HIStalk Interviews Larry Hagerty, President and CEO, MedAptus
Larry Hagerty is president and CEO of MedAptus of Boston, MA.
Tell me about MedAptus.
Our focus is on the revenue cycle. We develop software tools, information capabilities, and related services to improve charge capture and charge management.
The company is about 10 years old. We’re headquartered in Boston. We have a development office in Raleigh, North Carolina.
We’re trying to eliminate inefficiencies and improve processes in the revenue cycle. Our customers are generally physician practices. The bulk of our product is in professional charge capture, or physician charge capture. We’ve been fortunate enough to be very successful in the major academic centers and integrated delivery systems because we’ve focused on flexibility and configurability of systems and integration with other systems and scalability.
Because we’re in the revenue cycle, clearly a lot of our value-added is in financial return. We do a lot of work in improving the top line of our customers because we’re helping them avoid missing charges. We help them in terms of the efficiency of that as well because we’re automating things that haven’t been automated and streamlining processes and helping them with compliance.
Charge capture sounds easy. Why isn’t it?
It’s a great question. I think that one big reason is that when one knows best what needs to be charged — which is as close to the point of care as you can be — the tools and systems that are in place aren’t really tuned to help you capture that and to manage it. The clinicians are working in a clinical environment. The systems and tools that they’re working with are geared to supporting that activity. The financial systems and administrative systems speak a different language.
A lot of our work is trying to make it easy for the doctors to capture what they need to know from that administrative or billing perspective and make that workflow between the doc and the administrative and coding staff very, very easy. These systems, again, they’re oriented differently. Connecting that and streamlining it is really where we spend most of our time and attention.
The industry is talking almost exclusively about the potential payout of meeting Meaningful Use requirements. How would you coach a physician looking at that potential return versus improving the way they capture and bill charges?
I probably couldn’t position it as one versus the other. I would say that, with regard to the charge capture work that we do — again, which interacts with the clinical domain but is not a direct part of it — there’s a much more clear and direct and immediate financial return, and it’s very significant. The clinical systems and Meaningful Use are trying to drive fundamental changes in clinical process. There are longer-term returns on those types of things. Also, there is a real return around the stimulus money.
Really, you have to be attacking both. It’s about timing and sequencing and integration.
When you look at the typical practice PM or EMR, what charge capture deficiencies does it have?
Depending upon what type of EMR system they have and how structured the documentation activity is in the creation of the initial charge, we make it very easy to do that to the extent that the system isn’t using it.
What’s more important are the things that go beyond that. We promote a lot more rules and flexibility and configurability to the physician. We do a lot to create the workflow between the physician and the administrators and the coders. We also do a lot of work that most EMRs don’t, around reconciliation and a lot of things that can be done to make sure that all the charges are captured independent of the tools around where the physician is entering their material.
That’s particularly true in an inpatient setting as well, where the EMRs and the operating systems that a physician may be working with don’t exist in the inpatient setting or they’re not there or not available.
We have a charge capture capability that cuts across those things and makes the job a lot more easy for them. We do things that are just out of scope, really, of a lot of their outpatient and office EMRs.
When you look at the big picture of the revenue cycle, what are the most important trends you’re seeing lately?
There’s a lot of consideration about reimbursement and reimbursement systems and how good the current system is and what we ought to be looking at in terms of bundling, whether it’s bundles of types of patients, or bundles of procedures and capabilities that go around an inpatient visit. I think that’s a very, very important issue and it’s going to change the way things happen.
ICD-10 is coming. Maybe it comes exactly when it’s projected now, or maybe it’s a little bit later, but that’s also a fairly significant item of operational impact.
Lastly, the fact that the EMR is going in place. That’s there, it’s going in, and the stimulus has helped with that. It’s had a big impact on our systems because we’re much more attuned to and aggressive about how our tools directly interact with and integrate and leverage that technology that’s being put in place than we might have been four or five years ago when those things were not moving as fast.
You mentioned ICD-10. How hard is it, overall, and how important is it to keep up with all the coding requirements that are constantly changing?
It’s tedious, it is hard, it’s extremely important, and it’s one of the values that a firm like ours provides because there’s leverage in doing that across multiple customers. It’s not impossible to do; it’s just a lot of work.
Something like ICD-10 is really more of a fundamental shift about the number of codes and some different approaches to the way the classification system is structured. That creates an additional challenge, but that’s what we do.
Isn’t it duplicitous for the government to talk about simplicity and transparency in healthcare, and yet it makes something as simple as getting paid so complex that companies like yours exist to support that?
One could only agree that the reimbursement system is not optimal and it ought to be streamlined. Frankly, we try to drive to do that. I think there’s plenty of room to streamline and improve and optimize processes and systems even with a lot of simplification.
What I would try to do is start the discussion around what are my objectives and what do I want to incent? Because that’s what the reimbursement system ought to be designed to do.
