HIStalk Interviews Ashley Glover, CEO, WebPT
Ashley Glover, MBA is CEO of WebPT of Phoenix, AZ.

Tell me about yourself and the company.
I started this job in November 2021, so I’m a few months in. I spent the last 15 years in real estate software with a company called RealPage that is similar to WebPT, in that we wanted to be a vertical software provider providing all solutions to people who largely owned and managed department communities. We grew RealPage from about a $30 million company to about a $1.3 billion revenue company and it sold a year ago for a little over $10 billion. I was president of that company at the time.
That gave me an opportunity to look at something new, and I got very interested in WebPT’s story. WebPT is the number one provider of outpatient rehab software, covering physical therapy, occupational therapy, and speech therapy solutions. Most of our clients are in the outpatient space, although we have a large and growing business in what I would call integrated businesses, like hospital systems that have PT clinics, that sort of thing.
WebPT has a little over 800 employees and over $150 million of revenues. We recently bought Clinicient and Keet, which were also leading edge providers of similar software in our space. In the last couple of months, we’ve been integrating the companies.
What challenges of outpatient rehab therapy providers can technology address?
Two cases drive most of the reasons people go to rehab. One is that they are recovering from an incident. That could be an injury. Athletes or weekend warriors often need rehab, or they’re coming in related to surgical recovery. The other thing that drives a lot of our patients is it age-related conditions, or other health conditions that drive the need for rehab to support people’s mobility.
From a software perspective, we started out as focused on allowing the clinician to provide leading edge documentation, plan of care, and monitoring of recovery through the plan of care. Ensuring that it is compliant, a best-in-class way to document, and easy to bill. Over the last several years, we’ve added additional solutions, like billing software. That facilitates billing and collections and software that enables the front office to better serve the patient largely through digital solutions. Think digital patient intake, electronic benefit verification, and marketing type solutions that manage communications with the patient.
Is the measuring of outcomes and patient satisfaction more pure than in a health system, where the care environment is less focused?
Absolutely. It’s pure in the sense that people really do want to know that they are delivering good outcomes. One of our biggest issues is that patients drop out of therapy at three or four visits, when they might really need 12 visits. So we talk about the need for patient engagement solutions, which is to keep them engaged through the plan of care, which ensures a better outcome, and frankly measuring the outcomes themselves.
Early in our business, we bought a company and integrated it into our solution that allowed us to manage patient engagement and increase the probability that they would move through their plan of care through better engagement with them digitally. We did not own an outcomes solution, but through this acquisition with Clinicient, we have picked up an solution called Keet that a lot of our members used and that we integrated with, but now we own.
What’s great about Keet is it’s in the musculoskeletal program and it’s a Qualified Clinical Data Registry, or QCDR. That allows for the Medicare reporting, but we think there’s a broader opportunity in using it as an outcomes tool to manage quality of outcomes and promoting that use case within the businesses, because obviously not everybody’s getting Medicare. Often the payers want to know if people are receiving better outcomes as well, and Keet will facilitate that.
What are the main reasons that so many patients don’t complete their course of therapy?
There are two things that just kill us, and if we could solve for it, our clients could make a lot more money and people would have better outcomes. One is that there’s a lot of evidence that people who should get PT are not getting PT at all, or OT or speech therapy. That’s an issue with a gap with people’s awareness of how effective PT, OT, and speech therapy can be in lieu of surgery or drugs, for example. Often, it’s not the first place even a doctor will send people.
I’m a great example of this. I’ve had an autoimmune arthritic condition for years and have had the best of care. Initially, it was misdiagnosed and I was sent in for knee surgery, which turns out that didn’t fix it, and then I got put on probably a three- to four-year cycle of trying to find the right drug. We did find a really good drug, but it was only after I fell off a horse and broke six bones. I’m a horse person, and when I went into PT to deal with my horse injury, my PT told me, “By the way, I can help you with your arthritis.”
