomes, drive loyalty and acquisition, and future-proof their growth strategies in competitive markets.
October 6 (Wednesday) 1 ET. “A New, Streamlined Approach to Documentation and Problem List Management in Cerner Millennium.” Sponsor: Intelligent Medical Objects. Presenters: Deepak Pillai, MD, physician informaticist, IMO; David Arco, product manager, IMO; Nicole Douglas, senior product marketing manager, IMO. The IMO Core CSmart app, which is available for Cerner Millennium in the Cerner code App Gallery, helps providers document with specificity, make problem lists more meaningful, and improve HCC coding. This webinar will review the challenges and bottlenecks of clinical documentation and problem list management and discuss how streamlined workflows within Cerner Millennium can help reduce clinician HIT burden.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

ManpowerGroup finalizes its acquisition of IT staffing and services provider Ettain Group, which acquired Leidos Health in 2019. Ettain will merge with ManpowerGroup’s Experis IT talent and solutions business and will operate under the Experis name.
Sales
- Cancer Treatment Centers of America will implement Lyniate’s Corepoint interoperability platform.
- Rochester RHIO selects Direct Secure Messaging capabilities from Secure Exchange Solutions.
People

Commure promotes Ashwini Zenooz, MD to CEO. She replaces industry long-timer Brent Dover, who will remain as an advisor.

Michael Wagner, MSA (MPRO) joins Honor Community Health as CIO.

QS Systems hires Kendall Stanley (Inovalon) as VP of sales and marketing.


Radiology Partners promotes Jennifer Beaumont to SVP of regional support services and clinical practice integration (she was SVP of IT) and hires Mark Logan (IBM Watson Health) as SVP of IT clinical technologies.

Patient and employee experience platform vendor Qualtrics hires Adrienne Boissy, MD (Cleveland Clinic) as its first chief medical officer.
Announcements and Implementations
Central Logic renames itself to About as it integrates recent acquisitions Ensocare (inpatient referral to post-acute care) and Acuity Link (transportation communications and logistics management).
Privia Health implements Kyruus ProviderMatch to enable patients to find and book appointments with physicians.

Sparrow Health (MI) adds a proof of COVID-19 vaccination feature developed by Epic to its MySparrow patient app. It enables users to display a QR code, download a PDF, or export verification to a health wallet.

Intermountain Healthcare, Presbyterian Healthcare Services, and SSM Health form Graphite Health, a nonprofit that will help member organizations vet, access, and implement digital health solutions.

Microsoft releases Windows 11 as a free upgrade for eligible Windows 10 PCs and on new PCs that have it pre-installed. My two-year-old laptop passed Microsoft’s Windows 11 readiness test, so I’ll give it a few weeks and then upgrade.

