Submit your article of up to 500 words in length, subject to editing for clarity and brevity (please note: I run only original articles that have not appeared on any Web site or in any publication and I can’t use anything that looks like a commercial pitch). I’ll use a phony name for you unless you tell me otherwise. Thanks for sharing!
Is Healthcare Interoperability Possible With a Conflicted Federal Committee?
By Rusty Weiss
Interoperability – the ability of health information systems in different organizations to “talk” with each other – is crucial to the future of healthcare. By tapping into “big data” to learn more from existing information, we will make healthcare more effective and less expensive. By allowing patients to carry their health information across provider lines as easily as we want them to carry their health insurance across state lines, we will empower patients. In fact, one of the stated goals written into the Recovery Act was the development of “software that improves interoperability and connectivity among health information systems.”
But one politically connected left-wing company, Epic Systems, could destroy this healthcare progress.
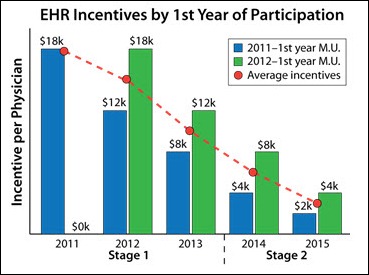
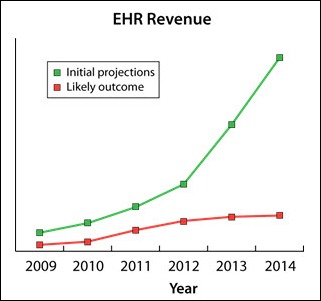
With over $19 billion in stimulus money being dedicated to health IT, the selection of members to occupy the Health Information Technology Policy Committee was a crucial one for the Obama administration. And a platform of interoperability isn’t exclusive to the Obama camp. Democrats, Republicans, and industry experts alike recognize the importance of interoperability.
So why, despite their public support for interoperability, did the administration appoint to the HHS board Epic Systems CEO Judy Faulkner, who opposes the broad consensus position on interoperability?
As Lachlan Markey pointed out in the Washington Examiner, “Epic employees are massive Democratic donors.”
Unfortunately, those political donations may have caused the administration to overlook things like Faulkner’s 2009 comments to Bloomberg News claiming that sharing electronic health records (EHR) “doesn’t work when you mix and match vendors.” She added, “It has to be one system, or it can be dangerous for patients.”
Tariq Chaudhry, a consultant for American Soft Solutions Corp. says, “Judith Faulkner’s version of interoperability reveals a clear effort to establish (a) monopoly for Epic.”
He also believes that after working with Epic for a couple of years, there is little to indicate that their software is unique in the industry.
“I have not seen anything specific to Epic, not found elsewhere that could set (them) apart from other competing EHR/EMR systems,” Chaudhry explains.
In fairness, the entire industry is, according to Otech President Herman Oosterwijk, “15 years behind in interoperability compared with PACS systems”. PACS (Picture Archiving and Communication System) is a technology that allows medical images and reports to be stored and transferred electronically.
Oosterwijk, who has worked with the US Department of Veterans Affairs and the US Department of Defense, believes that “none of the EHR systems are truly open.” He adds, “I can connect a PACS workstation to pretty much any PACS system and query and retrieve images. Compare this with an EMR where we, at best, can get a HL7 feed and/or CDA summary documents out.”
Andrew Needleman, president of Claricode Inc., acknowledges difficulty with the implementation of interoperable EHR systems.
“Due to the amount and complexity of data being transmitted between systems, even systems that attempt to be interoperable run into issues when they send data to other systems.”
Expanding on the complexity problem, Needleman says:
“For healthcare data, even the demographic data to determine if you are talking about the same patient is complex. Then, you add things like medications with dosages, different forms, such as capsules, liquid suspensions for injections, tablets, inhalers, etc. And then you need to include observations, doctor’s orders, lab requests and results, admissions and discharges, billing information, vital signs, etc.”
