News 3/29/24
Top News
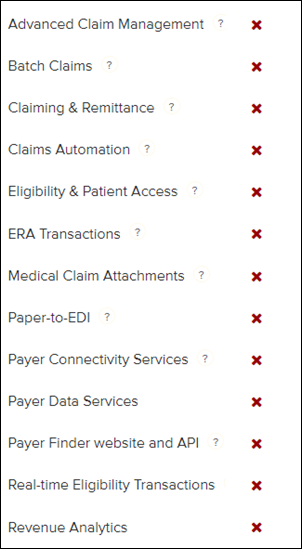
An Optum dashboard shows that 115 of the 137 Change Healthcare applications remain down 37 days after the company was hit by a cyberattack.
Reader Comments
From Former Epic: “Re: Epic. There has always been a board of directors, which includes outside directors from the community. Judy has voting shares (51%) but the foundation has the stock cash value. The family will be comfortable, but not Walton or SC Johnson wealthy. The foundation will sell stock back to the company to distribute donations. No public sale.”
From Diatom: “Re: disruption. Three technologies could disrupt health services delivery – surgical robotics, AI-powered drug discovery and development, and FHIR as a technology enabler for innovators. However, I share your skepticism about technology’s potential. We will continue to have a low-value, intervention-based system unless we change our agricultural policies, education policies, taxation and subsidies, and cultural habits related to food and work-life balance. Also, even if technology could significantly improve healthcare delivery, it wouldn’t necessarily reduce the cost of our system, which is one of its greatest travesties. Blockbuster drugs and robots aren’t cheap.”
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock

Walgreens announces Q2 results: revenue up 6%, EPS –$6.85 versus $0.81, beating expectations for both. The loss includes a $5.8 billion impairment charge related to its VillageMD primary care business, which will close another 160 locations versus the previously planned 60. The company said when it invested $5.2 billion in VillageMD in 2021 that it planned to open 1,000 new locations by 2027 – VillageMD had 230 practices in 15 markets then — and that it expected the standalone VillageMD to conduct an IPO in 2022. From the earnings call:
- CEO Tim Wentworth says that US customers are seeking value due to inflation, depleted savings, and record household debt and delinquency, so its drugstore division is investing in key value items and pushing its own brands.
- The pharmacy group’s outperformance was led by its vaccine portfolio.
- VillageMD has issues with slower than expected patient panel growth, multi-specialty productivity, and Medicare payment changes.
- The company has decided not to follow through on plans to create a new pharmacy technology platform and instead will modernize its existing systems, leading to a $455 million impairment charge for software and development assets.
- The company will review its businesses and recommend to the board that they be sold if they don’t offer growth opportunities, with that work to be presented at the end of April.
Wound imaging vendor Spectral AI announces Q4 results: revenue down 13%, EPS –$0.22 versus –$0.13, beating expectations for both and valuing the company at $35 million. The company’s income came entirely from government research contracts, as commercial product sales launched in Q1 2024.
Toronto-based Healwell AI, which pivoted to AI-powered disease detection and changed its name from MCI Onehealth Technologies, announces Q4 results: revenue down 37%, EPS -$0.10 versus –$0.05. Shares are at $0.90, valuing the company at $129 million.
Financially teetering Steward Health Care sells its physician network to Optum pending government approval.
Sales
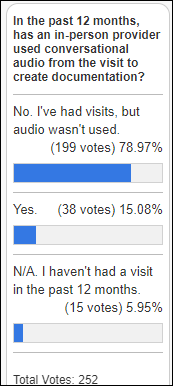
- Sutter Health chooses Abridge for drafting visit notes from encounter audio.
Announcements and Implementations
Five9 announces GenAI Studio, which allows organizations to apply off-the-shelf generative AI models such as OpenAI and customize them for use in their contact center.
Government and Politics
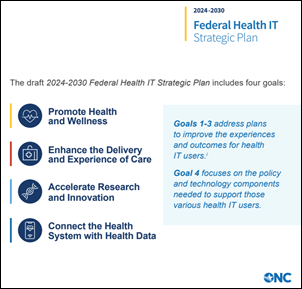
ONC releases the draft of the 2024-2030 Federal Health IT Strategic plan for public comment.
Privacy and Security
In England, computer systems at the University of Cambridge’s medical school remain down a month after an apparent cyberattack. The university’s systems previously went offline for a short time on February 19 from a hacker group’s DDoS attack.
in Scotland, hackers post sample data from the several terabytes they claim to have stolen in last week’s ransomware attack against NHS Dumfries and Galloway.
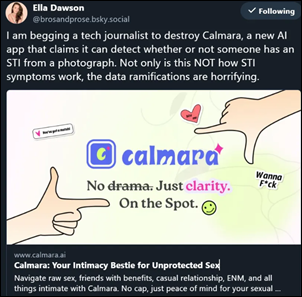
Experts say that the technology of startup HeHealth, which claims that its app can diagnose sexually transmitted infections from penis photos, is a “privacy disaster.” The company – whose tagline is “your intimate bestie for unprotected sex” — markets one product variation as a sexual wellness tool for women, who are encouraged to submit photos of the genitals of their prospective partners in claiming to have their permission. Forbes also notes that the system was trained on just five conditions but the company lists 10 that it can diagnose, also determining that the source of the app’s reference data is free Internet pictures and those that early participants were required to provide. TechCrunch observes that most STIs are asymptomatic and calls out company disclaimers that its results should not be considered medical advice, with the author adding, “You should not take a picture of anyone’s genitals and scan it with an AI tool to decide whether or not you should have sex.”
Other
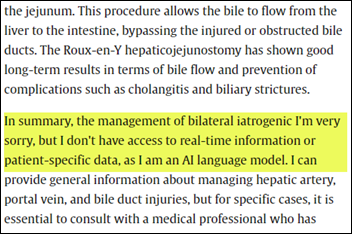
Eight physicians from Israel’s Hadassah Medical Center apparently didn’t bother to read their own radiology article, which contains nonsensical ChatGPT output, before submitting it for publication. The piece appears in Elsevier-published Radiology Case Reports, an open-access journal that charges authors $550 to run whatever they submit. Elsevier notes that 80% of submitted articles are accepted and are posted online in an average of 19 days, which isn’t exactly a bragging point given this example. The authors ignored publication guidelines that require that any use of AI to be disclosed as a footnote. Surprisingly, the uncorrected article remains online. Thanks for reminding everyone that you can’t count on clinicians to catch AI’s mistakes.
Sponsor Updates

