News 8/1/12
Top News
Accretive Health will pay $2.5 million to settle charges by Minnesota’s attorney general’s office over its aggressive patient collection tactics in hospitals (including those of Fairview Health Services) and lax security controls involving a stolen PHI-containing laptop. The company will cease all business operations in Minnesota, is banned from returning for the next two years, and can re-enter the state within the following four years only with the attorney general’s approval. Accretive is also required to return all patient information to the hospitals that provided it. The attorney general says she will turn over the patient affidavits her office collected to CMS, suggesting that Accretive’s hospital clients may have violated EMTALA laws that require them to treat emergency patients before trying to collect payment. The $2.5 million settlement will be added to a fund to compensate patients. Chicago Mayor Rahm Emanuel, who had previously inserted himself into the proceedings by trying to use his Democratic Party influence to get AG Lori Swanson to back off, declined to answer questions about his involvement.
Reader Comments
From Yesterdays: “Re: Community Health Systems. Contractor friends tell me they were part of the nearly 600 IT contractors laid off by CHS recently.” Unverified. I didn’t bother trying to confirm since I recently e-mailed someone at the for-profit hospital operator about a rumor that they were switching EMRs, but didn’t hear back.
From Wildcat Well: “Re: Practice Fusion. They have discontinued their affiliate program, which pays websites to promote signups for their ‘free’ EHR.” Unverified. They’re still taking signups on their Web page from what I can tell.
From Carolyn: “Re: National HIT Week. Are you involved in any of the activities?” No. To be honest, I’ve hated that concept from the day HIMSS started pitching the idea that provider IT people should stand shoulder to shoulder with their vendor brethren in trying to persuade politicians to throw taxpayer money at products sold by the vendor members of HIMSS (or as HIMSS nobly rephrases it, “public and private healthcare constituents will work in partnership to educate industry and policy stakeholders on the value of health IT for the US healthcare system.”) I don’t blame vendors for trying to influence the DC crew, but I am totally mystified how hospitals can justify spending the time and money required to send their IT people traipsing around Capitol Hill for the benefit of for-profit companies.
From Safety Paradocs: “Re: Wyckoff Heights. Wired for safety ‘well before ARRA’ as reported by the newsroom of Meditech, yet the young patient was not safe. How can we prevent such striking deaths?” Wyckoff Heights Medical Center in New York, which The New York Times politely calls “one of the most troubled hospitals in the city” because of mismanagement and its hiring of political cronies, admits a 22-year-old student who had consumed a diet drug and beer while pulling an all-nighter for her college Latin course. The hospital gives her IV lorazepam, ties her arms to her bed, and makes no notations in her chart (all documentation was on paper) that anyone was checking on her. Nobody notifies her family. She dies. A few weeks ago, the hospital’s own 83-year-old former chairman, who had been forced to resign and was then admitted for fainting spells, was found in his hospital room with a broken neck. Despite its problems (check out its reviews on Yelp), the hospital earned HIMSS EMRAM Stage 6 and $4.9 million in federal taxpayer dollars for its Meditech MAGIC implementation. To be fair, the incident occurred in 2007, which I assume was long before all of its EMR accomplishments. My takeaways are as follows: (a) while it’s true that better hospitals use more technology, it’s also true that technology didn’t make them substantially better – its use is correlated, but not causative, and plenty of crappy hospitals are using cool systems; (b) all the IT systems in the world won’t help if you have unskilled or uncaring caregivers, so choose your hospital based on quality and reputation, not what they’re packing down in the data center; (c) never, ever go to a hospital for anything serious without having an intelligent and alert advocate sitting by you at close to around the clock as possible, because having worked in several hospitals for most of my adult life, I can say that every one of them screwed up regularly due to inattentive or poorly trained staff, overworked doctors, unwashed hands, failure to notice when patients start to slip, overly aggressive treatment just because it’s possible, and lack of care coordination by all the one-trick specialists running around treating their particular body part of interest. Bring along a friend or family member to check your meds, personally challenge each major decision to make sure it’s based on conviction and science rather than lack of objection, and ask nurses whether your doctor and treatment plan are any good because they know but won’t say unless you press them. I think most hospital employees would agree that you need a wingman.
