News 4/13/22
Top News
Oracle extends its Cerner acquisition deadline from April 13 to May 11, with no other changes of terms to the $28 billion deal.
Oracle says that 11.5% of CERN shares have been tendered as of Friday.
Reader Comments
From HIS-Oldimer: “Re: Bon Secours Mercy Health. Is considering outsourcing infrastructure, Epic, Workday, and other platforms. The project, which is valued at $200 million over three years, could affect 350 to 900 employees. who will be rebadged to the winning firm (the usual suspects – Atos, Deloitte, and HCL) and released 6-12 months after training their offshore replacements. It will close Q3 2022.” Unverified.
HIStalk Announcements and Requests
Welcome to new HIStalk Gold Sponsor Myndshft of Mesa, AZ. Myndshft’s software-as-a-service automates and simplifies time-consuming healthcare patient access tasks associated with prior authorization, eligibility and benefits verification, and patient financial responsibility, freeing providers and payers to concentrate more fully on patient care. Myndshft works with leading providers, payers, and health information exchanges. A company overview is on YouTube. Thanks to Myndshft for supporting HIStalk.
It’s been a long time since the top-of-page banner spot was available. It gets lots of clicks, so contact Lorre to book it long term.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Laboratory systems vendor CliniSys Group acquires ApolloLIMS.
Senior-focused value-based care company Vytalize Health raises $50 million in a Series B funding round. The company has partnered with 280 primary care practices in 16 states to offer their patients virtual and in-home care enabled by its technology. Vytalize acquired patient communication company MedPilot last year.

Moxi hospital delivery robot developer Diligent Robotics raises $30 million in a Series B funding round. The company will use the investment to expand integration capabilities with hospital EHR and clinical communication software.
Imprivata acquires digital identity management vendor SecureLink.
Sales
- Wayne Health (MI) will implement digital health services from Qure4u that include online scheduling and appointment reminders, telehealth, remote patient monitoring, digital health screenings, and patient-to-provider communications.
People

Divurgent promotes Katherine Isaza to VP of client services.

Holon Solutions names Mike Kaminaka (Innovaccer) chief growth officer.

Krister Mattson (Essentia Health) joins Gundersen Health System (WI) as VP of enterprise analytics and data science.

Mukta Nandwani, MS (Epic) joins Findhelp, the social care connection technology vendor formerly known as Aunt Bertha, as CTO.

In England, Tunstall Healthcare hires Emil Peters (Cerner) as group CEO.

Nick Gauen (Greenway Health) joins Innovaccer as area sales VP.

IllumiCare hires Ralph Keiser (EPSi) as chief strategy officer.

Elsevier Clinical Solutions promotes Maryann Abbruzzo-White, MBA to SVP of global marketing.


Pegasystems hires Kikelomo Belizaire, MD, MPH (Anthem) as chief medical officer and Barry Chaiken, MD, MPH as CTO.
Announcements and Implementations

