Curbside Consult with Dr. Jayne 1/30/23
I’m putting my travel schedule together for the next few months, and I’m pretty excited about some upcoming conferences. Although HIMSS is back in Chicago, the other two are in cities that I don’t get to as often as I’d like. I’ll be attending the American Telemedicine Association (ATA) in San Antonio in early March, and then the CHIME/ViVE event in Nashville later in the month.
I typically register for conferences as early as I know I’ll be attending so I can get the early bird discounts – and for ViVE, the discount is just about a necessity. It’s one of the more expensive conferences I’ll be attending and I hope it lives up to the hype (as well as the cost).
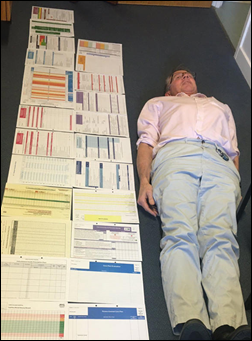
Usually, the decision to attend a conference is based on a directive by an employer or a client, rather than me looking at specific sessions or content. Because of that, I don’t always look at the agendas in detail until they get closer. Depending on the conference, some of them don’t even post agendas until shortly before, meaning that many people make the decision to attend without all the information that would help them make a good decision.
Even though I’ve been doing work in the telehealth space for half a decade, I haven’t attended the ATA meeting. I dropped by their website today to think about what I might like to attend, and the first thing that caught my attention was the tagline on the home pages of “Telehealth. Is. Health.” Which is interesting since the organization has seemingly decided to stick with the “telemedicine” moniker.
Organizations rebrand all the time and spend lots of money doing so, as we recently saw with the rebrand of Intermountain Healthcare to Intermountain Health. The substitution of the word “health” where organizations previously used “medicine” or “medical” seems to have happened just about everywhere else, starting with the transition from electronic medical records to electronic health records. The change indicates that an entity is about something more than just medicine or medical practice.
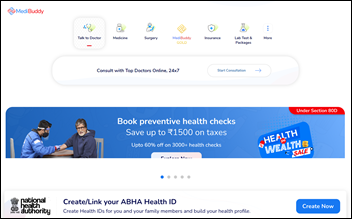
The realm of telehealth has become significantly larger in the last five years and now includes more than just medical practice. Some of the hottest areas for growth aren’t even “telemedicine,” but include all the other ancillaries that patients need for comprehensive care. Some of these include remote monitoring, psychotherapy, counseling, occupational therapy, physical therapy, speech therapy, nutrition consultations, pharmacist visits, dental advice, and more.
In most states, these areas wouldn’t be considered as “medicine” under the state medical practice acts, so the broader term of telehealth makes more sense. It makes me wonder if the ATA is just keeping with tradition or if they think a rebrand isn’t worth it, or if they don’t see value in going with the broader terminology. From a marketing standpoint, they would still be the ATA, so at least that’s easy. Some of the possible domain names they’d need for a rebrand aren’t in use, although it can sometimes be tricky to get a domain you want if someone is already holding it, so that may be a factor. They do use “telehealth” throughout their publications, at least.
ATA shifted the dates of the Annual Conference and Expo this year, moving it from a Sunday through Tuesday format to a Saturday through Monday format in an attempt to reduce the number of days people need to miss from a traditional work week. Depending on where you are traveling from, however, as well as how much of the conference you are planning to attend, many of us will still miss two weekdays due to limited travel options. Flying into San Antonio isn’t as easy as going to Chicago, Las Vegas, or Orlando, so I guess that’s the downside of having it in a smaller metropolitan area.
The full agenda is available and there certainly isn’t a shortage of good sessions to attend. A couple of my medical school colleagues who are now involved full-time in telehealth will be there, so I’m looking forward to it. Not to mention that San Antonio’s climate in early March is a lot more alluring than the Midwest, as is the Tex-Mex scene.
As for CHIME/ViVE, the value of the ViVE side of the equation is a little more difficult to judge. I really enjoyed CHIME in the fall, especially the low-key vibe and the ability to have high-quality conversations with peers. ViVE is only in its second year and they have really been pushing hard for registrations. I was a on a CHIME/ViVE call last week that was advertised as a way for people to understand the value of attending, but ended up being entirely too salesy. If I heard one more person talking about how it was “curated just for people like you” I thought I was going to scream.
We are less than two months out and they don’t have a full agenda published yet, so it’s hard to judge the value on a day-to-day basis. It’s also hard to schedule meetings and times to connect with colleagues, because it’s inevitable that the time I pick will end up being in conflict with a session I’ll ultimately want to attend. The agenda “themes” are published and several are eye-catching for me. One has a tagline of “delivering virtual care with intention,” but I’m not enamored with its actual title, which is “That’s so Meta.” I’m also interested in sessions on: recruiting, retention, and team development; managing chronic care costs; technology cohesiveness and efficiency; and using technology to advance health equity (although I’m not a fan of using the new buzzword “techquity” to encompass it).
I’m looking forward to visiting Nashville for the conference, as I haven’t been there in years and it’s a good excuse to hang out with one of my shoe-loving besties who happens to be a local. The last time I attended a conference there, it ended up being one of the most crazy drunken vendor user groups ever, so I’m hoping for something significantly more tame. I’m sure my friend will give good advice for off-the-beaten-path adventures that will still let me be vertical the next day. It sounds like Nashville has become quite the foodie city since I last visited, so that’s something to look forward to as well.
What are you looking forward to about upcoming conferences? Is it the food, the people, or the content? Leave a comment or email me.

Email Dr. Jayne.
































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…