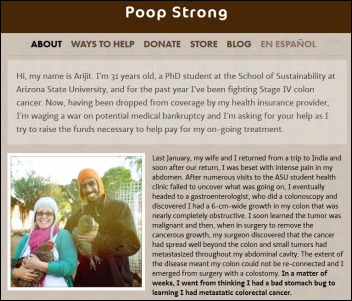
From Westie: “Re: cancer patient whose costs exceeded insurance cap. Wins a victory via Twitter.” Treatment of a 31-year-old’s colon cancer exceeds the lifetime dollar limit of his Aetna student insurance plan, leaving him with no insurance. He gets into a Twitter debate with Aetna CEO Mark Bertolini, who decides to cover the $118K in bills the patient racked up before was able to sign up for a different insurance plan. The tweets are fascinating as observers jumped on Aetna, blaming the company for selling insurance with low caps, questioning what would have happened had the patient not drummed up his own social network, ridiculing the CEO’s $10.6 million salary, and questioning how the Affordable Care Act will or won’t help. I’m glad he’s getting help, but we’re back to the original issue that patients can easily run up more expenses than the insurance they voluntarily signed up for will cover, and unlike every other kind of insurance, everybody expects someone else to pay without objection even though they met their legal obligation. I’d be interested to see who charged what of the $118K University of Arizona Cancer Center bill since those folks aren’t sharing Aetna’s financial sacrifice on the patient’s behalf as far as I know.
From Frank Fontana: “Re: paid endorsement programs such as those from AHA Solutions and the HFMA Peer Review Program. What do readers think about those programs?” I said years ago that they were pay-to-play, but they do still require products to be vetted, leaving me neutral on their value (I don’t see the benefit, but if they help connect vendors with prospects, then I see no harm.) Your opinions, please.
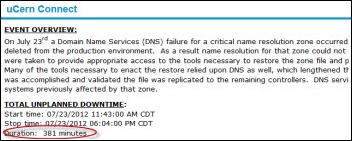
From EMR User: “Re: downtime penalty terms in contracts. We negotiated that any issue that we deem adversely affects our access or system usability allows us to subtract 5% of our monthly fee. We can do this daily up to five times per month.” I’ve said it before, but maybe it bears repeating. List the top handful of items that would be worst-case to you once you’re live on a vendor’s system (downtime, vendor acquisition, hardware failure, lack of acceptable implementation people, poor support) and insist on a penalty if any of them occur. Or, if you’re a glass-half-full type, reduce your fixed payment amount and offer a bonus if none of the events happen (same result, but it sounds nicer.) That makes sure your vendor has a vested interest in not allowing your worst dreams to come true, and at least if they do, you get the slight satisfaction that you’re getting paid for your trouble.
From Laboratorian: “Re: Epic. Could you opine to the extent to which MUMPS is constraining the growth of Epic? Everyone suggests this is a limiting factor, but so far it hasn’t been. How and when would they hit the proverbial wall?” It’s armchair quarterbacks, not customers, that keep trying to create a non-existent Epic Achilles’ heel out of MUMPS and Cache’. Most of that hot air comes from competitors Epic is killing, self-proclaimed experts who’ve never worked a day in IT or in a hospital, and cool technology fanboys who can’t stand the idea that Epic doesn’t care what they think. Despite the use of some ancient underpinnings, Epic’s product is apparently almost infinitely scalable, it does everything customers need it to do, and it works reliably. Nobody cares what it’s written in except their programmers – customers just want solutions, and the decision-makers when Epic is purchased are usually end users and operational executives, not IT geeks who salivate over source code. The only walls Epic could hit would be if InterSystems decided to go out of business (that’s not happening – they were absolutely printing money even before all those thousands of new Epic Cache’ user licenses dropped into their lap); if InterSystems decides to get greedy and either raise their Cache’ licensing fees or stop developing it (doubtful); or if Epic can’t get programmers willing to learn MUMPS (which has never been a problem because they do all of their training in-house and new UW psychology grads aren’t exactly swimming in job offers from Microsoft or Cisco). Anyone who claims Epic is about to hit the technical wall is just trying to plant fear, uncertainty, and doubt in the market. If there’s an Epic wall to be hit, it will be high costs that hospitals can no longer afford with reduced reimbursement, lack of ability to scale as it tries to extend its dominance outside of the US, some kind of meltdown like Judy stepping down and creating a vacuum of power, or perhaps some major and heretofore unfelt shift toward open systems that would put its rather closed model at risk. You’ll know that’s happening when you see the KLAS scores move from green to yellow. The only opinions that count are those expressed by customers with their dollars.
From Infrastructure Manager: “Re: downtime. I used to work with McKesson Horizon Clinicals, which didn’t have a great downtime report system. We scripted a routine that generated a PDF on a different server than Horizon and also copied it to a few PCs. It’s not a fast system to begin with, and you can’t help but feel the system drag when running those reports every hour, even with a huge Oracle server farm run by skilled DBAs. Also, the database design is poor and the tables are not indexed properly – you’ll see 4000 IOPS on a table/storage location and wonder that the hell is going on. If you’re hosted, who cares? Chew up those servers in a data center you don’t run and hope they’ve scaled to the appropriate size. If you aren’t hosted, take these reports very seriously.”