I still go to PT even though I fell off that horse almost a year and a half ago. It has wound up being more effective than all the other courses of care I’ve had. I’ve had doctors, but there’s a blind spot to it, in the patient population and medical provider population, that it can be a way to go in lieu of other options. We have an initiative we call Get PT. Our advocacy group, APTQI, is working to increase awareness of people trying PT as a solution in lieu of some other solutions.
Our second issue is that people will enter PT and not want to continue a course of care because they feel better, or it’s a hassle.
I believe, and many people in our industry believe, that the true evolving model is going to wind up as a hybrid model. It is not going to be all virtual and it’s not going to be all in-person. People are playing around with models and our software supports this, where you might have an initial in-person evaluation and maybe a couple of courses of care, then you might have the option to do home exercises or a virtual visit where that’s tracked through the application, and then come back for periodic check-ins. You’re not having to get in the car, go to the clinic, do your course for 12 sessions. Maybe you’re only doing four or five in-person, but you’re doing some virtually.
I think personally that’s the future to ensure that people stick with a course of care, because you’ve got to reduce the hassle factor and you’ve got to make every visit meaningful when they do have to come in for that in-person visit. The key to that is having software that supports the hybrid model. We have that and we think we can better enable it. The key is RTM code billability, which we’re making sure that virtual visits are billable. Then the key is also monitoring outcomes, because we need to be able to measure that the outcomes in these situations are as good or better than if people came into that in-person care.
The hottest thing years ago was companies that were using Xbox and other consumer gaming consoles to show patients how to do exercises at home and then to monitor whether they were doing them correctly. Do you still see that or other technologies, such as video, that support at-home treatments?
It’s more than video, and we are looking very hard at RTM codes right now. I’m not a lawyer and I’m less than six months into this industry, so I’m not an authority and I am consulting with outside advisors. But there are rules around what defines a medical device. Does the stuff that we are providing qualify as a medical device? We don’t want to go awry on the compliance perspective, as you can imagine.
Remote therapeutic monitoring could be a virtual visit, but it also could be something as simple as people having check-ins through software that measures their current parameters or conditions. It can literally be self-monitoring your condition, working with your provider, checking in, and providing measurements along the way. RTM can be defined in a lot of ways. Before we release anything that does this, we want to make sure that we’re doing it right and that we are supporting all the possible use cases. During COVID, virtual visits were billable, then they weren’t, and now they are saying that they are billable in some cases. This is an area where even the payer and Medicaid rules change frequently.
What does the therapy practice landscape look like? Does it have similar M&A activity that we see in hospitals and medical practices and are private equity firms involved?
There is absolutely a consolidation activity in this space, and that has been going on for a long time. We think of the industry distribution looking like a barbell. There’s a lot of small practices, then there’s quite a bit of consolidation in the top 20-to-50 providers on the larger side, and the middle market is getting smaller. The middle market is getting smaller obviously because these private equity consolidations love to buy larger 10- to 30-practice middle market providers that consolidate into their several hundred practice larger company. If you are doing a consolidation exercise, it’s easier to buy somebody who is managing 10 to 30 clinics versus one clinic.
The middle market is ripe for consolidation activity, so we’ve seen it getting smaller over the years. But there are also, and this is good, a lot of new therapists coming out into business. Many of them are starting out as solo or small group practitioners. There’s also constantly new therapists coming into market and feeding that small business side.
There’s a very large small market side, where one to five people are running a practice together, and then there’s a very large what we would call enterprise, where there’s hundreds of clinics. They’ve negotiated national deals with payers and they’re running more like you a large corporate entity. Their needs are different. In the small practice, the clinician is doing everything. They’re managing patient intake, they’re getting their insurance, they’re diagnosing them, they’re managing their course of care, and they’re billing insurance. We need to provide that all-in-one solution to them.
The larger enterprise area is more specialized. The therapist who is touching the patient isn’t having to worry about the front office activity, the billing activity, compliance, or the financials. They are focused on the course of care. But that means your software has to be able to specialize and handle all the different roles in those organizations effectively. We’ve been working to make sure our software meets the needs of both segments, but they’re very different.