Alice Hyde Medical Center goes live on Epic as part of the University of Vermont Health Network’s third phase of implementation.
New York-based HIE Healthix implements FHIR-based patient record snapshot technology developed by Hixny, an HIE serving New York and Vermont.
Netsmart will integrate Bamboo Health’s OpenBeds resource with its CareManager population health management software to better enable healthcare organizations to respond to demands for crisis-oriented care. The Missouri Behavioral Health Council will implement the new technology as part of its statewide crisis management program.
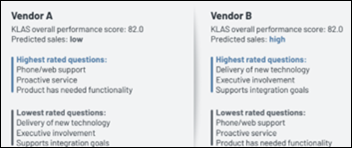
A new KLAS vendor-only report finds that the company’s own overall performance score, such as Best in KLAS, is not among the strongest predictors of sales among the factors that KLAS measures. Sales volume predictions are most closely correlated to KLAS categories of likely to recommend, supports integration goals, delivery of new technology, and executive involvement. Factors associated with lower sales are money’s worth and median number of years live, both of which are indicative of products that are late in their life cycle and thus at risk of being replaced. KLAS says that Best in KLAS is mostly used by buyers to create short lists and to identify questions to ask, with few organizations mindlessly buying the top-rated product. An unstated possibility is that customers don’t actually use KLAS to make product decisions and that KLAS reports reflect rather than influence vendor performance.
Government and Politics
A VA-sponsored study of veterans with mental health issues living in rural areas finds that 36% of the 13,000 who received a video-enabled tablet during COVID-19 were less likely to make a suicide-related visit to an ER, and that 22% were less likely to show suicidal behavior.
HHS will collect data from more than 2,000 providers on their medical bill collection practices as part of the federal government’s efforts to crack down on consumer medical debt. The data will be used in future grantmaking and policy decisions.
FDA warns providers that imaging software cannot be used to diagnose stroke patients, only to prioritize cases for a radiologist’s review. FDA also tells providers that the devices may be specific to certain arteries only rather than all intracranial vessels and are unable to rule out the presence of large-vessel occlusion.
FDA clears the atrial fibrillation detection algorithm of Google-owned Fitbit, which assesses heart rhythm while the user is passive or sleeping. The algorithm measures heart rhythm via a blood vessel expansion optical sensor that will soon to be incorporated added to Fitbit devices. The company’s ECG app will remain in place so that users can perform a spot-check rhythm screening and ECG capture, while the new technology supports long-term background assessment.
Other

Allscripts and Cerner achieve top customer rankings for their integrated EHR and RCM technologies, according to Black Book’s latest survey of 1,700 community hospital end users.
Sponsor Updates
- Netsmart showcases the power of a digitized platform and Certified Community Behavioral Health Centers leadership at the National Council for Mental Wellbeing 2022 Conference through April 13 in Washington, DC.
- The Incremental Healthcare Podcast features About Healthcare CMO and co-founder Darin Vercillo, MD.
- KLAS Research highlights Agfa HealthCare as one of the most frequently considered vendors in the Middle East.
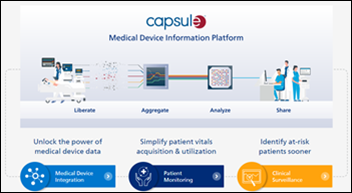
- Philips Capsule will exhibit at AONL in San Antonio through April 14.
- CareMesh publishes a new case study, “From the Hospital to the Extended Care Team: Tampa General Hospital Notifies, Transitions, and Connects with Any Healthcare Provider in the Country Digitally.”
- Get-to-Market Health’s Steve Shihadeh interviews investor Lee Shapiro of7wire Ventures in Part 1 of “How Health Tech Companies can Grow and Thrive in Today’s Challenging Environment.”
- CarePort will present at ACMA National 2022 May 3 in Dallas.
- Change Healthcare publishes the “2021 Laboratory Ordering Index.”
- Optimum Healthcare IT posts a video titled “Optimum CareerPath Testimonial: Ben Mensalis, CHIME’s 2021 Innovator of the Year.”
- CHIME releases a new podcast, “Leader to Leader: Getting to Interoperability with Ajay Kapare and Marc Probst.”
- Clearsense has sponsored the Banner Health Children’s Open golf fundraising tournament.
- Crossings Healthcare Solutions names Marjorie Fiorilli (Ascension) project manager, and Shyla Dubois and Lucien DeCecco account executives.
- Dina joins the Florida Association of ACOs.
Blog Posts
- Improve Practice Outcomes by Outsourcing Your Revenue Cycle (AdvancedMD)
- Proactive External Audits and Other Tips for Avoiding OIG Investigation (AGS Health)
- Developing and Engaging Preferred Post-Acute Networks (Bamboo Health)
- 3 conference takeaways: Activating patient data across the care journey (Bravado Health)
- 2022 CHIME CIO Survey Results Are In (CereCore)
- Easing Clinician Burnout, Cybersecurity Fatigue (Cerner)
- 21st Century Cures Act: Interoperability and Information Blocking and What it Means for Healthcare Organizations (Clearwater)
- Hospital-at-Home Patient Testimony: Joy (Current Health)
- How Data Analytics Can Help Advance Your EHR Strategy (Dimensional Insight)
- Focusing on Public Health: Staying Connected with the Community (EClinicalWorks)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.












































There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…