Weekender 7/10/20

Weekly News Recap
- Health Catalyst will acquire Healthfinch for $40 million in shares and cash.
- A Health Affairs blog post calls for ONC to start measuring the impact of the interoperability requirements of the 21st Century Cures Act.
- VA seeks robotic process automation to import patient documents from external providers into VistA and Cerner.
- Walgreens will spend $1 billion over the next five years to open VillageMD primary care clinics in up to 700 of its stores.
- Informatics pioneer Octo Barnett, MD dies at 89.
Best Reader Comments
The new interoperability regulations that were promulgated in March are like any other regulations, they are only as good as the enforcement actions that will be taken. Thus, while it is fine to have a wish list of those things ONC should track, more importantly is simply enforcing the regs as they stand. Of course, putting on my cynic hat, I see this article from academics as a lead up to a research grant from ONC to support an academic endeavor to measure these metrics. (John)
Those proposed metrics are a bit confusing to me. Measuring things that aren’t in the rule as a way of implicitly adding the things we all wish were actually in the rule (but aren’t) doesn’t seem right. (Brendan)
The main barrier to telehealth is financial. I work for providers who are using telehealth extensively for med refills and wellness visits, and it has been working well. They and their patients want to continue using it, but the insurers continue to waffle on payment policies and suggest that they will only pay for online visits during the pandemic. Of course practices are preparing to bring patients back in whenever possible under those conditions. (Amanda B)
I work in mental health and much of what we do can be delivered quite well by telehealth and often by phone for patients without the ability or devices to do telehealth. The vast majority of our patients do not want to come into the office and the vast majority of our clinicians do not want to sit in a small poorly ventilated office where there is a risk of COVID transmission. However, our organization is strongly encouraging us to see more patients in person because the rates for phone calls are less than telehealth or face-to-face and because the insurers are already jerking us around on reimbursement with the likelihood of additional payment-related travails from insurers and CMS down the road. (RightOn)
Unfortunately, your assessment of telemedicine is spot on. Absent a significant change in healthcare and healthcare delivery in this country, profits ($) will continue to drive behavior, despite the fact that we have the worst outcomes on a number of measures of health and healthcare in the world (including our management, or lack thereof, of COVID-19. (Michael J. McCoy, MD)
Dr. Jayne, I am so embarrassed and ashamed of our healthcare system as I read what you are experiencing in the trenches. We are about four months into this Coronavirus pandemic. I was a little more forgiving (but not much) in March since supposedly this virus caught us off guard. But now? Really? After working in healthcare since the 1970s, I have no words anymore. Just tears. (JT)
Two ways to do something, the right way and again. Allscripts has showed a willingness to take the second option as a standard practice. So, until that stops, they will lose customers. Remember the business model is to buy startups and then promise to integrate them, while not requiring them to integrate. (AnInteropGuy)
Watercooler Talk Tidbits
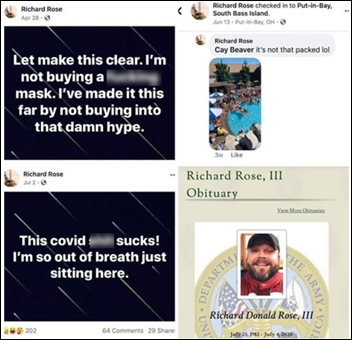
Army veteran Richard Rose III of Port Clinton, OH died July 4 of COVID-19 at 37, with his previous Facebook posts in which he disdained wearing masks and checked in at crowded bars and parties now forming his obituary. He said just before he died that he probably caught the virus at the party on the upper right. Meanwhile a 30-year-old man who intentionally exposed himself to the virus by attending a COVID-19 infection party dies of it, telling his hospital nurse, “I think I made a mistake. I thought this was a hoax.”

A Vice article describes how biomedical technicians are buying non-working, 20-year-old ventilators on Ebay, then using a handmade dongle to program around manufacturer protections so they can fix them. They can then sell the repaired device to US hospitals to meet COVID-19 demand. Newer models validate the identity of the repair tech to make sure they’ve paid the manufacturers’ $10,000 to $15,000 fee that allows them to bypass the anti-repair technology, so the market is in older machines that don’t have that protection. Ventilator manufacturers say their machines are complex and they need to limit who can work on them, while hospitals say it’s their own liability if their highly trained technicians make a mistake, which has apparently never resulted in a manufacturer lawsuit. Hospitals also note that manufacturers wouldn’t sent techs onsite in the early days of COVID, so they were stuck with machines they needed that were awaiting repair.

A Nebraska ED nurse renders aid at a two-car accident that she encountered on her way to her daughter’s wedding.
In Case You Missed It
- News 7/10/20
- EPtalk by Dr. Jayne 7/9/20
- News 7/8/20
- Curbside Consult with Dr. Jayne 7/6/20
- Readers Write: Enabling Clinically Intelligent EHRs
- Monday Morning Update 7/6/20
Get Involved
- Sponsor
- Report a news item or rumor (anonymous or not)
- Sign up for email updates
- Connect on LinkedIn
- Contact Mr. H


Yes! Flip flops are essential as the back up for professional footwear. Plus they are easy to put into your…