HIStalk Interviews Patty Hayward, VP, Talkdesk
Patty Hayward, MA is VP of strategy, healthcare and life sciences, of Talkdesk of San Francisco, CA.
Tell me about yourself and the company.
I’ve been in healthcare IT for the past 25 years. I’ve worked with several organizations to transform processes and procedures in areas such as medication safety and revenue cycle. I worked at Aetna, helping with the first ACOs. I’ve had a lot of stints in population health. Now I’m working with patient experience.
Talkdesk has been around for 10 years. It offers the first cloud-native contact center as a service. It was born out of a hackathon from Twilio. There was a niche in the market that needed to be worked on. The company has kept over 50% of its employees based in product and R&D, which is a huge commitment to innovation, looking at how we can transform and disrupt different areas.
About a year and a half ago, the decision was made to look at specific verticals, with healthcare being the first. That’s when they brought me and other folks on board. For us, it’s all about how to reimagine that patient experience, reduce friction, and help providers offer a different experience than is typical. We want to make sure that it is synchronized across multiple channels and is personalized and convenient.
How do large health systems tailor their digital health strategies in the face of potential competition, but while operating at capacity and with record profits?
Interesting and unique forces are definitely in play. There’s a lot of change in the market. Large retailers are jumping into the market, bringing their experiences to target areas such as primary care, population health, and chronic disease management. That’s going to give them a lot of ability to steer. Whoever you’re dealing with most — your primary care doc or someone who is working with you to manage your chronic disease — is who you will listen to on where you go. Younger generations are interested in different ways of doing business and thinking about healthcare in a different way. Record profits make it attractive for people to jump in, and you are seeing that.
Amazon has the luxury of catering to a self-selected customer base that is comfortable with an online-only relationship. Do providers have a different challenge in accommodating people who may prefer interacting in person or via telephone?
You are seeing this a lot with Medicare Advantage plans. They are obviously targeting the senior population, but they are tech savvy and tech forward in their approach and are using it in a smart way. They are giving a lot of choice and a lot of opportunity to utilize technology selectively, but also using care guides to guide folks through the system, which is much needed when you think about chronic disease patients in the Medicare population. It is difficult to navigate. They are allowing their members to come to them as they can, or as they would like to, whether that’s via voice or via technology. They are also using technology to make their agents efficient. So there are multiple ways to look at technology and how to implement it. It doesn’t have to be patient- or member-facing.
How are health systems using their contact centers differently?
Health systems are starting to look at their contact center as a strategic asset versus just the cost center it was in the past. It is the front door, typically the first touch that a patient has with their organization. We went the NGPX patient experience conference at the beginning of December and one of the things that struck me was that about 95% of the presentations were on HCAHPS scores. Those are acute focused, inside, did we do these certain things. When I had conversations with a lot of folks, the Mayo of course jumped out and started talking about patient experience in a very different way. They still do HCAHPS, because you have to, but they have jumped over to using Net Promoter Score as a measure of patient satisfaction. That’s unusual in the space.
People are starting to think differently about how they can transform to “how did we make you feel” versus “did we do the right things all the time.” A lot of forward-thinking folks are looking at how to do this differently. You are also seeing CMS start to push member experience as a huge piece of how they reimburse, making that one of the biggest metrics that they are using for star rating.
Providers used then-modern technology such as PBX systems or online contact forms to prevent people who needed help from easily accessing their employees. How are they thinking differently about tailoring communications using someone’s preferred method and personalizing the message?
People are talking about things like digital front door. Health systems, especially those that take risk or have their own plans, want more interaction with their patients in the right way. Being able to do things like send a text reminder that is interactive versus “say yes to confirm or no to cancel.” They want to keep that revenue stream going, because if you miss an appointment, that’s money out the door. They want to continue to have those record profits. There are a lot of ways that you can work through that whole aspect.
During COVID, the volumes that hit their switchboards were unmanageable. I talked to several health systems whose entire phone systems were taken down by the volume. People quickly automated as much as possible, standing up IVRs to give automated answers to quick questions, offering chats, and adding FAQs to their websites. Taking simple things that could be easily answered by automation off their switchboards to give their agents time to answer questions and have good interactions.
Forward-thinking ones are looking at the disruptors that are coming into the space and taking patients off of their books. How can we keep up with them? Amazon Care is going after employers, not necessarily patients themselves. Hilton was their first big one. There’s some big innovation in not only the care that is given, but in how they get patients on their rosters.
Most businesses assign a single customer identity and a defined way to interact with them. How well do health systems coordinate the many reasons they might be communicating with someone – clinical care, marketing, reminders, population health, billing – and give their employees a single view into every one of those communications?
