News 12/1/21
Top News

Greenway Health promotes President Pratap Sarker, MBA to CEO, effective January 1.
Sarker replaces Richard Atkin, who will take on the role of executive chairman.
Reader Comments
From Orion’s Roar: “Re: LinkedIn. A telehealth company sent me an invitation to become a strategic advisor, based purely on my profile. They offered the chance to buy shares, get stock options, and earn a percentage of revenue from B2B sales that I would help them earn. I’m sure they could find better advisors and this is just clever bait for investing in their company.” I see nothing impressive about the company (I’m omitting its name), which seems to be selling shares rather than product and recruiting sales affiliates rather than advisors.
From DeeDee Centralized: “Re: closing the IT department. Is WSJ right?” The IT pendulum is always swinging from “let departments do their own IT work with their own people and budgets” to “we have to regain control of rogue departments whose mini-IT fiefdoms are spending even more money with less accountability and measurable corporate benefit.” Everybody is an IT expert until their cool tech stuff breaks or screws up a downstream department that they failed to consider in their on-the-fly design. The answer is always a less-dramatic compromise that won’t make management professors famous – centralize the technology rule-making to avoid an unreliable hodgepodge of faddish technologies, oversee the IT spend both centralized and decentralized so it can be understood and optimally deployed (in hospitals, failure to do this means the well-connected finance and patient accounting departments get about 70% of the total budget), and embed IT people on the front lines and vice versa to make sure everybody understands the current and desired future state. People who write “first kill all the IT people” articles are no different than those who can’t decide if outsourcing is brilliant or stupid — they just take the opposite position every few years to get press as contrarians despite having no experience running the organizations they advise.
HIStalk Announcements and Requests
Thanks to ConnectiveRx for upgrading their HIStalk sponsorship to Platinum. They have supported HIStalk since 2012.
My Bitdefender Total Security 5-Device subscription was set to auto-renew at $90 for one year. As always, I cancelled the auto-renewal and found a better deal, in this case $30 for two years from Best Buy, saving me 83%. All I had to do was enter the new code into Bitdefender Central to pop the expiration date out 24 months.
I’ve decided that I’ll attend HIMSS22 after months of waffling about whether to go or not, motivated more by habit than desire or high ROI expectations. I compromised by choosing a short stay in which I’ll just go Tuesday and Wednesday.
Webinars
December 8 (Wednesday) 1 ET. “What Lies Ahead for the EHR’s Problem List.” Sponsor: Intelligent Medical Objects. Presenters: James Thompson, MD, physician informaticist, IMO; Deepak Pillai, MD, MBA, physician informaticist, IMO; Jonathan Gold, MD, MHA, MSc, physician informaticist, IMO. The EHR problem list can be cluttered with redundant, missing, and outdated diagnoses, and displays don’t always help clinicians process the available data correctly. The presenters will discuss how improvements in creating, maintaining, and displaying problems could reduce errors and decrease the cognitive load of clinicians while continuing to optimize reimbursement.
December 9 (Thursday) 1:30 ET. “Cone Health: Creating Extreme Efficiencies in Surgical Services.” Sponsor: RelayOne. Presenters: Wayne McFatter, RN, MSN and Sharon McCarter, RN co-directors of perioperative services, Cone Health. The presenters will discuss how they have empowered the entire surgical care team, including vendor representatives, to get real-time access to surgery schedules and case requirements in the palms of their hand. RelayOne CEO Cam Sexton will also present the findings of a recent study of 100 hospital leaders regarding their operating room optimization plans for 2022.
December 14 (Tuesday) 1 ET. “Using Cloud to Boost AI and Enterprise Imaging.” Sponsor: CloudWave. Presenters: Larry Sitka, MS, VP/CSIO of enterprise applications, Canon Medical Informatics; Jacob Wheeler, MBA, senior product manager, CloudWave. Enterprise imaging has remained a holdout of data center complexity despite the benefits the cloud offers. The presenters will discuss innovative ways to reduce complexity and lead with disruptive technology using AI, enterprise imaging, and the cloud.
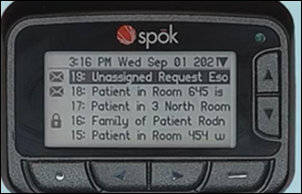
December 15 (Wednesday) 1 ET. “Improve Efficiency, Reduce Burnout: Leveraging Smart Clinical Communications.” Sponsor: Spok. Presenters: Matt Mesnik, MD, chief medical officer, Spok; Kiley Black, MSN, APRN, director of clinical innovation, Spok. The presenters will identify the most common clinical technology contributors to alarm fatigue and clinician burnout. They will describe how improving three clinical workflows can increase care team collaboration and reduce non-patient care workload and explain how a clinical communication platform simplifies finding care team members and pulling actionable information from the EHR.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Elsevier acquires digital healthcare educational content company Osmosis, which it will add to its Global Medical Education portfolio.
Analytics and data integration vendor Innovar Healthcare is among several companies that are purchasing the liquidated assets of Bridge Connector, a Nashville-based data migration startup that closed last year. The company, which had raised over $25 million several months before going out of business, and owes its creditors $5.4 million.
Babyscripts increases its previously announced Series B funding round with an additional $7.5 million investment. The virtual maternity care company has raised $37 million since launching in 2013.
Clinical task management software vendor CareAlign raises $2.3 million in seed funding. Former Penn Medicine associate CMIO Subha Airan-Javia, MD created the company in 2014, spinning it out of Penn five years later.
Sales
- UAB Medicine selects specialty pharmacy-focused analytics and data integration services from Loopback Analytics.
- Elsevier integrates Nuance’s PowerScribe radiology reporting software with its STATDx diagnostic decision support tool for radiologists.
- Phoebe Putney Health System (GA) will implement Wolters Kluwer Health’s POC Advisor for sepsis detection and patient management at three hospitals.
Announcements and Implementations

