Ron Remy, MBA is CEO of Mobile Heartbeat of Waltham, MA.

Tell me about yourself and the company.
Mobile Heartbeat is in the clinical communication and collaboration space, which is being renamed as care team collaboration as the market is changing. We’ve been in the business since 2011 with our existing product line. I’ve been the CEO since 2013 and been involved since 2011. We were acquired by a public company back in 2016 and have been a part of them for almost seven years now. We are fully deployed in the market with over 260,000 monthly users, predominantly clinicians in acute care facilities. We have been on premise and are in the process of coming out with our first cloud-based platform.
I have a background in electrical engineering, which is surprisingly pretty useful in the software space, and a minor in computer science, which back in the day was an interesting field that was relatively new.
How did the business change with the pandemic?
It was fascinating, particularly in the first six months. Clients that were fully deployed were really grateful that they had deployed communication capabilities in their facilities. Clients that had partially deployed were calling us and asking us to speed up the process of getting them fully deployed, which was challenging because getting on site in some of these facilities for our staff was not an easy task pre-vaccination. Those that were in the process of evaluating new technology acquisitions — not just us, but anything that was new technology — those opportunities just ground to a halt because there was so much they had to do.
Our existing clients were extremely happy, and we made sure that we were there to support them to keep things running. It was a core to them being able to treat patients effectively. For those that were partially deployed, we sped up the deployments. They saw the value from the places that they had rolled out smartphones and our software, and they wanted it everywhere. Those that hadn’t made a decision to deploy this new technology just stopped. They couldn’t take on any new projects. That lasted until a year or 18 months ago and was a pretty consistent trend.
It works like this in our experience. A health system decides to deploy smartphones to its staff. They do analysis to determine how many smartphones to buy, how many units they have, and how many folks they want to give access to this technology. They put the phones in place and then look at one of the communication companies, Mobile Heartbeat being one of those, as a vendor of choice. They deploy, because the first tool that they need is a communication tool. That’s obvious. Immediately after the tool is deployed, they start seeing some pretty good return on their investment. Then they look at other capabilities that they can put on their smartphones to enhance the clinician experience, improve patient care, or decrease errors.
It’s fascinating how our clients have integrated different pieces of technology onto these smartphones, using Mobile Heartbeat software to glue them all together. That trend is accelerating, and we have clients that are making these integrations on their own. We don’t even know that they’ve integrated other products into our own because they have become so good at it. I’m excited about the trend of the in industry going forward because clients see this as a future-proof path to providing better care and providing a better experience for their clinicians. That’s what we set out to do back in 2011, and we are seeing that come to fruition. The pandemic accelerated how clients pushed their smartphones to their highest capability.
We saw during the pandemic that clinicians and then patients were untethered from traditional locations. How has that changed your strategy?
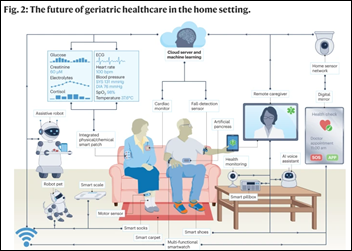
It changes it in one big aspect for us, which is that we’ve supported the telecare side of telehealth predominantly. For remote nursing or central monitoring, we’ve become the endpoint for those folks that are doing the remote monitoring to message and communicate with the actual point-of-care caregivers.
Take a central monitoring scenario. You have a technician, nurse, or other clinician who is monitoring a number of patients. Suddenly, they notice something about a patient. They have to immediately get that information to the caregiver who is most likely to provide care for that specific patient. They need to communicate quickly and efficiently, and they can’t be searching around for the right person.
In that scenario, the technology that Mobile Heartbeat produces has become a critical component of those systems. That has been the biggest change. The pandemic has sped up those telemonitoring scenarios. I believe that virtual nursing will be the next big trend, providing nursing care without being in the room all the time, but still with a presence in the room.
What have you learned from analyzing how caregivers use messaging and mobile devices?
The first thing that you learn early on in deploying smartphones and communication capability is that you need to think of it as an enterprise product. Not just from a product standpoint, but from a value standpoint for an acute care hospital or system. Metcalfe’s Law was proposed in the early 1980s by Bob Metcalfe, one of the co-founders of 3Com. His law states that the value of your communication network is equal to the square of the number of endpoints on that network. It dates back to the days of fax machines being replaced by a 3Com network. The value of your network grows exponentially as more people can use it to communicate with one another.
A healthcare system’s investment in communication technology becomes exponentially more valuable, and your ROI increases, as you put more people on the network to communicate with one another. You‘ll see challenges if you only do one unit versus the entire hospital so that the whole hospital can communicate with one another. That’s the biggest lesson that we got from the earliest days of Mobile Heartbeat. We are seeing this come back 10 years later as we talk about new technologies going out into the hands of clinicians, making sure that that network grows and includes the entire continuum of care.
It’s not just those inside the hospital. Now it is the at-home capability of a physician who may be a referring physician and isn’t part of the hospital system. How do we bring them into the communication network? You’re going to make a big investment, so you want to make sure that the ROI is as high as possible for your system. You have to pick carefully which projects to fund, the ones that have real value to your patients and your staff.
When do collaborating caregivers prefer a synchronous voice call versus asynchronous texting?
That differentiation started immediately with our first customers. Our analytics tell us who is who is texting who, who is calling who. We can see it over time. Put an asynchronous communication system in place in a hospital, with smartphones and Mobile Heartbeat software, and the communication paths won’t be what you expect at all if you’ve enabled other parts of your facility. Those paths will be much broader than you expected. It’s not just physician to physician or nurse to nurse. There’s a lot more people involved, such as pharmacy, respiratory, and PT, that are key parts of the care of a patient.
