Submit your article of up to 500 words in length, subject to editing for clarity and brevity (please note: I run only original articles that have not appeared on any Web site or in any publication and I can’t use anything that looks like a commercial pitch). I’ll use a phony name for you unless you tell me otherwise. Thanks for sharing!
Is There Really an End In Sight? Will EHR Be the Answer?
By Pat Clark
With all of the media attention being given to the “new, improved and affordable healthcare in the US” who will actually benefit? The “real life” continuity of patient care seems to be worse now than ever. With the new federal regulations forcing healthcare providers to implement and use EHRs and physician’s being forced to track and record meaningless quality standards, you would think that the public is finally getting the “quality, affordable, well informed “ healthcare they deserve.
In this age of unlimited access to all levels of information technology , including the ability to communicate sensitive patient information from one physician to another and/or between facilities, there is no reason for the major disconnect we still see in today’s patient care. All healthcare providers involved in a patient’s care should be completely informed about their shared patient and have access to that patient’s recent medical history and list of current medications.
Unfortunately, this is not the reality of today’s healthcare environment. The onus of healthcare and the continuation of care for each patient is still the sole responsibility of the patient and/or a family member (when possible) to battle the convoluted maze of US healthcare and “follow-up patient care”.
I have been involved in healthcare for over 30 years, both on the clinical and administrative sides. As a healthcare consultant, working with facilities to help interpret the federal guidelines, I have been a huge fan of the current push towards EHR and the true intent of HIPAA.
Recently, however, I have had the personal pleasure to experience the true disconnect between facility inpatient care and the transition to outpatient follow up care. I am totally amazed that any elderly patients survive post-hospital life. My experience is not limited to one facility or even to one state.
My father was hospitalized in Asheville, NC after having a stroke in September 2009. He was evaluated, admitted, monitored, and released within two days. His stroke was considered minor, but he was left with memory and vision loss.
His discharge papers were filled out accurately and he was promised a series of social and rehabilitative services, including: visiting home health, physical therapy, Meals on Wheels, and community transportation. Very few services were actually provided. Park Ridge Hospital did send a social worker to the house to assess my father’s needs. It was determined that he did indeed need home care to help with not only his physical therapy, but also his new assortment of pharmaceuticals (14 pills to be taken at different times throughout the day).
It took five additional days to get another hospital employee to come out to the house to draw blood for his Coumadin management and then several additional phone calls to get a physician to monitor the dosage. Without help, my father would not have survived!
Two months later, my father moved to Scranton, PA to be closer to family. As a responsible adult, my father gathered all of his medical records and immediately made an appointment to establish a new primary care physician.
Within two weeks of his initial visit, my father suffered a heart attack in our new house. Because my father is a diabetic, his heart attack symptoms were not classic chest pain but simply a “funny feeling”. When the “funny feeling” did not go away, we decided to go to the ER. At that point, my father began having trouble breathing and walking. The local police were wonderful and the ambulance services were quick to respond.
My father was taken to Moses Taylor Hospital, Scranton, PA, diagnosed with CHF, and then admitted to ICU for the acute MI. He was monitored and stabilized for 72 hours and then transferred to Mercy Hospital, Scranton, PA., where he had a complete cardiac workup, including a heart catheterization and bypass surgery. Once my father was stabilized, I became terrified. How was I supposed to coordinate the care needed to allow my father to recuperate completely?
After having experienced such poorly coordinated post-hospital care in NC, I was nervous about the care required after a 20+ day hospitalization. This time, the discharge papers from Mercy Hospital were unbelievably disgraceful! There were drugs crossed out, dosage changes, and follow-up requests scribbled all over the place.
I refused to take my father home until I personally spoke to a home health nurse that would follow up with my father upon discharge. Fortunately, my request was honored. It took the HH RN over three hours to identify what medications were active and which ones were to be discontinued. She also had to negotiate between physician offices to see who would monitor my father’s daily Coumadin.
After Christmas, the discharge notes stated that we needed to make three different follow-up physician appointments. Only one of three physicians even knew why we were calling.
Gotta love the new EHRs and transportation of patient information! I can’t wait to see the new “affordability” portion of healthcare in action.
Pat Clark is a healthcare consultant for a software vendor.