HIStalk Announcements and Requests

![]() Unlike the curmudgeon Mr. H, I have watched a good deal of the Olympics. Who knew team handball was even a sport, much less an Olympic one? Yep, that’s what’s on at 5:00 a.m. on Sunday (don’t ask why I was up so early.) Go Iceland, by the way. So far my biggest complaint is that the men beach volleyball players don’t wear uniforms that are nearly as hot as the women’s. Thank goodness for men’s synchronized diving, however. I have decided that someone ingenious needs to develop an app that blocks all spoilers on Twitter and Facebook so that I will be totally surprised when Michael Phelps becomes the most decorated Olympian of all time (thanks all you expats in England who just had to share the news on Facebook.) Finally, good thing Rio is only one hour ahead of Eastern time so we’ll all see more live coverage in 2016.
Unlike the curmudgeon Mr. H, I have watched a good deal of the Olympics. Who knew team handball was even a sport, much less an Olympic one? Yep, that’s what’s on at 5:00 a.m. on Sunday (don’t ask why I was up so early.) Go Iceland, by the way. So far my biggest complaint is that the men beach volleyball players don’t wear uniforms that are nearly as hot as the women’s. Thank goodness for men’s synchronized diving, however. I have decided that someone ingenious needs to develop an app that blocks all spoilers on Twitter and Facebook so that I will be totally surprised when Michael Phelps becomes the most decorated Olympian of all time (thanks all you expats in England who just had to share the news on Facebook.) Finally, good thing Rio is only one hour ahead of Eastern time so we’ll all see more live coverage in 2016.
Just to prove to Inga that I’m not totally Olympics ignorant even though I haven’t watched the tape-delayed spectacle, here’s an interesting fact: the 300 hospitals beds used in the producer’s opening ceremonies tribute to NHS will be donated to hospitals in Tunisia.
Listening: reader-recommended Son Volt, music for driving or moping in smoky bars. Born of the remnants of 1990s minor stars Uncle Tupelo, somewhere between alt-country and roots rock. REM meets Neil Young.
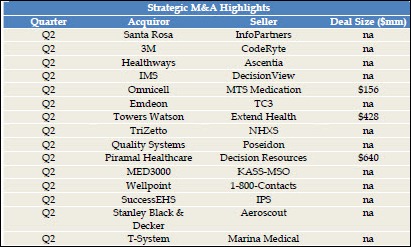
Acquisitions, Funding, Business, and Stock
CommVault beats Wall Street expectations with its Q1 performance: net income of $10.1 million ($0.21/share) compared to $3.1 million last year on revenues of $111.3 million, up from $91.5 million.
Merge Healthcare announces Q2 numbers: revenue up 13%, adjusted EPS $.02 vs. $0.06, beating earnings estimates by a penny.
Sales
The Canadian Centre for Addiction and Mental Health selects Cerner Millennium as its clinical information system.
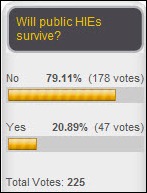
North Carolina HIE expands its relationship with Orion Health with the implementation of the company’s Health Direct Secure Messaging. The HIE went live in April 2012 and 70 providers have signed up, with the next phase being rollout of Orion’s EMR Lite. NC Direct is free for NC HIE participants and $100 per year per mailbox otherwise.
St. Louis-based Mercy chooses Humedica MinedShare as the Epic-integrated clinical intelligence solution it will use to manage population health for its 31 hospitals and 200 hospitals.
People
Lifespan (RI) names Eric Alper MD (UMass) as information systems medical director, charged with overseeing the development and implementation of clinical applications for the health system.
Amanda LeBlanc (Encore Health Resources) joins CTG Health Solutions as managing director of marketing and communications.
Announcements and Implementations
Yavapai Regional Medical Center (AZ) implements Cerner.
Christus St. Vincent Regional Medical Center (NM) goes live on the second phase of its Cerner implementation with the addition of CPOE and documentation for physicians, nurses, and ancillary care providers.
The VA system in western New York announces its participation in the HEALTHeLINK HIE as part of the VA’s Virtual Lifetime Electronic Record Health Communities Program.
Vocera announces the availability of its B3000 Communication system in France and introduces the Vocera Secure Messaging application for tracking messaging communications.
Jacksonville Medical Center (AL) goes live on CPSI.
E-prescribing system vendor NewCrop will incorporate interactive drug services from PDR Network into its platform, allowing its users to receive updated drug information, safety alerts, and regulatory and liability messages at the point of prescribing.
Caradigm (the GE-Microsoft joint venture) announces GA of Vergence 5, the latest release of its single sign-on and context management platform for healthcare.