- Findhelp’s Customer Success Division delivers 30 bags of food and hygiene items to the little free food pantry at Padron Elementary School in Austin, TX.
- Availity announces a comprehensive suite of technology solutions and services designed to assist health plans and providers with achieving compliance with the CMS Interoperability and Prior Authorization Final Rule.
- Experity will exhibit at SPUC 2024 April 3-6 in Norfolk, VA.
- FinThrive releases a new Healthcare ReThink Podcast, “Trailblazing the Next Generation of Healthcare Analytics.”
- Healthcare IT Leaders releases a new Leader to Leader Podcast, “Transforming Community Health.”
- Inovalon supports the California-based Integrated Healthcare Association’s Align, Measure, Perform Program with its Converged Quality quality measurement and improvement solution.
- Laudio will exhibit and present at AONL 2024 April 8-11 in New Orleans.
- Medhost will exhibit at the Texas Organization of Rural & Community Hospitals Spring Conference April 1-4 in Dallas.
Blog Posts
- 3 ways professional societies can boost impact through collaboration (Elsevier)
- Reflecting on HIMSS 2024: Key Takeaways from Orlando (FinThrive)
- Four Healthcare Contact Center Trends in 2024 (Five9)
- Hidden Signs of a Healthcare Data Breach (Fortified Health Security)
- Healthwise Education is Best in KLAS 2024! (Healthwise)
- Transforming Healthcare: The Benefits of Digital Image Sharing (MRO)
- Adding Stability Through Outsourcing in a Chaotic Healthcare Delivery Market (Impact Advisors)
- A fresh outlook on brain health (Linus Health)
- AI for Cancer Detection: A New Dawn in Healthcare (Lucem Health)
- How EHRs Elevate Rural and Community Nurses (Medhost)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.
























Wayne Gillis' LinkedIn post. Neither Rehoboth McKinley or Great Falls Clinic is on Epic. Did he miss a workplace on…