Nuance announces GA of its new Precision Imaging Network, cloud-based technology that transmits AI-generated data and analytics from diagnostic imaging systems to existing clinical and administrative workflows.
UC Davis Health (CA) and Amazon Web Services launch a Cloud Innovation Center that will focus on developing digital health solutions that are accessible and equitable.

Teleradiology service StatRad implements Change Healthcare’s cloud-based Stratus Imaging PACS.
Edifecs announces implementation of a work model that allows most of its employees to work from wherever they think they are the most productive – home, office, or a combination – while allowing them to reduce commuting stress and run personal errands.
Per-diem nurse staffing platform vendor IntelyCare launches a credentialing passport for uploading and providing licenses, screening test results, certifications, and employment eligibility verification.
NextGen Healthcare launches a benchmarking and analytics service for Community Health Centers.
Government and Politics
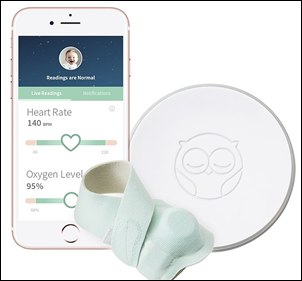
FDA forces Owlet to stop selling its smart baby monitoring socks that track vital signs and sleep patterns until it earns FDA approval. FDA did not require the company to recall the 1 million sock it has sold over the past six years. Owlet says it will soon launch a new sleep monitoring solution.
The VA awards a five-year, $65 million contract to Caregility, ThunderCat Technology, Sterling Heritage, and Iron Bow Healthcare for remote patient monitoring software and services that it will roll out through its TeleCare Companion Patient Observation Support and Services Program.
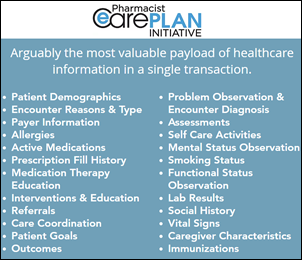
The Pharmacy HIT Collaborative meets with ONC and pharmacy system vendors about pharmacy interoperability, including integrating the information in the Pharmacists ECare Plan with provider EHRs and payer systems, as required by the Cures Act.
HHS OCR settles with five providers that failed to give patients timely access to their records at a reasonable cost under the HIPAA Privacy Rule, with settlement costs ranging from $10,000 to $160,000. A cardiovascular disease doctor who ignored a patient’s request for a copy of their medical record and then ignored OCR investigators waived his right to a hearing in paying $100,000.
Other
Business Insider asks eight big health systems to describe the most interesting tech project they are testing (and in some cases, also investing in):
- Northwell Health: AI analysis of EHR data to identify pregnant women who are at risk for pre-eclampsia.
- New York – Presbyterian: EHR triggers to make sure orders are completed that would otherwise prevent a patient from being discharged as planned.
- Cleveland Clinic: optimize use of unnecessary lab tests and supplies based on historical patient data.
- Providence: allow behavioral health referrals to be ordered during primary care visits.
- LifePoint Health: remote patient monitoring.
- CommonSpirit: open a bricks-and-mortar women’s and reproductive clinic with telehealth startup Tia.
- Universal Health Services: notify providers of patient health or admission status using EHR data sent to a homegrown app.
- UPMC: remote patient monitoring.
Sponsor Updates
- The Rotherham NHS Foundation Trust and Agfa HealthCare celebrate Enterprise Imaging’s 34th UK go-live.
- PRWeek highlights Actium Health’s role in helping Virtua’s marketing team launch a campaign that successfully encouraged patients to come in for missed screenings.
- Intelerad launches a cloud-native disaster recovery solution.
- Cerner staff assemble 200 meal baskets for veterans and families supported by Veterans Community Project and Jackson County Family Court Services.
- Netsmart partners with the National Council for Mental Wellbeing to improve care coordination and use data to drive outcomes for certified community behavioral health clinics.
- A public regional hospital group in Italy will implement Ascom’s Digistat software in several of its facilities.
Blog Posts
- Vendor HIPAA Breach Affects 319K Patients & Their Providers (AdvancedMD)
- The Glidepath to Downside Risk: Future-Proof You Healthcare Business Through Value-Based Care (Arcadia)
- Embracing Interoperability with FHIR (Availity)
- Interoperability is Key to Care Coordination (Bamboo Health)
- The Path to Meditech Expanse: Where Should You Begin? (CereCore)
- Optimize Star Ratings in the Medicare Advantage Market: 3 Strategies for Payers (Collective Medical)
- Five powerful COVID-related shifts in patient care (ConnectiveRx)
- Driving Health Care 4.0 (Diameter Health)
- The Shift to Care-at-Home: Are You Ready? Why You Need to Be (Dina)
- The Future is Online Appointment Scheduling (EClinicalWorks)
- What does the connected generation (Gen C) expect from providers? (Experian Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.





















Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…