G. Cameron “Cam” Deemer is CEO of DrFirst of Rockville, MD.

Tell me about yourself and the company.
I was a latecomer to healthcare IT. I started my career in the ministry and didn’t get into this side of the industry until the early 1990s. I started working with PCS Health Systems in Scottsdale, Arizona. I did about a decade with PBMs, worked with NDC Health for a couple of years building what became Surescripts later, and then joined DrFirst in 2004.
When I joined DrFirst, I would have called it an e -prescribing company, which would have been easy to understand. But since then, we’ve developed a much broader vision. Today, the company is about making sure that patients have their best outcomes through their medication therapy. We do that through offering technology platforms that help providers work with patients around things like electronic prescribing, medication reconciliation, and population health. Our fastest-growing platform addresses patient adherence to therapy.
How has the original vision of e-prescribing expanded?
I had a front-row seat in the early days of e -prescribing. We did some seminal piloting of e -prescribing when I was with PCS. It has gone from essentially a record of what would have been written on a piece of paper to being a more fully informed decision support system.
As an example, we connect to all of the state PDMPs, the controlled substance registries, so that a doctor can consider that information at the same time they are writing the script. They have a much better idea of whether someone is drug seeking or legitimately coming onto therapy. Similarly, a real -time benefit check allows them to understand exactly how much the patient is going to pay. Then, bringing other information in from outside, such as formulary status and electronic prior authorization. Essentially e -prescribing has become an ecosystem as opposed to just a replacement for the prescription pad like it was originally started.
How does seeing cost and insurance coverage at the time of prescribing improve patient outcomes as well as patient satisfaction?
We view it as two parts. There’s what happens in the doctor’s office when they are prescribing therapy, and then what happens after the patient is released back into the wild to act on the prescription.
In the physician’s office, we think that real -time benefit improves compliance with therapy, because it finally gives the physician a real idea about the impact of what they are prescribing. How much is this drug going to cost versus that drug? Or is therapy going to be delayed because you have to go through a prior authorization if you choose this therapy versus that therapy? It is giving the physician real insight. They already know what they want to write, so now they get insight into what the outcome will be from the patient’s perspective.
The reason that we started working downstream from there, on what happens to the patient after they walk out of the office, is that we often found that the providers maybe didn’t have time, or maybe they weren’t focused enough on the extra information, and weren’t necessarily helping the patient make a decision that would be ideal for the patient to then go fulfill the therapy.
We try to hit the patient immediately after they leave the doctor’s office with more information. What prescriptions were written? Where are they going to get them filled? We have a call to action to pick up the prescriptions. We provide financial assistance information if the physician has chosen a drug that is extraordinarily expensive for the patient. We give the patient the tools to make up for what may have been missed when they were in the provider office, or to reinforce the decision the provider made.
Have coupon-type programs, such as manufacturer assistance programs or GoodRx, made displaying patient prices more complicated?
Systems have come a long way in being able to present all that at once. From a provider perspective, they wouldn’t be perceived as a set of different decisions. At least for our system, it’s all combined into one decision point, so the physician can consider them all at once. From a patient perspective, it would only really be one thing, because their therapy has already been decided at that point. Now they just have the one decision to either pick it up or don’t pick it up. The financial incentives can help them with the “pick it up” decision if they are available.
Has the prior authorization process, which everyone seems to agree is burdensome, improved?
Boy, I agree that it needs to be fixed, so I’m on that page. Prior authorization is widely recognized as a coping mechanism, a way to stem the flow of products that the payers feel are expensive. They don’t necessarily want to cover the therapy unless they are pushed to do so.
I’m not sure how much incentive exists to truly fix it. Truly fixing would look like the barriers make sense and they are readily overcome. What’s going on in the industry right now to fix it is that when the physician is confronted with a screen they have to fill out for the prior authorization, can we just grab that information out of the EHR, fill in the form, and let the physician have very little work to do to send that PA?
The whole thing is counterintuitive. They are intended as a barrier. Making it easy makes the barrier less effective. It’s an interesting problem that I’m not sure we are really solving yet.