“Despite the existing standards,” he says, “It’s not an easy task.”
Rob Quinn, a partner at APP Design, a software development company, says the office of Health and Human Services “is trying hard to get vendors to communicate via standards,” though he doubts many health IT companies like Epic will comply.
“There’s simply too much money to be made in locking in their clients,” Quinn admits.
In the end, Needleman isn’t sure if the appointment of Faulkner crosses ethics boundaries, but says a conflict of interest may be unavoidable.
“I think that it would be extremely difficult to appoint someone who was knowledgeable enough about the industry, was willing to serve, and didn’t have an interest in the outcome of the regulations.”
Needleman has a point about the difficulty of finding somebody without any conflict of interest. But it seems like the administration, at a minimum, should have appointed somebody whose business was not antithetical to an interoperable future. Unfortunately, as an iWatchNews investigation pointed out in Politico, the administration has appointed hundreds of big donors to “plum government jobs and advisory posts …”
The appointment of Faulkner poses a significant challenge for the Obama administration. Her opposition to interoperability creates difficulty for the advancement of the health IT industry. The market should decide whether the Epic Systems approach to health IT should be rewarded or deprecated, but – in the interests of interoperability and political integrity – HHS should immediately ask Judy Faulkner to step down from her role on the HHS Health IT Policy Committee.
Rusty Weiss is a freelance journalist focusing on the conservative movement and its political agenda.
Is Meaningful Use Enough When Disaster Strikes?
By Eric Mueller

Within the last 12 months, natural disasters have taught the health IT community the necessity of preparation. We’ve seen tsunamis threaten nuclear disaster; tornados wipe out entire communities and hospitals; earthquakes damage national monuments; and hurricanes effect remote coastal towns. In the wake of Hurricane Irene’s flooding and billions in damage, I truly wonder what we can learn from this experience in an effort to make the next disaster … less of a disaster.
When I think of disasters, I think of recovery. In health IT, how do we clean up and recover from the unexpected? How do we recoup data, tests, records, history, systems, schedules, hardware, software, and all the technical things that make our facilities run? Katrina occurred six years ago, yet some areas of New Orleans are still cleaning up. Virginians can tell you all about the unexpected now that they’ve experienced an earthquake in their back yard.
And who can forget the tragic images of Joplin, Missouri, where St. John’s Regional Medical Center stood directly in the path of the monster EF-5 tornado? Thankfully, St. John’s had just switched to an electronic medical record system, though it reportedly sustained some permanent paper record loss. We’ve already heard reports of IT-related problems stemming from Irene with offsite centers and backup generators failing along with general logistical and access issues. Unfortunately, after the dust settles, we’ll likely hear of communication outages, lost patient records, and failed technology – a story that is become a bit too familiar.
Having learned from past disasters, many large facilities have business continuity plans in place to restore their operations quickly. They have online data storage backups and cloud-based hosting facilities to mitigate minimal interruption and risk. But what about those that don’t? Many physicians and hospitals across the country continue to lack capital and access to advance to technology typically afforded to large hospitals. Many find it challenging to meet the noble intentions of Meaningful Use, which is designed to do just that. Reach the communities that don’t have the funds or access.
Long-timers in health IT know that implementation and adoption of new technology can be S-L-O-W. So when exactly is the appropriate time to hold ourselves and our vendors to a higher standard of safety, data recovery, and connectivity over finances? What measures do we enact to safeguard our IT investment before a catastrophic event strikes? Moreover and most importantly, how do we help those caregivers in need RIGHT NOW of information technology?
For example, cloud technologies are words that scare us. We think liability and compliance obstacles instead of opportunity and solutions. Flexibility is paramount. Many organizations are in critical risk positions because archaic and poorly funded IT processes and architecture are wrapped around one very inflexible platform. In allowing the unknown to stop us from proactively seeking out sustainable solutions, will we allow history to repeat itself the next time a natural disaster crosses our path?
