Readers Write: Al’s Story
Happy Memorial Day. Today’s article is dedicated with a special, heartfelt thank you to all of our veterans serving our country abroad and to those here at home. Many thanks to all of the family members of the soldiers currently serving in harm’s way and to those who have lost loved ones. You all truly demonstrate great courage on a daily basis.
Mr. HIStalk, thank you for being so supportive of the troops. I’ve been present at many events across the country where you have personally recognized and paid tribute to anyone who has served in the military.
I recently sat down with Captain Donna Rowe who shared the story of her husband, Colonel Al Rowe.
Al’s Story
By Lisa Reichard, RN, BSN

Colonel Alvin G. “Al” Rowe
Al Rowe was born in Dubuque, IA in 1933. He became an Eagle Scout by the age of 12. He was a proud Iowa Hawkeye and graduated from the University of Iowa in 1956 with a bachelor’s degree in civil engineering. It was then that he entered the US Army as a Second Lieutenant through the university’s ROTC program. Al also received his masters in science degree from Iowa State University. Like many soldiers, Al could have made six figures working in the public sector as a civil engineer, but instead he chose to serve his country and did so faithfully for 30 years.
In 1965, he was sent with the 82nd Airborne to quell a communist uprising in the Dominican Republic. He was in his Jeep with his comrades and battalion. Sniper fire from rooftops hit him in the head. His comrades saved his life. There would be no one left behind.
“Al [shown third from the right] loved his comrades and put them first. He was a soldier’s solder who cared about his men,” said Donna.
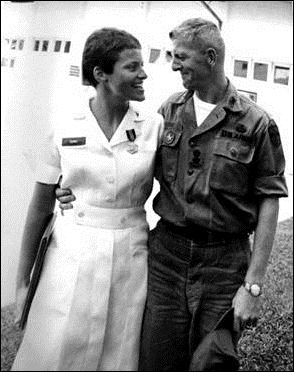
My Sweetheart
According to Donna, “Al was treated for his injury at Fort Bragg, NC. This is how I came to meet him at Womack Army Hospital. He was my patient. I was a nurse supervisor at the time and we met briefly while he was recovering from surgery. Our first encounter was when I had to ask Al to quiet down. He was singing too loudly in the ward. Four days later when he was off duty, he asked to see me and if he could take me to dinner and I said OK. Although Al asked me for my number, I got busy and I walked off without giving it to him.”
“He called for three weeks to get my number, but since army policy is to never give out phone numbers, the ward would not release it. Finally, he called one of my friends who got my permission to give Al my phone number. We finally had our dinner date and when Al came to get me, my Louisiana-native roommate at the time, Carol Burnett, said with a very southern accent when Al picked me up in a white T-Bird convertible, ‘Donna, he has come to pick you up in a white stallion and carry you away.’ We were married 18 months later in 1967.”
Newlyweds Sent to War
Al and Donna were sent to Vietnam during the peak of the war in 1968 and 1969. Donna served as a head nurse of the Third Field Hospital in Saigon, one of the largest shock-trauma-triage emergency rooms in Vietnam. Al served as an adviser and equipment supplier to soldiers in the field during combat.
“Al and I were married 47 years and 10 months. He was my best friend,” said Rowe.
Donna and Al in Vietnam, Christmas 1968: “We sent this photo home to our families.”
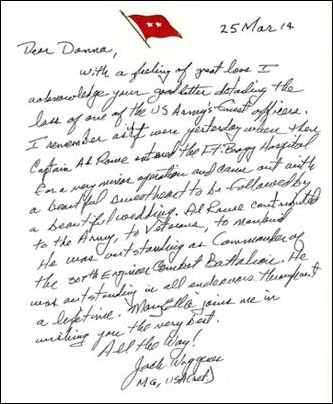
Remembering an American Soldier and War Hero
Donna explained Al was shot down five times in Vietnam, but survived. “The communities where Al served loved and respected him a great deal both here and abroad. The South Vietnamese awarded him the Vietnam Cross of Gallantry.”
Col. Rowe received other military medals and decorations, including the Legion of Merit, the Bronze Star, Meritorious Service Medal, Joint Service Medal, Army Commendation Medal, Purple Heart, and the National Defense Service Medal, and many more. He was also a Master Parachutist.