If the prior authorization is a prescribing speed bump that payers hope will discourage the prescription, what interest would payers have in solving the problem? Why couldn’t they look at a prescriber’s history, even with AI if needed, and bypass the front-end work unless that provider is an outlier in deviating from accepted norms?
That would be a fascinating way to handle it. I’ve actually not thought about that before, but with machine learning and AI, you should be able to analyze, give the doctors some kind of performance score, and put a lower set of barriers in front of those who are good actors. There would be a lot of discussion about what equals a good actor from a provider perspective. I imagine there’s a wide range of thought on that.
An interesting development is Lilly’s program, where they are to some degree working around these kinds of restrictions with some of their new drugs for weight control and diabetes management. They appear to be sidestepping the process and maintaining pricing control rather than throwing rebates at formulary status.
Rather than being told that your drug will go off formulary unless you can bring this price way down from a PBM perspective and that you will be faced with a prior authorization hurdle that will be a giant pain to get people on, they are essentially setting up a parallel system. Patients can have relatively simple access to the drug and they can help manage the cost for the patient without causing the kind of disruption to everybody that a massive rebate program causes. Good or bad, I think it’s a really interesting approach that was creative on Lilly’s part.
It’s also interesting that they are working with third-party companies for telehealth prescriptions and pharmacy fulfillment. Will other drug companies follow suit?
I want to reinforce that what they have effectively done with those third parties is sidestepped the plan design. Patients are being asked to go outside of the health plan that they are paying for, and instead participate in this other parallel program that’s been set up for these drugs.
That will make it a little more difficult for other drugs. Not many drugs have the demand profile of the weight loss drugs. If your expensive drug is less in demand, there’s probably less incentive for the patient to step out of their plan design. I’m paying for this insurance, I should use it, that kind of psychology, so I wouldn’t think that everybody will be in a position to follow suit. But it’s a creative model when the drugs fit the profile that would make this work. It’s brand new, so we don’t know yet.
Lilly is also potentially keeping some of the revenue that would have otherwise gone to PBMs or pharmacies while gaining control over pricing. Is there a DrFirst technology implication for manufacturers that sell drugs directly with patient discounts?
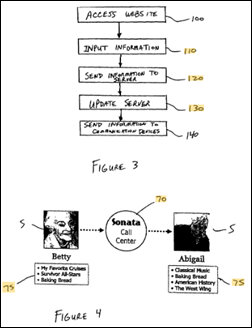
One of the things we are excited about is our ability to engage patients, let’s say five minutes after they leave the doctor’s office. Because of our position in workflow on the prescriber side, we actually know when the electronic prescription has been sent. At that point, we can reach out and engage a patient. We are four and a half million patients a week touching about one out of every four new prescriptions. Our scale has gotten fairly large because of the number of EHRs that we work with.
As a result of that, we are in a position to work with somebody like Lilly to be an entry point for patients into their program who might not know about their program. In the event that the physician bypasses whatever opportunities Lilly has provided for them, we have an opportunity to talk to both the provider and the patient because we sit squarely in that workflow. So yes, I hope we can be a part of that. I really enjoy these creative solutions to persistent problems around cost in healthcare.
What is the state of medication history and its delivery directly into the clinician’s EHR workflow?
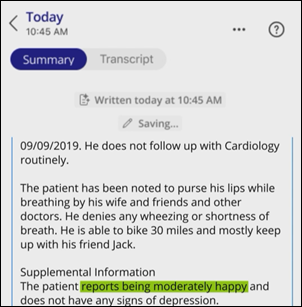
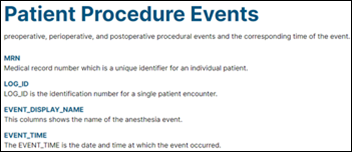
I would say not greatly improved. There may be broader access to records now, a more complete patient record. But not much has happened to clean up the dirtiness of the data, this kind of shady underbelly of the whole data space. We spend a lot of time on data optimization because we find that the data feeds still are not semantically usable by the people who receive them.