What communication is involved with making and accepting a patient referral and then reporting back the therapy outcomes, especially if there’s a value-based component?
Historically, the practices would build relationships with doctors who would refer patients in for care, either surgeons or general practitioners, all the different reasons why people might come in. You build relationships. If you think about a small practice, that could be local relationships. The larger practices get, the more likely they are to build referral relationships with local hospital systems, local payers, or even unions. We’ve seen people build relationships with unions or other groups that handle populations.
The trend towards value-based care and payment on outcomes is slower in PT and OT than it has been in other industries, but we see that trend still coming. It will still come our way. The models now are more experimental, but there’s a high demand for tighter integration in the referral network for us to be able to automate the receiving of the patient referral, which even in today’s environment is largely manual intake, and automate pushing back what the plan of care is and what the outcomes are.
We are trying to drive a lot more interoperability in the industry with this two-way integration so that we can better monitor the course of care. That’s one place that we’re seeing our business grow. We’re going to continue to push is making sure that we have that tight integration with that broader ecosystem that the patient exists in. Historically, we thought of the patient only in the lens of the person who was treating them in our business, the physical therapist or the occupational therapist, for example. But increasingly we are aware that patients are actually receiving care from multiple providers and there’s a need to see how their outcomes are being managed holistically. Our goal is to support that.
What is the strategy for the company over the next 3-5 years?
This industry is ripe for a more integrated model from a technology perspective. A lot of point solutions were built in the last 15 years and they solved individual problems. If you look at our practices that are buying the software, they are now assembling all these point solutions and trying to integrate them together to get to the answer they need. But no one solution is doing everything or even 80% of what they need to do as a practice, so it’s hard. Imagine that you’re managing a practice, you’ve got your physical therapy degree, and now you’re running a business and you have to be an IT person. That’s just not sustainable. The winners in this model will sit in the captain’s chair as if they were one of these company leaders — whether they were small, mid-market, or enterprise — and think about where people are having their broadest challenges from an integrated solution perspective. Then they will solve those challenges.
I’m not saying I have to be the only provider of software to these companies, but I think there’s ample room to integrate more pieces of the solution so that we take some of the burden off of our customers. Where I saw a lot of innovation in my last business, and I see now sparks of innovation that we can push forward, is how do we fully automate that patient experience? Imagine that our patient went to their general practitioner, they got diagnosed with a problem, they wound up in a hospital, and maybe they had surgery. Then they have to get therapy, medication, et cetera. But in today’s environment, the patient is managing all those interactions disparately because those systems don’t talk to each other and the patient is deciding if the outcomes are coming together.
My goal is that we integrate that patient experience and make it easy for them to cross through all the providers that they need to access. It allows those providers to easily communicate with each other as to what’s going on with that patient. Not the case, but the patient. They key to the value-based care model is making sure that we are looking across all of the modes of treating the patient and ensuring that we are optimizing them. The company that nails that will get a lot of traction.
Our goal is to be part of that ecosystem, to have a high degree of interoperability with the hospital network or the systems that the doctors might be using and make it easy for overall monitoring of the patient and not that individual problem that the therapist is trying to solve, because it exists generally in the scope of more problems. Our business is unique in that very rarely is that problem an isolated problem. Most of the time, we’re treating someone in the context of a larger course of treatment. Our industry has a huge opportunity to connect better to the broader course of treatment, and that’s where I think the future will go. You are integrating that from the patient perspective and you are integrating that from the clinician perspective.































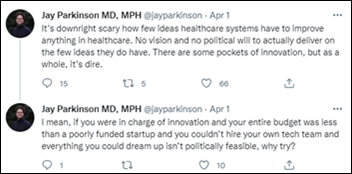
The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en