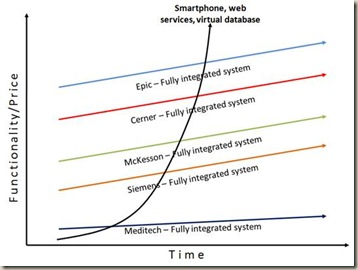
Future in Healthcare IT
by Mark Moffitt
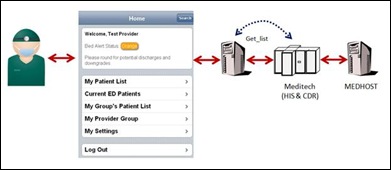
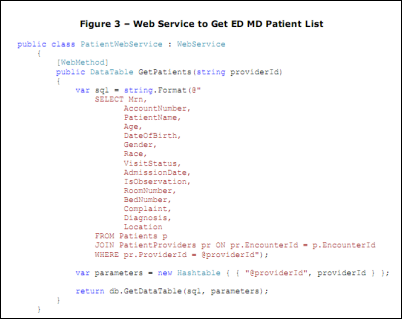
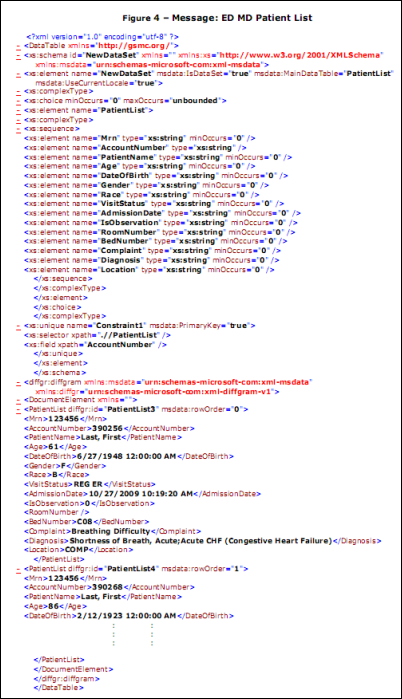
Early in the morning Dr. Brimmer, chief hospitalist at Good Shepherd Medical Center, pours a cup of coffee and reaches for her iPhone. She logs into an iPhone application using a four-digit PIN, like her ATM, on a large virtual numeric keypad. Elapsed time to login: three seconds.
Dr. Brimmer is alerted that one of her patients has a critical potassium level. She taps on the icon “Contact Nurse” and the application dials her iPhone.
The nurse assigned to the patient feels her iPhone vibrate and reaches in the pocket of her lab coat, grabs her iPhone, and answers, “This is Sharon Thomas in A600 and how may I help you?” Dr. Brimmer identifies herself and instructs Sharon to give the patient potassium bolus of 40 mEq and repeat the lab test in five hours.
Sharon walks to a computer, selects an icon on her iPhone desktop, and a message is sent over Bluetooth to the computer and an application automatically logs her on and displays only those patients assigned to her. She taps the screen to select Dr. Brimmer’s patient and taps the “Order Med” icon. The application displays the top 25 meds most often ordered by Dr. Brimmer. The list is dynamically updated after every entry. Three more taps on the monitor and the med is ordered and transferred electronically to pharmacy. She repeats a similar process for the lab test. Sharon never touches a keyboard during these transactions. Elapsed time for entering both transactions: less than one minute.
Dr. Brimmer receives a text message on her iPhone notifying her she has an order waiting her approval. She selects the link and the med and lab order entered by Sharon is displayed on her iPhone browser. She approves the order. The transaction is recorded. Elapsed time for transaction: 15 seconds.
While entering the med order, Sharon is alerted that the patient’s allergy information has not been updated since 2008. She selects the “My Tasks” folder and taps the icon “Add a Task.” She selects “Update Allergy”, selects a patient, and enters “Now.” She selects “OK” to complete the task. She enters another task by tapping the icon “Lab Test,” selects a patient, Potassium lab test, and selects “5 hours.” She selects “OK” to complete the task. Elapsed time for both transactions: less than one minute.
Sharon gets distracted with other tasks and forgets to update the patient’s allergies. Five minutes later, her iPhone vibrates. She reaches for it and selects the link and it pulls up “Reminder: Update allergies on Mary Johnson” on her iPhone browser. Sharon walks to the patient’s room, obtains allergy information, and then enters allergy information on her iPhone while talking to the patient in the room. The patient shares with Sharon her grandson has “one of those gadgets” as she points to the iPhone. They both share a laugh. Sharon asks the patient the name of her grandson and discretely records the name using her iPhone. Sharon knows patient satisfaction scores can be improved by remembering important tidbits like a grandson’s name.