The second thing you start seeing is that the trend to move to asynchronous happens immediately. People realize the value of sending you a message to read when you have time versus a phone call that interrupts whatever you’re doing. The value of asynchronous communication is immediately recognized, but it has a fascinating secondary effect, which is that once people are comfortable asynchronous communication — a phone call, a synchronous outreach via phone call — the recipient knows that that is valuable. They know that that’s important, because otherwise it would have been a text. The likelihood of the recipient picking up the call and actually starting a conversation is much higher because there’s a confidence level that you’re only calling me if you need me right now.
That has an improvement on your overall communications capacity and the way people use the different tools and the best path. Asynchronous if you don’t meet need me immediately, synchronous if you need me immediately. Your chances of the communication being correct and actually occurring is much higher. I found that fascinating early on, watching the phone calls drop and the text messages grow. Then going back six months later and interviewing the clinicians, who say, those phone calls are still critical to us. When something is really needed, someone hops on the phone and I always answer, where before I would let things go to voicemail. That’s a fascinating change in human behavior based on new technology.
Are messages escalated or alerted if they aren’t delivered or answered?
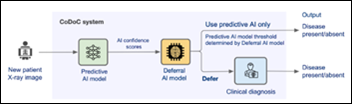
The alerting capability is pretty much in place today. What will be fascinating in the future is the ability of AI tools to make sure that these orders workflows are done, they’re done in the right order, and that people are reminded if they’ve not completed.
The digital playbook for a stroke stroke patient is different from hospital to hospital. If everyone is in a channel that has access to the digital playbook, it will be followed. You’re making sure that everyone takes care of their steps in the playbook, and you’re using some assistive AI technology to predict what the next step should be. That’s a big plus and that is a big win for the patient, the hospital, and the healthcare system. It’s a really good use of new artificial intelligence technology. I think we will see that coming relatively soon.
Alerting when things don’t happen properly, if messages don’t get sent, is already pretty much there. It’s the keeping track of what should be done in a playbook manner for each patient and for each condition that will be the future.
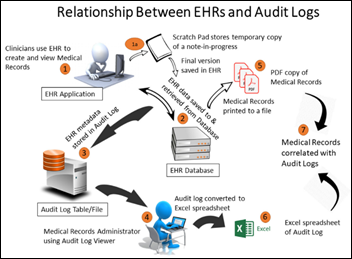
Are health systems doing anything to integrate messaging with the EHR?
Almost everyone stores the actual messages, archiving them or keeping them in a offsite facility. They choose how to long to hold this. But very few want this to be a part of the medical record, for good reason. In many cases, these are conversations happening between clinicians. It’s like a hallway conversation. Would you really want every hallway conversation written into the medical record?
There are places where you need to be written in, and other places where you need it to be accessed down the road, but you’re going to clutter up a medical record with an awful lot of chatter around a patient if you wrote every conversation into the record. That being said, you may want to access it at a future date, so you need it to be archived, but you don’t want to bring back hundreds of pages of conversation in the medical record around the patient. You’re asking people to search through a lot of data for limited value.
Phone use went from calls to texts and then to two-way video like FaceTime. Are you seeing health system demand for that video capability?
There is demand, and we are moving down that path. The big use case is, “I need to show you something, but you’re not with me at the moment.” That’s the use case of video. You and I are working together. We have a patient or something of interest in common. We are in different facilities across town, you need to show me something, and I can’t be there standing next to you.
The video will give that opportunity. You have a smartphone in your hands that has camera capability. I can receive it. I can look at something with you on using the voice side of it. I can illustrate what I am seeing, ask for an opinion, or let someone know of something that will interest them that they should be aware of.
The challenge is that video is bandwidth heavy, and wireless requirements in healthcare systems are growing exponentially. If you’re going to add a lot of video onto your network,you’ll have to do some physical infrastructure planning to support it.
You have an unusual perspective in being a vendor that is owned by hospital operator HCA. How is the business environment changing for digital health companies?
I’m fortunate, and our team here is fortunate, to see how our parent company operates and how they make decisions around not only acquiring technology, but also business decisions around staffing and growing the business into different areas.
One trend that doesn’t seem to be going away, both in our world but also in that of our customers, is the pressure on staffing and cost. Staffing costs are going up, and you have a couple of choices to try to address that. One is to hire more staff, which is difficult because the people just aren’t there. If you look at the number of nurses entering and leaving the profession, you have a potential 10 to 20% staffing gap in five years in just that individual role alone. Roll that across your whole system and that’s a pretty big gap.
You can’t hire your way out of the problem, so what can you do? You can decrease the quality of patient care by assigning more patients to each caregiver, but that’s not a very good thing when the quality of care begins to slip. Now you look at other ways of mitigating this issue, and technology plays a role. It’s not a panacea. It won’t solve every problem. But it certainly serves a role, along with making operational changes.
If you can reduce operational challenges using technology — make the clinician available to the patient more frequently or cut down their non-productive time so that they are practicing medicine instead of standing in front of a workstation on wheels – you have a chance of solving this problem. We are looking at the operational side of the clinician’s world and how our communication capabilities can improve it. How can we make them more efficient? How can we increase their job satisfaction? How can we increase their time spent with patients and decrease the time they spend on administrative tasks?
Everything we are working on is aimed at that. It’s a problem we see both in our parent company and across the industry. That problem of staff cost and shortages is just not going away.
Comments Off on HIStalk Interviews Ron Remy, CEO, Mobile Heartbeat


























Give ophthalmology a break. There aren’t many specialties that can do most of their diagnosis with physical examination in the…