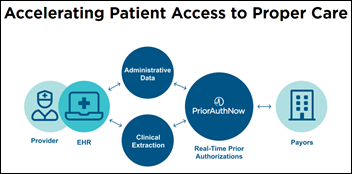
The key is integrating with the system of record. If it’s the EHR, you want to make sure that you’ve got a connection to make the API callout so you can see snippets. You aren’t trying to duplicate the EHR – you want the highlights of things that are of interest. We are completely customizable, so we can build that to the experience that you would like. You may have different groups that need different visions. Someone who is in revenue cycle and billing wants a different look than those who work in patient access or care management.
You would want to be able to see if they started it off with a chat. You would authenticate to have a real conversation, be able to see who they are, and be able to do things like patient scheduling. Then if it is escalated, to be able to bring all of that information to that agent’s workspace so that they can see what’s happening and they don’t have to listen all over again. You see that in other verticals, where when people call in, they start with a discussion with an AI agent and then escalate to a human who says, “Give me a minute to get caught up on what you’ve said.” That’s an important aspect that we don’t tend to have in healthcare as much. It’s important to have that integration into the EHR.
Patient portals used to be viewed as consumer-unfriendly, but suddenly they are the well-received launching point for most interactions with patients. How do they fit into the ideal consumer experience?
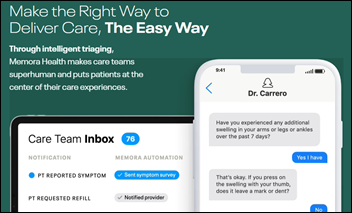
Patient portals are not going to be real time. I just had my annual physical and it took a week to get a response from my physician. The patient portal can automate things that make sense for patients to do when they are on their computer, such as scheduling appointments, rescheduling, paying their bill, things like that. But a lot of times, people are on their smartphone and want to be able to start a conversation using the chatbot in the corner of the web page.
Ideally, it’s all tied together and you can see the history. If there’s an interaction that’s recent, you want to be able to pull that in, create intents, and use AI to determine that the person is calling in because they’ve asked their question three times. You should see that as you’re answering the phone call. It’s important to be able to synchronize all these things, which typically doesn’t happen today. You call in and they have no vision into what you’ve been doing. I’ve been with my primary care provider for 19 years and it’s like I’m brand new every time I call.
Providers used to just hang out a shingle and people lined up, so nobody worked too hard to attract new patients. How are chief digital officers or chief experience officers who come in from other industries working with health systems who aren’t used to having to be consumer-friendly?
They are bringing in all sorts of people for these roles. It’s not just folks who are traditional healthcare. You have people coming in from Disney, Best Buy, the retail sector, and the entertainment sector with a viewpoint of what it could look like. They are bringing a different and unique lens to how you can capture more of the populations and become a destination place where people want to go. Mayo Clinic can dictate the kind of patients it wants, and other systems are, like you said, taking the approach that their shingle is out and people are coming.
Disruptors that are coming into the space are going to peel off those more valuable individuals, those who have more money to spend, and offer additional services that they are willing to pay for. If you look at that Amazon Care video, it’s pretty cool to be able to have a virtual visit, and if they can’t solve it on videoconference, they will send someone to your house or your place of work and then deliver your medications in two hours. There’s this full circle of care that can happen that makes it convenient and easy for you to seek the care you need.
Otherwise, folks will avoid doing that and then end up in a worse position or in the ER, which may be profitable if the ER isn’t taking risk. But if they are taking risk, all of a sudden the cost situation flips. That’s where the change is. Fee-for-service loves that ED visit, but with fee-for-value where you take on risk of the population, it’s a different discussion. We are seeing a lot of push towards fee-for-value. It has been going on for over a decade, but we are seeing more folks jumping in and offering different opportunities to grab onto that fee-for-value area and show value back to the government or to employers who are paying the bill.
What developments will we see with the company and industry in the next few years?
You will see AI take a bigger role, both in the things that are easy to automate and those that are not. It will take a huge role in helping the agents with their work, so that information is easily accessible and correct so that you can get it done quickly the first time. Agents will be able to spend more time and emphasis on that empathetic journey that you would like to show to your patients, at least those organizations that do it well.
You’re going to see a lot more emphasis on providing what in retail they call a delightful journey. Not too many people would call healthcare’s journey delightful. You typically come there stressed out and having a lot of interactions, so being able to deliver an experience like that is important. As we get folks to take care of themselves in the way that is prescribed, how do we activate the patient? How do we get them to think about how to take care of themselves and make the right choices? All of that will start to come together. Smart watches, devices, and different areas will allow you to get a lot more help and a lot more ability to, when you want, get guidance in real time.






























I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…