After Vietnam, he went on to serve in the Pentagon, followed by the Army War College in Pennsylvania, before setting up forces command at Fort McPherson.
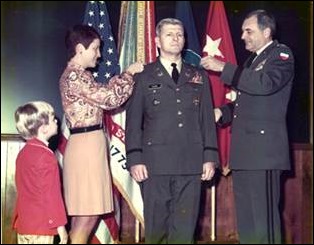
“Al [2nd from left] loved his comrades and put them first. He was a soldier’s solder who cared about his men.”
Al’s promotion to colonel at Fort McPherson in Atlanta in 1974 with Donna and son Richard at far left
“Al was a wonderful family man, and he was very active in the community,” said Donna. “We have two wonderful sons. He was a father figure to many.” She continued, “The military life can be very tough on families. They make lots of sacrifices.”
Upon his retirement from the Army, Al moved to Marietta, GA where he worked for Lockheed as a research engineer. Col. Rowe retired from the Army in 1983 as a colonel and was president of the Georgia Vietnam Veterans Alliance for four terms.
Another Battle
Col Rowe contracted Lou Gehrig’s disease, a neurodegenerative condition that affects nerve cells in the brain and the spinal cord, and struggled with the debilitating disease for three to five years. Donna believes it was service-connected (US Dept of Veteran Affairs – Agent Orange). “The journey with Lou Gehrig’s was difficult. It was another war that Al and I fought together.” She added, “The Department of Veterans Affairs in DC was wonderful during the illness. I really can’t say enough about how well we were treated.”
“Al served his country for 30 years, 10 months, and 22 days before he passed away on January 21, 2014. I miss him dearly. He was loved by many more friends and comrades-in-arms, and he will be dearly missed by everyone who knew him.”
Col Rowe’s legacy lives on through many programs, including the Society of American Military Engineers (SAME), which provides scholarships.
Fast Forward to Telemedicine Possibilities
With the recent resignation of Robert Petzel, undersecretary for health for US Veterans Affairs, there is a lot of discussion around improving timely access to care. General Eric Shinseki, US Secretary of Veterans Affairs, recently said most veterans are satisfied with the quality of care they get, but more must be done to "improve timely access to that care." Telemedicine could help to improve compliance and provide specialized care while decreasing long appointment waits both in the fields and at home for veterans.
Donna was willing to share her thoughts on telemedicine. “I really think it would be great to have telemedicine for diabetes patient maintenance and for treatment of Post-Traumatic Stress Syndrome (PTSS). It would cut down on a lot of hassle around travel time, parking, and other logistics and could help to increase compliance with maintenance programs,” she emphasized. Donna said that telemedicine will be great for soldiers in the field and that email centers exist for communication.
Final Thoughts — Help a Veteran
Hire Heroes USA provides career placement assistance to all of our returning service men and women. Here are some vet-friendly employers, including several healthcare companies.
Thank a Veteran
Donna sharing stories with me from her personal memoirs.
Donna was candid and generous to share her photos for this article. This interview was a good reminder for me that, like Donna and Al, every soldier has their own unique story just waiting to be told. If you get a chance this Memorial Day or any day, talk to a veteran and thank them for their service to our country.
When I started the interview with Donna Rowe about her husband Al, I thought it would make her day. Instead, I left the interview knowing that she had made mine.

Lisa Reichard, RN, BSN is director of community relations at Billian’s HealthDATA. HIStalk also featured an interview with Donna Rowe on The Kathleen Story for Nurses Week in May 2012.
























Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…