EPtalk by Dr. Jayne 1/11/24
Masks are back on at my local hospitals. Our area is seeing a surge of COVID, influenza, and RSV patients. We’re seeing full intensive care units. Nursing exhaustion is approaching pandemic levels.
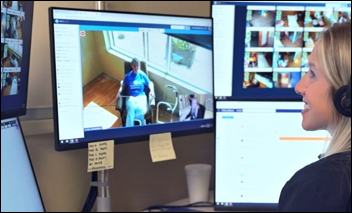
Across the US, hospitals are experiencing staffing challenges, which often cause beds to be unavailable because they aren’t staffed. This rolls downhill in the hospital, landing in the emergency department that has to board the patients until beds are available. In turn, this can back up ambulances, which leads to delays in 911 calls. For my friends working in EMS, this is starting to feel a lot like 2020, and in my community, the COVID-related hit to EMS staffing is still present.
If you’re on the healthcare IT side and the clinical staffers that you are interacting with seem frazzled and distracted, it’s because they are. One of my ICU nurse colleagues commented, “It’s like people forgot what we went through and just don’t care about healthcare workers any more.” Let’s remember to wash our hands, stay home when you’re sick (or wear a well-fitting mask if you can’t stay home), and look after each other. We’re all in this together.
I’ve started working on a project that involves an area of clinical informatics that I haven’t worked on in some time. To get up to speed with the vendor landscape, I’ve been visiting lots of websites to view white papers and customer case stories. Maybe my brain is just used to operating in an older way of working, but I find myself increasingly annoyed when companies have decided that the only way they’re going to share information on their websites is through videos. Some of us absorb more through reading actual words. Of course, others are more visual or auditory learners and might do better with that kind of content.
For me, it’s often a time issue. I can read much faster than most video presenters speak, which means that when there is only video content available, I tend to perceive the sites as not being a good use of my time. It left me wondering what happened to the good old written word and whether it’s just me or whether times have changed and I need to get used to my work taking 50% longer than planned.
A primary care colleague reached out to me today, venting that her organization has yet to configure the EHR to allow physicians to submit the G2211 billing code that went into effect on January 1. That’s an add-on code that allows physicians to submit charges for the time they spend building longitudinal relationships with patients and addressing patients’ issues over the long term. CMS describes the code as billable for “visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed healthcare services and/or with medical care services that are part of ongoing care related to a patient’s single, serious condition or a complex condition.”
The nature of the relationship between the patient and the physician is the factor that determines whether the code should be used. It’s worth around $16 when billed for Medicare patients, so it’s not designed to drive significant revenue, but rather to offset some of the valuable whole-person care that is provided by primary care physicians. Medicare’s documentation about the change says that the typical primary care physician who has Medicare beneficiaries in their patient panel will coordinate care with 229 physicians in 117 disparate practices. If it hasn’t yet been added to your EHR workflows, your clinicians are missing out.
The US continues to have supply and demand issues with stockpiles of personal protective equipment (PPE). A recent AP report explored the fact that states that had scarcity of supplies during the high points of the COVID pandemic are now dumping PPE at an alarming rate. Ohio has auctioned off nearly 400,000 protective gowns and has thrown away 7 million gowns along with countless masks, gloves, and other supplies. States are having to determine their go-forward strategies for supply stockpiles and preparation for potential disasters.
The amount of materials that is being shredded, recycled, or destroyed is simply staggering. Georges Benjamin, MD, executive director of the American Public Health Association, mentioned that our “bust-and-boom public health system” creates waste as well as lack of preparedness. Many states didn’t respond to the AP’s request for information, so it’s hard to know exactly how large the problem might be.
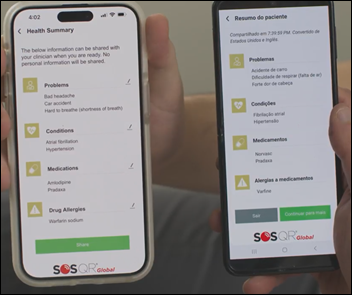
As a CMIO, I’ve worked on a number of projects around health literacy. I would bet that most people in healthcare IT don’t understand the level of understanding of the average patient. For written communications, we need to focus our writing at roughly the fifth-grade level to ensure that patients will be able to understand any instructions we provide. Organizations have also made significant efforts to provide documents for as many patient-preferred languages as possible.
I was excited to see this article that looked as the association among hospitalizations, emergency department visits, and health literacy interventions. Researchers concluded that patients who read patient education materials and summarize their understanding back to the care team are 32% less likely to be hospitalized and 14% less likely to visit the emergency department. Additionally, there was an association with overall declining health costs in patients who received the intervention. The study was performed using subjects that were part of an employee health plan, so it’s not clear if results are generalizable to all patients. Thanks to Healthwise for including this study in their blog, otherwise I would likely have missed it.

The Consumer Electronics Show is upon us, and Garmin is finally taking a giant leap forward in the realm of wearables by introducing a women’s heart rate monitor that clips onto a sports bra and doesn’t require a separate strap. For anyone who has had to deal with a heart rate monitor strap interfering with your bra, this is a welcome addition. The HRM-Fit strap retails for $150.
What are the best and worst things you’ve seen coming out of the Consumer Electronics Show? Leave a comment or email me.

Email Dr. Jayne.






































Give ophthalmology a break. There aren’t many specialties that can do most of their diagnosis with physical examination in the…