Creating flexible and efficient solutions provides the foundation for innovation and problem solving. Remember, if your vendor doesn’t play well with others, Mother Nature will force you to figure this out. Patients rely on the entire continuum of healthcare to do one thing – deliver great care. Doctors, nurses, and administrators can’t deliver great care without depending on their arsenal of tools and technology in their greatest time of need. Let’s challenge ourselves to be innovative and redefine Meaningful Use in ways to help all providers regardless of size and limits, both at work and in our communities. I believe it’s worth the effort.
Eric Mueller is president of WPC Services of Seattle, WA.
Is It Only CPOE, or Is There More?
By Daniela Mahoney, RN

We’ve got to think about what is ahead of us more holistically. CPOE is no longer a standalone project. If there is one common denominator amongst any size hospital that is embarking on this journey, it is the fact that the effort is considerably underestimated. Unless you have directly experienced projects of such magnitude, it is natural to treat and plan for this project as you would for any other.
What makes CPOE so different? It is often a multi-year process, especially for larger organizations. It has clear beginning, but not an end. It impacts every operational aspect of a hospital’s business. Above all, it leads to significant clinical transformation efforts that are not welcomed by providers and clinical staff.
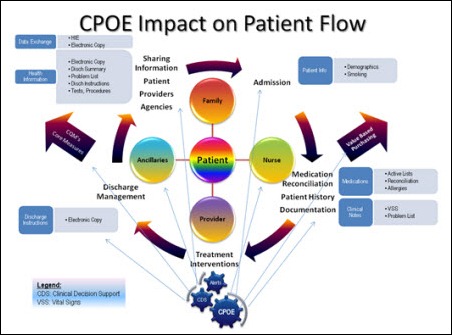
Adding to the complexity of delivering CPOE within the Meaningful Use timeline is that all of the clinical components targeted for Stage 1 interrelate. We have two significant integration points: (a) the integration of the CPOE application with the appropriate modules and technologies (lab, radiology, pharmacy, documentation, ED, medication reconciliation, discharge instructions, etc.) and, (b) integration of clinical workflows. The latter is more challenging.
The easier question that organizations should ask is not what CPOE impacts in a hospital, but what it does not impact. That answer is by far shorter. To drive successful CPOE implementation, we know that the leaders have to be involved to “pave” the road and set direction.
To achieve Meaningful Use Stage 1, a cadre of leaders — including the CEO — need a working knowledge of the requirements and organizational changes necessary to succeed. An IT strategic plan aligned with the vision of the organization should be in place at the time Meaningful Use projects are executed. For successful organizations, their strategic plan is centered on the patient and how to maximize clinical performance, the need for increased transparency, pay for performance, provider engagement, and building and expanding business intelligence capabilities, to name a few. This calls for resources, innovative technologies, and infrastructure, as well as a strong leadership team that is able to drive such a vision.
The CIO’s role in the execution of the vision is essential. To successfully attain these goals, the infrastructure must support all these clinical and revenue-generating applications and the new tools that optimize the care delivery process. Someone made the analogy that the infrastructure is like a garden — cultivate it and it will produce expected results, but ignore it and the weeds will take over. As we plan the budgets for these initiatives, although we lead with saying that these are clinical applications and we need to focus on clinicians, we cannot minimize the importance of reliable infrastructure.
In the big scheme of things, what does CPOE impact? Putting it simply, it will impact everything that a provider order does today. Moreover, if what happens today is not functioning at the most optimum levels, then CPOE will accentuate all inefficiencies, resulting in potential barriers towards its adoption. Even processes such as the timely assignment of the appropriate provider to a case will impact CPOE, as any delays or inaccurate information will cause disruptions in communication, delays in care, inaccurate physician performance reporting, billing, etc.
Another critical factor is the fluency of clinical processes related to patient flow, especially at the points of entry through ED or PAT/surgery. As an example, take the efforts of trying to integrate CPOE with a disparate ED system while fine-tuning the medication reconciliation processes. In most cases, the result is a mixture of new processes that could still place patients at risks, unhappy providers if they have to use multiple systems, and budget overruns. Time is a precious commodity – neither the patients nor providers want to waste it.