Iowa Medicaid says its integrity program saved the state $30 million in its second year of operation, bringing the total to more than $50 million. Optum administers the program that analyzes provider claims for overcharges due to upcoding, unnoticed private insurance coverage, fraud, and simple math errors in bills.
Technology
The FDA clears Proteus Digital Health’s ingestible sensor, which works with a companion wearable patch and mobile app to monitor medication adherence.
The DoD and VA release PE (for prolonged exposure) Coach, a free smart phone app to assist service members and veterans with PTSD.
Other
Minnesota achieves the highest rate of e-prescribing use in 2011, with 61% of prescribers routing prescriptions electronically. Massachusetts and New Hampshire had the highest physician adoption rate at 86%.
The New Orleans paper reveals that two-thirds of the full-time physicians working in Louisiana state prisons have been disciplined by the state medical board for issues that include pedophilia, substance abuse, and dealing methamphetamines.
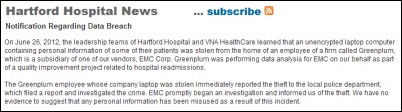
Hartford Hospital (CT) and a home care group announce that information about 10,000 patients was contained on a laptop stolen from an employee of Greenplum, a “big data analytics” vendor and division of EMC that was doing readmission analysis for the organizations. The laptop was not encrypted.
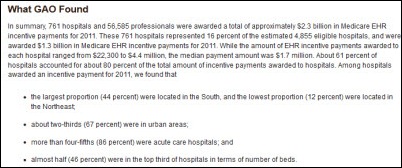
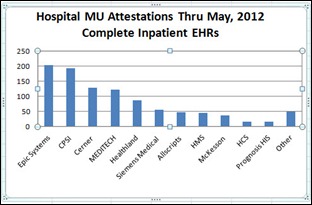
I’m always skeptical of the Meaningful Use attestation numbers, so here’s an example that Meditech sent over in response to some of our recent posts. Inga’s analysis of numbers provided by CMS showed Meditech with around 120 hospital customers attested through May 2012. Meditech’s official number is 431, and even if mega-customer HCA is counted as only one hospital, they’re still at 271. That would place Meditech at #1, far above CMS’s #1 Epic, except that maybe CMS has their numbers wrong, too. I personally don’t think the number of attesting customers means much and this makes me even less interested in the vendor totals.
Physicians and experts testify to a House subcommittee that small practices are dropping like flies, with physicians moving to employed positions because of declining payments and increased reporting requirements. An orthopedist said his group shut down and took hospital jobs after spending $500K on an EMR hoping to reduce cost and improve quality, but the initial savings were eaten up by increased IT labor costs, upgrade fees, and the work required to document Meaningful Use.
Weird News Andy dubs New York Mayor Michael Bloomberg as “Dr. Bloomberg” after his push for hospitals to discourage new mothers from using canned baby formula instead of breast-feeding. WNA adds that he assumes the newborns won’t be allowed to have 32 ounce Big Gulps, either.
Sponsor Updates
- Wolters Kluwers executive board member Jack Lynch discusses the emergence of “compliance clouds” during the company’s Half Year Media Roundtable meeting in Amsterdam.
- Informatica gains partner support for its latest release of Informatica Cloud.
- Impact Advisors earns the highest ranking in KLAS’s HIE consulting report, specifically identified as the only fully rated vendor providing HIE advisory and technical work.
- DrFirst Chief Strategy and Privacy Officer Thomas Sullivan testifies at an ONC hearing on identity-proofing solutions for the electronic prescribing of controlled substances.
- HIStalk sponsors earning a spot on Modern Healthcare’s Best Places to Work in Healthcare in 2012 include Aspen Advisors, DIVURGENT, Encore Health Resources, ESD, Hayes Management Group, Iatric Systems, Impact Advisors, Imprivata, Intellect Resources, Intelligent InSites, maxIT Healthcare, Santa Rosa Consulting, and The Advisory Board Company.
- Allscripts, Beacon Partners, Cumberland Consulting Group, ESD, Merge Healthcare, and The Advisory Board Company receive the Healthcare’s Hottest companies designation by Modern Healthcare.
- eClinicalWorks and Intelligent Medical Objects host webinars to introduce eCW IMO Problem IT Smart Search for ICD-10 coding.
- United Hospital System of Kenosha (WI) renews its licensing agreement for Streamline Health’s Enterprise Content Management Solution.
- MED3OOO customer Family Healthcare Network (CA) receives over $500,000 in EHR incentive payments.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.



































































We should be concerned that the forthcoming MINIMUM cybersecurity standards will lead to many organizations being even less prepared than…