New Cerner President and CEO David Feinberg, MD, MBA will kick off the two-day virtual Cerner Health Conference 2021 next week.
Mackinac Straits Health System will affiliate with MidMichigan Health to address its IT needs and to implement Epic.
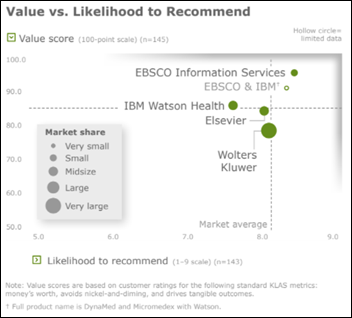
A new KLAS report on point-of-care references for clinical decision support finds that market share leader Wolters Kluwer is loved by physicians who learned to rely on UpToDate in medical school, but health systems say it’s the most expensive of available solutions and they sometimes switch to a cheaper alternative. Users of IBM Watson Health, especially pharmacists, like its NLP search feature even though the company scores poorly in customer support. Elsevier and IBM Watson Health both suffer from content delivery that can run months behind, users report. Ebsco earns the highest overall score with deep content at a fraction of the price of competitors.
Privacy and Security
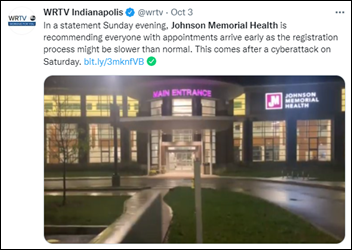
In Indiana, Johnson Memorial Health and Schneck Medical Center recover from apparently unrelated cyberattacks that forced the organizations to take their IT systems offline.
Other
Business Insider looks at problems in Apple’s healthcare organization, most of which have been described previously:
- Employees say people were disciplined for disagreeing with their bosses over the way health data is being used to develop products and the questionable quality of that data.
- The company expected the Apple Watch to spawn a subscription-based health program in which consumer data would be shared with their physicians, but the engineers who developed Watch designed its features for consumers rather than patients who are seeking medical care. The Watch can identify conditions, but isn’t as strong at measuring them.
- Apple uses its AC Wellness employee clinic as a healthcare workshop, but the company is questioning its cost compared to similar programs such as that of Crossover Health.
- Apple has talked to health plans about selling its HealthHabit app that allows its employees to track fitness goals and blood pressure, but poor user engagement has caused Apple cut back on the project roadmap and to reassign its employees.
Steve Jobs died 10 years ago at 56, having kicked a dent in the universe that outlives him.
Sponsor Updates
- Availity integrates TruthMD’s MedFax healthcare data solutions with its initiatives for provider data management.
- Olive will hire an additional 300 employees by the end of this year, increasing its employee base by 30%.
- Wolters Kluwer Health CEO Stacey Caywood earns a Bronze Stevie Award in the category of Female Executive of the Year – Business Products.
- EClinicalWorks publishes a new customer success story, “Using Prisma to Help Staff and Close Care Gaps at Centerpoint Health.”
- CareSignal has partnered with Innovaccer to offer deviceless remote-patient monitoring to organizations and payers participating in value-based care on the Innovaccer Health Cloud.
- Change Healthcare will host its 2021 Virtual Innovation Summit October 12-13.
- CHIME releases a new Digital Health Leaders Podcast, “A Conversation with Sarah Richardson, FCHIME, CHCIO, SVP and CIO, Tivity Health.”
- Clearwater expands its customer training content and security awareness capabilities through a new partnership with cybersecurity education company Infosec.
- CloudWave publishes a new whitepaper, “Enterprise Imaging in the Cloud.”
- CoverMyMeds will present at Epic’s App Orchard Conference October 6.
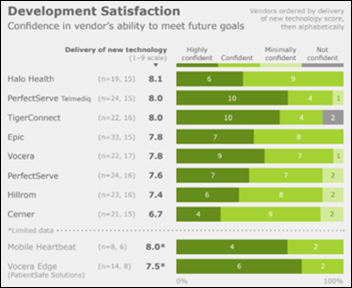
- A new KLAS report, “Clinical Communication Platforms 2021,” recognizes Vocera as a top-rated vendor in health systems with enterprise-wide deployments.
- Diameter Health Chief Architect Sam Schifman will present at the John Snow Labs NLP Summit October 6.
- Engage publishes a new case study, “From Chaos to Control: How Exeter Hospital Addressed Their Disaster Recovery Challenges.”
- EClinicalWorks will host its national conference virtually October 7-8.
- EZDI wins at the HIC2 in India for the use case “Digital Clinical Assistant for Integrating with Legacy EHR.”
HIStalk sponsors named top-ranking outsourcing vendors in 2021, according to Black Book Research’s latest survey, include:
- Credentialing & Privileging – Symplr/TractManager
- Cybersecurity – Fortified Health Security
- Database Support & Analytics – Health Catalyst
- ERP Support – Pivot Point Consulting
- IT Tech Support – Cerner
- Medical Imaging Systems – Agfa HealthCare
Blog Posts
- How to Get Your SNF Survey-Ready (Ability Network)
- Five Technology Disruptions in Healthcare That Will Stock Post-Pandemic (Ascom)
- After 20 years, one thing stands out. It’s all about multi-payer collaboration. (Availity)
- How Healthcare Organizations are Implementing Innovative Virtual-first Care Models (Bluestream)
- Digital Transformation Starts with Data (CereCore)
- 5 healthcare trends rounding out 2021 (Cerner)
- Solving Healthcare Business Challenges with New Service Models: A Thought Leadership Roundtable (CHIME)
- Highlights from the DIUC21 Keynote (Dimensional Insight)
- Post-Acute 2.0: New Services Needed to Deliver Care at Home (Dina)
- How providers can streamline care to prepare for a “twindemic” of COVID-19 and flu (Experian Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.


































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…