How do we plan for CPOE? It is by beginning with the end in mind and creating a patient-centric implementation. CPOE has to be safe, should optimize our clinical performance, and improve organizational efficiency. It is complex, but we can simplify it by always asking the question: will the patient and provider/clinicians benefit from it? If the answer is yes, then we are on the right track.
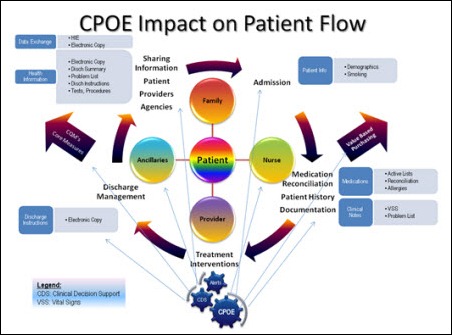
I mapped a visual diagram on how to think about the Meaningful Use components in parallel with what is happening to a patient when admitted to the hospital. This will provide a reference of thinking about what we do in a different way.

And of course, I did not forget about another delicious recipe you could try as we are approaching the end of the summer. I know this has nothing to do with CPOE other than finding a way to relax after a long day at work. And next time, we will talk more about provider adoption, organizational culture, and how to look for that value proposition.
Daniela Mahoney RN is vice president of Healthcare Innovative Solutions of Seville, OH, A Beacon Partners Company.
PHR: the Unicorn of HIT
By Ryan Parker
The Personal Health Record (PHR), in theory, is one of the best ideas in healthcare. Not only in terms of value (think of Facebook and Twitter’s skyrocketing valuations), but also in terms of patient care. As a depository of information, medical records would be easily accessible by patient and provider alike, with medications, procedures, and diagnoses always being accurate and up to date.
Unfortunately, the PHR is the unicorn of healthcare IT.
There have been some valiant efforts, but everyone seems to miss the key reasons why this fantastical PHR will remain just that, a fantasy.
- PHR interoperability would be an issue. For a viable PHR, it would need to link with every practice and hospital, not only to ensure that providers can view information, but to also make sure that patient data is recorded properly. However, a direct EMR/PHR link would be costly and resource heavy. It would essentially be more effective to create a national HIE (which I won’t get started on why that will never happen). Since we all know that is not an option for the near future, the best option would be to give patients the responsibility of filling out the information themselves. This brings me to my next point …
- People don’t want to take the time to fill out a PHR. Unless they are made to, most people won’t take the time to find a PHR online and then take the necessary time to fill out all of the information accurately to really make it a worthwhile source of information. In order for this to work, you would need almost a social networking/PHR option that draws people in and then allows them to fill out their medical information, essentially a “Facebook for your health.” However …
- There will never be a “Facebook for your health.” I’ve heard this idea thrown around quite a bit, and again, it would only work in theory. Most people only use one social networking site. Although Google+ has seen some initial success, I think it will soon bow down to the Facebook beast. The only way we can guarantee a majority of the population has access and comes into daily contact with a PHR would be for Facebook to add a PHR section, which leads to my final point …
- Facebook will never step into the healthcare arena. Sorry, folks, it is just not going to happen. Facebook is fun, exciting, and laid back. Unless you feel reviewing friends’ home medication list and procedure history is really something that most people would enjoy doing (and if you do, I think you might be in the minority on that one) venturing into healthcare IT would be an extreme departure from Facebook’s prior success strategy.
I, for one, am interested in seeing what the next few years bring in terms of PHR strategy. I think there is an option out there that will work, but it definitely has not been created yet.
Ryan Parker is implementation practice director of Preceptor Consulting Corporation of Fort Myers, FL.












































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…