Readers Write: The Cost Savings Realized by Single-Platform Solutions
The Cost Savings Realized by Single-Platform Solutions
By Deborah Kohn
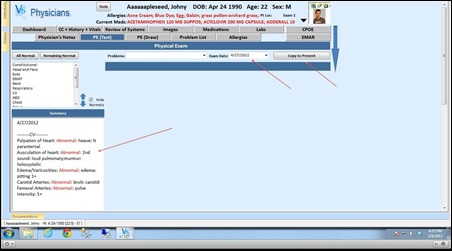
Medicare cutbacks, increased mergers and acquisitions, and declining revenues and margins are daily realities for healthcare provider organizations. Yet so are costly and often mandatory IT initiatives, such as replacing or implementing electronic health and financial record (EH&FR) systems, integrating and securing the next mobile form factor of computing devices, converting to ICD-10 for reimbursement purposes, and meeting the Affordable Care Act requirements.
How does a CIO not compromise on health information technology (HIT) delivery and still maintain cost containment priorities?
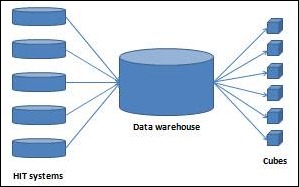
A well-developed, single HIT platform strategy for most applications can realize cost savings by optimizing the IT infrastructure, regardless of whether the platform resides on premise or in the cloud. For purposes of this article, a single computing platform is defined as one that provides a database and set of technologies across a set of heterogeneous applications.
However, still many provider organizations acquire and deploy heterogeneous applications that could be built on a single, common platform. Consequently, this approach continues to generate silos of systems that cannot interoperate and to burn holes in IT operating expense budgets.
Thankfully, no longer is the HIT industry faced with an abundance of best of breed EH&FR applications, typically with each sitting on top of its own proprietary computing platform. Top-selling EH&FR solution vendors finally are offering one or — at most, two — unified platforms for the myriad, structured data-based EH&FR applications.
On the other hand, today, many solutions that complement EH&FR systems remain siloed. Such solutions worth mentioning for this article include but are not limited to Picture Archiving and Communication Systems (PACS) solutions for the storage of image-generating “ology” applications and Natural Language Processing (NLP) solutions for applications such as speech recognition, computer-assisted coding (CAC), and business intelligence (BI). By deploying a single storage platform for PACS solutions or a single NLP platform for speech, CAC and BI applications, chances are that the platform will be around longer than any application an organization has today.
For example, when developing a strategy for managing all the image-generating “ology” applications in the enterprise, it behooves the provider organization to consider a vendor-neutral archive (VNA). This poor choice of name for a storage platform (a more appropriate name might be a PACS-neutral or image file-neutral archive) stores all the heterogeneous, enterprise modality images (DICOM and non-DICOM) in a single, replicated archive. This eliminates the need for each costly, siloed PACS archive and, more appropriately, changes the “A” In PACS from “Archiving” to “Accessing.”
Typically, the platform includes tools to help manage all the different lifecycles of the image data (e.g., retention scheduling and purging mechanisms). And, perhaps the biggest benefit to clinicians is that this platform allows for the creation of an aggregated, patient-centric record of all the enterprise images.
A VNA platform is expensive, requiring a large, complex, capital-intensive project. But well thought out strategies for deploying this platform over time have proven that significant cost savings are realized. Eliminating the organization’s most costly departmental PACS operating expense — recurring migrations with storage media migrations typically occurring every three to four years and PACS replacements requiring massive proprietary data migrations, typically occurring every five to seven years — alone cost justifies this single platform solution.
When developing a strategy for deploying diverse yet complementary EH&FR applications such as speech recognition, CAC software, and BI, it behooves the provider organization to leverage a single NLP platform product that manages each of these technologies well. All NLP engines perform some type of pattern matching, and to varying degrees, incorporate both rules-based and statistics-based techniques. That means that a plethora of applications can be developed using a single NLP platform.
These applications include but are not limited to speech to text (dictation systems), text to code (medical coding), data analytics (data warehouse systems), foreign language translation (Google Translate), question and answer (IBM’s Watson playing Jeopardy), document classification (Outlook’s spam filtering), candidate identification for clinical trials (determining eligible candidates), adverse events (patients with gunshot wounds), core measures (patients who already had been treated), geographic disease epidemiology, and on and on.
At HIMSS13, several complementary EH&FR application vendors were demonstrating more than one heterogeneous application using a single NLP platform. Currently the challenge is that not one vendor offers most of the above applications or even the same applications. Where one vendor might offer medical coding and data analytics using a single NLP platform, another vendor might offer data analytics and candidate identification using a single NLP platform.
For cost justification and interoperability purposes, it behooves provider organizations to strategically look under the hood and determine where a single NLP platform can be deployed.
Deborah Kohn, MPH, RHIA, FACHE, CPHIMS, CIP is a principal with Dak Systems Consulting.















Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…