News 3/30/22
Top News
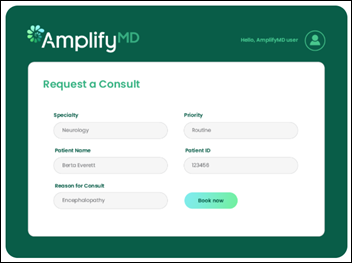
AmplifyMD, which connects hospitals to specialists via telemedicine, raises $23 million in a Series A funding round. The San Francisco-based startup’s software also incorporates care management, billing, and analytics.
Webinars
April 6 (Wednesday) 1 ET. “19 Massive Best Practices We’ve Learned from 4 Million Telehealth Visits.” Sponsor: Mend. Presenter: Matt McBride, MBA, founder, president, and CEO, Mend. Virtual visits have graduated from a quickly implemented technical novelty to a key healthcare strategy. The challenge now is to define how telehealth can work seamlessly with in-person visits. This webinar will address patient satisfaction, reducing no-show rates to single digits, and using technology to make telehealth easy to use and accessible for all patients. The presenter will share best practices that have been gleaned from millions of telehealth visits and how they have been incorporated into a leading telemedicine and AI-powered patient engagement platform.
On demand: “Cybersecurity Threats Facing Healthcare Today.” Sponsor: Net Health. Presenters: Jason James, MS, CIO, Net Health; Monique Hart, MBA, CISO, Piedmont Healthcare; Jeffrey Rosenthal, , MBA CIO, Reliant Rehabilitation; David Jollow, MBA, CISO, Healogics. The panel of CIO and CISO leaders will discuss the cyberthreats that healthcare faces today. They will review security priorities for the increasingly complex healthcare IT environment that includes cloud-based applications, an increased number of endpoints that include connected devices and patient wearables, and patient portals.
Previous webinars are on our YouTube channel. Contact Lorre to present your own
Acquisitions, Funding, Business, and Stock
![]()
RCM software vendor NThrive will change its name to FinThrive. The company acquired TransUnion Healthcare late last year for $1.7 billion, and is in the process of purchasing Pelitas, which specializes in patient access, intake, and RCM software.
Change Healthcare will reportedly sell its ClaimsXten claims payment and editing software business to Availity as potential acquirer UnitedHealth tries to work through DoJ antitrust concerns. Legal experts suggest the sale of ClaimsXten may weaken the DoJ’s lawsuit against the proposed sale of Change to UnitedHealth. The companies have until April 5 to walk away from the $8 billion deal.
Novant Health (NC) launches Novant Health Enterprises, an independent business focused on developing, acquiring, and scaling clinical, financial, and patient-oriented solutions.
Cardiologist John Spertus, MD files a copyright infringement lawsuit against Epic claiming that it has made some of his diagnostic questionnaires available in its EHR. Spertus is the director of health outcomes research at Saint Luke’s Mid America Heart Institute in Kansas City, MO.
Sales
- In Ireland, Mater Private Network will implement Meditech Expanse across its hospitals and clinics.
- Digital home care company Vesta Healthcare selects Bluestream Health’s virtual care platform-as-a-service.
People
David Garets, whose long health IT career included leadership roles with Gartner and HIMSS Analytics, died Monday at 73.

Inderpal Kohli (Hospital for Special Surgery) joins Englewood Health (NJ) as VP of IT and CIO.
Other

A local website’s profile of Epic Systems hints at a forthcoming app that will enable physicians to research best patient care practices using real-world evidence culled from the company’s Cosmos dataset, and outlines the company’s plans to continue expanding its 1,100 acre campus in Verona, WI. It opened its new 350-office Mystery building last week, and will open a similar building, dubbed Castaway, later this year. Three more additions will open within the next five years.
Vanderbilt University Medical Center’s Clickbusters program has helped reduce alert fatigue through a six-month review process that has modified 42 clinical decision support alerts and turned off 10. Eighty-four alerts were reviewed by physicians, nurses, and pharmacists, ultimately resulting in 71,227 fewer interruptive alerts being sent per week, and a 15% reduction in total interruptive alerts.
Sponsor Updates

- The Ascom marketing team has worked with Habitat for Humanity to paint two houses in Cary, NC.
- Healthcare IT Leaders publishes a new managed services case study featuring Northeast Georgia Health System.
- AdvancedMD awards Client Support Specialist Hannah Dixon an FIT Award.
- Arcadia publishes a new case study, “How Summit Health’s transitional care management creates value for patients and practices across multiple payment models.”
- Baker Tilly will present at the Pennsylvania Association of Directors of Nursing Administration Convention March 29-April 1.
- Bamboo Health will present at the Rx Drug Abuse and Heroin Summit April 19 in Atlanta.
- Dina will present at the TAG Digital Health Summit March 30 in Atlanta.
Blog Posts
- Debunking three common misconceptions about gateway edits (Availity)
- How a Virtual Care Platform as a Service enables better care (Bluestream Health)
- What orthopaedic surgeons need to know about surprise billing legislation (Bravado Health)
- Unleashing the Power of Communications for Healthcare (CareMesh)
- 5 Qualities That Add Value to a Managed IT Services Partner (CereCore)
- Why RHCs and FQHCs Should Care About Chronic Care Management (ChartSpan)
- 7 Things Healthcare Leaders Should Know About 405(d) HICP (Clearwater)
- It’s Time to Rethink Healthcare Data Backups (CloudWave)
- Clinical Research Study Aims to Improve Obstetric Outcomes in Uganda (Current Health)
- HIMSS22 Outlines Opportunities in Healthcare (EClinicalWorks)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.









































The New Yorker cartoon of Readers Write articles.