Ten minutes later, a pharmacist processes the patient’s med order. The pharmacist notes the recently updated allergy information and that the order was entered by Sharon and electronically approved by Dr. Brimmer. The pharmacist processes the order.
Dr. Brimmer completes her review of critical labs while she sits at her kitchen table sharing the time between preparing for work using her iPhone and talking to her kids before school. She appreciates the ease and convenience of the iPhone application that makes it easy to do both. As a result, she can spend more time at home in the morning with her kids while preparing for the day.
Sharon’s iPhone vibrates again and she reads that a patient’s med is available in Pyxis. She retrieves the med from Pyxis, gives it to the patient, and then records the administration on her iPhone. Tap, tap, tap, and she slips the iPhone into her lab coat pocket. Elapsed time for transaction on the iPhone: less than 15 seconds.
Later that day, Sharon’s iPhone vibrates and a text message is displayed with a link that takes Sharon to a Web page that alerts her to collect blood for a potassium lab test ordered earlier in the morning by Dr. Brimmer.
Note: All of these events are possible with current technology or will be possible with anticipated enhancements to the iPhone OS or with current unsupported third-party software. No $20 – $50 million healthcare IT system is required. This level of functionality is possible with legacy healthcare IT systems.
Mark Moffitt is CIO at Good Shepherd Health System in Longview, TX where his team is developing innovative software using the iPhone, a web services infrastructure, and a virtual clinical data repository.
Lessons Learned From Our Top 10 Infamous Interviewees
By Tiffany Crenshaw

You just landed an interview with a coveted hospital in the city you’ve been dreaming of for years. It would mean a significant pay increase, along with stronger job opportunities for your spouse and better schools for your kids. As you don your best suit and head with sweaty palms to what you are hoping will be your next place of employment, don’t forget to pack your common sense. This list of our favorite infamous interviewees may serve as good reminders of what can happen when you leave your common sense behind. Enjoy!
The Dawdling Responder
One job seeker sailed through the interview process and was immediately offered the job. Perhaps no one told him that it would not be prudent to respond, “Thank you so much for this opportunity! Tell you what — I’ll be getting back to you in six months with a response on your offer.” Of course it may have been worse had he demonstrated his enthusiasm at the offer by busting out break-dance moves, but common sense would have dictated that he communicate sincere interest in the opportunity by providing a timely response. Six months — not so timely. If you need a few days or even a week to consider an offer, assure the interviewer that you will get back with her or him on a specific day. And then, of course, follow through.
The Mute Criminal
Criminal background checks are standard, no surprise there except to the interviewee who underwent a lengthy interview process all the while hoping that the misdemeanors he’d accumulated through the years (one per decade) would be ignored. It wasn’t, and this particular interviewee had no skill at spinning his experiences into positive outcomes, so he began his muddled reply with a rather uncomfortable and protracted pause. The interviewer, predictably, was not impressed. The candidate’s time was wasted, as was the prospective employer’s. If you have a skeleton or two in your closet, it won’t necessarily disqualify you from a position, but anticipate that the interview process will uncover those bones. Take control of this issue by bringing it up before a background check reveals it, and address the issue in a positive light, explaining how you have grown through or acquired new skills as a result of the experience.
The Lunch Lady
A well-dressed woman with a professional demeanor and a stellar resume was demonstrating to her interviewers how she led training sessions. Normally in these sessions she would provide snacks to the trainees, so she decided to provide snacks to the interviewers as well. After all, it was lunchtime, and there may have been a few stomachs rumbling. Unfortunately, though, to her interviewers, this smacked of unprofessionalism. Perhaps they were concerned about dribbling goo on their ties or blouses, or perhaps they did not want crunching sounds to compete with conversation. Either way, her decision to incorporate a potentially charming if slightly unusual interview tactic lost her the job. So if you are ever in doubt about whether an activity is appropriate, be conservative.
The Want-to-Be Comedian
A male interviewee was asked the familiar “How do you handle work pressure?” question. He drew a pensive expression and then creatively replied: “I liken it to my experience surviving in a household of teenage daughters with PMS.” And, readers, he didn’t stop there. He made a few jokes about preventive measures and calendars. Save it for the stand-up routine. An inappropriate analogy is a great way to offend the interviewer. Creativity is great, but when it borders on the offensive, it moves into hazardous territory. Stay in the region of known safety.
