Monday Morning Update 10/23/23
Top News
Medication management company Cureatr shuts down without notice, blaming a lack of financing and a failed acquisition.
The company acquired SinfoniaRx in March.
Reader Comments
From Tolstoy: “Re: startups. The wave of shutdowns and fire sales is just starting as former stars run out of cash.” Agreed. Companies that ran big early-round raises in a go-go market are just now seeing the invisible investor strings that were attached – the moneyed folk are demanding profitability, growth, and proof that the company’s moat exists and is not drying up. Inexperienced operators, especially first-time founders, are new to a market that values being cash-stingy to ride out the storm. Some will attempt to pivot, which rarely works. The lowest-quality startups will shut down, but most will come hat-in-hand to established companies hoping to sell the business, its IP, or its office furniture at a dismal fraction of now-laughable historic valuation. Meanwhile, the valuation premium for startups versus publicly traded companies is narrowing and founders are packing up their rosy pitch decks being forcefully relocated from the CEO chair to the boardroom. The upside is that the cream floats to the top when irrational exuberance meets reality, so winners will emerge stronger.
From Belzer: “Re: Waystar IPO. Good timing?” It’s hard to say given the long IPO drought and SPAC distraction. The PE-owned company’s string of acquisitions has piled up quite a bit of debt, with the S-1 showing interest payments of $149 million in 2022 on $704 million in revenue, resulting in a $66 million pretax loss. The company was valued at around $3 billion in 2019 when a majority stake was sold. Rumors of an $8 billion valuation floated around last summer when the IPO plans leaked.
From Plowboy: “Re: Henry Schein. We are placing orders by phone while the company keeps its site offline.” The medical and dental supply vendor took its systems offline on October 14 due to a cybersecurity incident, although its practice management software was not affected.
HIStalk Announcements and Requests
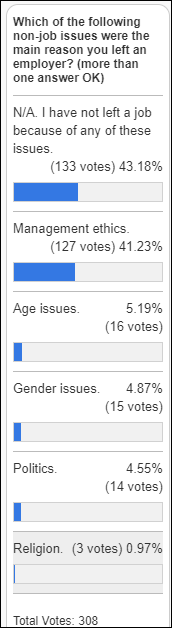
Poll respondents who quit because of non-job issues cite management ethics by far as their most common issue.
New poll to your right or here: Looking back five years, which aspects of healthcare have been significantly improved by technology? I ran this a few years ago, so let’s see how the responses differ.
Webinars
October 25 (Wednesday) 2 ET. “Q&A: What’s new with the NSA? A No Surprises Act update.” Sponsor: Waystar. Presenters: Joseph Mercer, JD, managing director, Marwood Group; Heather Kawamoto, VP of product strategy, Waystar. The No Surprises Act created a lot of change, and those changes are still coming. A panel of revenue cycle experts answer frequently asked questions and offer a concise update on the NSA, including legislative developments, FAQs, and tips for navigating changes.
October 25 (Wednesday) 2 ET. “AMA: The Power of Data Completeness.” Sponsor: Particle Health. Presenters: Jason Prestinario, MSME, CEO, Particle Health; Carolyn Ward, MD, director of clinical strategy, Particle Health. Is your healthcare organization looking to drive profitability and scale quickly? Our experts will explore how comprehensive clinical data can revolutionize the health tech landscape. This engaging discussion will cover trending topics such as leveraging AI and data innovation to enhance patient care and outcomes, real-world examples of organizations leading the charge in data-driven healthcare, overcoming challenges in data completeness and interoperability, and visionary perspectives on the future of care delivery.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
EClinicalWorks announces that it expects to generate $900 million in revenue in 2023, up from the previous year’s $800 million. The company will continue to invest in AI, including ChatGPT integration, an AI-based image model for document management, and RCM improvement.
Weight loss drug startup Calibrate will sell itself to a private equity firm and restructure the business, which recently pivoted from selling prescriptions directly to consumers to having employers offer its services as an employee benefit. The company has struggled with refund-demanding customers who couldn’t get their prescriptions filled due to short supplies, as well as those who found that their insurance wouldn’t cover the high cost of GLP-1 drugs.
Nomad, whose app connects travel nurses with hospitals, lays off employees for the second time this year as budget-challenged health systems reduce their use of expensive travel nurses.
Sales
- The US Defense Health Agency awards Amwell and Leidos a contract valued at up to $180 million to provide a hybrid care platform that will replace MHS Video Connect.
People

Tony Ambrozie, MBA, MIM (Baptist Health South Florida) joins CVS Health as chief digital and technology officer, pharmacy and consumer wellness.

Net Health hires Ron Books (ECI Software Solutions) as CEO.

Matter Communications promotes Paul Berthiaume to SVP.
Privacy and Security

HealthAlliance Hospital (NY) discharges or transfers all of its inpatients and diverts ambulances following a cyberattack. Owner Westchester Medical Health Network says the incident also affected Margaretville Hospital and Mountainside Residential Care Center.
Other
Cedars-Sinai researchers develop an AI tool that can detect atrial fibrillation in people who don’t have symptoms, including in diverse settings and patient populations.
Sponsor Updates
- Inovalon partners with HealthVerity as part of its new Preferred Data Partner Program to advance the use of real-world evidence in research.
- NeuroFlow publishes a new case study, “Prudential Helps High-Risk Disability Claimants Access Support Through Population-Wide Suicide Risk Assessment & Prevention.”
- Surescripts shares a new podcast, “A Recap of NACDS Total Store Expo 2023.”
- Wolters Kluwer announces that its Emmi patient engagement and education solution has received a 2023 Black Book award for highest client/user satisfaction from managed care providers.
- InterSystems partners with Indonesian EHR vendor Zi.Care to provide expert services via the InterSystems Iris for Health – Indonesia Edition data platform.
Blog Posts
- What’s top of mind for healthcare executives now? (Notable)
- Intelligent patient experiences, part 1: How easy it is to use your patient portal? (Nuance)
- Healthcare workforce: Burnout, compensation, and strikes with Elizabeth Ojo on Diagnosing Healthtech (Redox)
- Supporting Med Access by Collecting Digital Patient Consent (RxLightning)
- 4 Reasons to Skip Paper and Switch to Online Incident Reporting Software (Symplr)
- Rev cycle 101 – Healthcare revenue cycle terminology: Denial prevention glossary (Waystar)
- A Provider’s POV: Can Technology Help Us Be Better Patient Advocates? (CereCore
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.






























The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en