As an example, somebody who creates a record might be using Latin abbreviations, and somebody who is receiving it might use English abbreviations. No matter what abbreviations they use, they can still write the sigs [abbreviations for instructions] differently and you can make millions of different combinations out of any given sig, depending on how the one system prepared it and how the other system wants to receive it. A big part of our business remains matching those data feeds up. How do you massage the incoming feed to make sure that all the fields are discrete and all the data elements are ready to be imported into the receiving system so that somebody doesn’t have to manually retype it?
That kind of data optimization is still missing from the industry and still needs to be handled independently before a system can receive the records. The bottom line is that I would say that there’s availability of a lot of records now, more than there’s ever been, but they are still just as dirty as they were years ago and still need that cleanup.
What role do you see for AI in your business and the industry in general?
We’ve been all over AI for data optimization for at least six years now, and it makes a huge difference. Machine learning and AI provides a much more elegant and complete solution than, say, a table of substitutions. You can only anticipate so many errors that a person might make, and the ability of the AI to sort that out automatically is huge. We end up with much higher rates of cleanliness of the data than are available through traditional methods.
We call that augmented intelligence, meaning that we do the cleanup, but then we provide the clinician with both the original and the cleaned up version. If they’re good with it, they can just say, “That’s good.” Otherwise, they can tweak it if it’s incorrect in some way. We put most of our focus on trying to find practical problems in the workflow and provide an efficient solution so that providers can get more work done and get away from that burned out feeling of having to retype everything.
What are the company’s near-term priorities?
One of our major business lines is providing e-prescribing platforms for EHRs. We serve over 300 EHRs in that way. A major change is coming in 2027, when Surescripts is going to implement the 2023 version of the SCRIPT standard. We expect other changes to come along with that. That will make everybody stop and do major development in their systems again. A big part of what we’re going to do over the next few years is work on helping people with that conversion. Some will decide that this is the last straw and that it’s not worth maintaining their own e-prescribing channel any more and we’ll be able to do integrations with additional companies. It will be a major focus to make sure that the industry is ready for this big change in coming in 2027 around prescribing standards.
Another major focus for the company is to continue to drive our adherence programs. We believe that we will eventually get to one out of every two new scripts, and when we have that level of aggregation, we will be meaningfully able to address things like access to specialty scripts. The industry is moving towards specialty drugs at this point, and those have all kinds of access challenges. We’re going to be spending a lot of time cleaning up those processes for the industry and making sure that patients can get on therapy quicker and stay on therapy for specialty.
The last thing is perhaps a little controversial, but we believe that it’s time to take a hard look at what happens after a script leaves the doctor’s office before it gets to the pharmacy. We’ve been working since the 2000s under a 50-year-old technology, the switching network that we use to move scripts between doctors and pharmacists. It’s a lowest common denominator solution that lets everybody have a level playing field, but doesn’t give anybody an opportunity to innovate and try new models.
We’re going to be breaking out of that mold over the next few years. We are standing up a capability to provide real innovation in this space with a broader set of data exchange between providers and pharmacies to enable better business flows on both sides of the equation. Just think about when you write a script, knowing that the drug is in stock at the pharmacy you are writing it to. Or if you’re on the pharmacy side trying to do some primary care type functions, think about what it would mean to get a patient record at the same time the script comes to you. That kind of innovation isn’t available today. We’re going to make that a part of how the industry works going forward.
I got into this industry in 1992 and have been talking to pharmacists this whole time. They are always trying to find that a breakthrough to be able to work at the top of their license, but never getting there. We’re developing our pharmacy channel to get closer to pharmacy. That takes a while. It’s a big area, and you need to build some trust. But I’m hoping that we can finally help them practically get there where they’ve really struggled before. Since we have theses massive EHRs behind us on one side and pharmacy customers on the other side, we believe that we can finally bring them together so that we get this real collaboration around the patient that has eluded the industry for a long time.
Comments Off on HIStalk Interviews G. Cameron Deemer, CEO, DrFirst
































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…