The Tumultuous Telephoner
Picture this: the dog is barking to be let out, the cats are scuffling loudly in the adjacent room, the baby is howling at the top of her lungs, and you are on the most important phone interview of your career. Not a comfortable scenario. Unfortunately, a candidate recently experienced a scene similar to that. The background noise during her phone interview was so disruptive that the interviewer asked if the candidate needed to reschedule for a more convenient time. And if that weren’t bad enough, the candidate’s spouse yelled in the background, “If the hiring manager thinks this is noisy, just tell him to call back in two hours when the rest of the kids get home!” One just cannot convey professionalism from a zoo. If your interview is by phone, lock yourself in a room, keep the pets out, and bribe your family with dinner out for an hour’s total quiet. With common sense in gear you can easily create the calm, distraction-free environment you need to present yourself as the competent, focused professional that you are.
The Chemically-Enhanced Candidate
Clearly nobody with even half an ounce of common sense is ever going to consider doing cocaine during an interview. Well, that part of the cranial grey matter was apparently missing for the job candidate who took a bathroom break during an interview in order to snort a line. Apparently this little fix depleted any other common sense he might have had. When he returned to the interview, he thought it wise to explain to the hiring manager why there may be traces of chemical substances in his drug screen. Hard to believe, but that is a true story. While you certainly will not be ingesting chemical substances in between questions about your professional background and skill sets, you may want to lay off the wine at lunch. And if a seemingly harmless indulgence like a heavy meal makes you drowsy, you’ll need to avoid that prior to an interview. Your mind should be razor-sharp and your thinking, quick.
The Unsavvy Dresser
One interviewee walked into the room and before he sat down, the interviewer had already formed an opinion that was not promising. The candidate was wearing black pants, a blue blazer, and brown shoes. Certainly your mother taught you that it is the inside that counts, right? But not in an interview — this is where you are judged by how you present yourself on the outside. Your professionalism, character, personality, and competence are being assessed visually from the moment you walk into the room. This candidate did not follow the basics of dress codes, and his indiscretion was perceived as an unforgiveable breach of professionalism. Never, ever forget the basics.
The Diverted Traveler
A gentleman booked a flight online for his upcoming interview with a large, highly respected health system. The route included a relatively lengthy layover in the world’s entertainment capital. To pass the time, this job seeker decided to partake in a few of the city’s diversions. Lady Luck was apparently pleased with him, though Lady Prudence was not. As his dollars (or alcohol) accumulated, his good sense diminished, so that when he should have been boarding his plane, he was cashing in his chips. Needless to say, he missed the connecting flight, and, consequently, the interview. The moral of the story: Don’t miss a connecting flight in Vegas on your way to an interview. What stays in Vegas is your good reputation.
The Fast Friend
One sharp, talented candidate was confident that she had not only wowed her interviewer, but also had clicked with her right away. They had several common interests and similar personalities. So, in her thank you follow up note, she included a photo from a recent family trip to a mutually appreciated vacation spot. The interviewer, much as she liked the candidate, was not impressed. The little red flag that signals “What you are about to do may be slightly inappropriate” failed to rise (or it did and she ignored it), and she lost a fantastic opportunity. It’s fantastic to have immediate rapport and that can make for a more relaxed interview, but remember that in the end, business is business.
The Gnashing Professional
The final reason-challenged candidate actually demonstrated a good deal of common sense in many key ways. Unfortunately, the demonstration of professionalism she established with her timely response, favorable background check, clean drug screen, punctuality, polished appearance, and professional appropriateness was dashed to pieces by a tiny wad of gum rolling around in her mouth during her interview. The result was more redneck than executive. But we know you have more common sense than that.
It all boils down to common sense. Although you may not even be able to conceive of doing anything remotely near what these interviewees have done, we have cringed while witnessing these very real events. These examples serve as good reminders to follow the red flags of prudence along the often stressful, but in the end, gratifying, process of interviewing.
Please accept our apologies if you resemble any of these remarks. We are on a mission to create better interviewers one candidate at a time. We believe a sense of humor, dash of common sense and willingness to learn from mistakes are ingredients for career success and life in general.
Tiffany Crenshaw is CEO of Intellect Recources.



































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…