I do think that concepts of bundling are relevant in a number of these situations. I think concepts — to some level — of bundling around types of patients and things like that make sense. I think at various levels within the delivery system, counting what people do is an important part of reimbursement, but that may not be the case at the highest levels of reimbursement all the time.
I just think it’s going to be evolutionary. I would focus first on what objectives are you trying to get accomplished, and how to try to do that. Obviously, there’s a lot of discussion about does a reimbursement system incent more volume than one needs? I’d be looking at some of that if I were in a position of authority in looking at reimbursement systems.
What we’re trying to do is based on the rules that are put in place by the government and other payers. We’re trying to make sure that our customers accurately and efficiently bill properly against those rules. Our job is to understand what they are and get it right the first time. We streamline the process and make sure that the providers are getting it done accurately.
What percentage increase of charges that a practice is entitled to collect might a practice see with your product?
It’s a significant percentage. Five to 10% is not unusual. If they are in a paper process prior to us working with them, $20-30,000 a physician per year is a very routine kind of return that we get. This is because of things they may miss when they’re in an inpatient setting, defensive under-coding, and the inability to reconcile. We make sure they’ve captured all the business they’re charging. It’s a meaningful percentage.
How have the RAC audits changed your business?
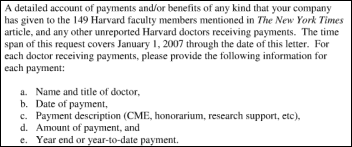
They’ve probably created a little bit more of an incentive to use a tool like this because we create an audit trail of the billing and coding activity. As we’ve evolved our tools over time, we’ve expanded our audit capabilities. In a number of settings, data has been extracted to support the compliance work that our customers are doing.
Looking at the big picture of revenue, what impact do you think healthcare reform is going to have?
One is the volume of care through the government and other insurance mechanisms is going to expand. The mix of how reimbursement, or the mix of payments, will increase through the structured insurance industry. That’s an expansion kind of activity for the providers.
I think on the flip side, it would only be prudent to expect that there will be more pressure on reimbursement and more economic pressure on providers. So, while there’s an expansion of volume that’s going to go on, I think there’s going to be an increased push — and one that’s going to be more intense than has been felt in the past — around being efficient and effective and high-quality and high-caliber, both clinically and administratively.
Many people think physician practice reimbursement is going to go down no matter what. How do you see practices reacting if that happens?
I hope they get more competitive. You know, improve their processes. I think that’s what they need to do. Now obviously, we have a wonderful system of clinical capabilities, but there are real opportunities to do things better.
Any kind of environment where you’ve got an opportunity to automate things that can be automated, you have an opportunity to reduce cycle times. You have an opportunity to reduce errors, whether it’s administrative errors or clinical errors. You have an opportunity to reduce frustration, at least within the walls of the provider institution, by improving processes.
All those things have to happen, and happen more effectively. I think that’s the only move that will be a successful one.
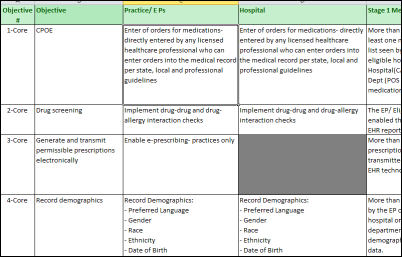
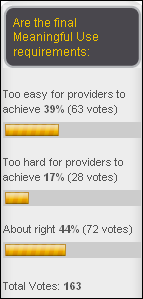
When you look at the Meaningful Use requirements, do you see that as doing enough to encourage the kind of behavior that will make practices more efficient?
I would say that it’s probably a start and directionally good, but my personal view — and this doesn’t have much impact on our business directly — is it has to go beyond those things. Whenever you have rules like that, I think sometimes they get at form over substance. I think more has to be done over time.
If you look five to ten years down the road, what are your plans for the company?
We’re a niche leader in what we do. We’ve had a very good run. Our track record is good. Our customer base is strong. We see this area of charge capture and linking the clinical and the administrative systems more effectively being a big growth area. All of our energy is on doing as good a job as we can do with that and expanding our capability.
We’ll probably be doing more in the future with regard to channel partnerships with HIS vendors. For example, we have a nice growing relationship with Allscripts today, so we’ll probably do a little bit more of that, but our focus is all on this particular area. Whatever happens with us down the road, we expect that this charge capture and charge management functionality to be at the core.
Final thoughts?
With our policy reform and a lot of what’s going on in the industry, this is such a real important time for the delivery system. The rules are changing. We think it’s a neat time to improve operationally, clinically, and organizationally. There’s probably no more important time to try to get more aggressive and innovate in ways that can pay off than now.
























































Thank you for your comments on Amazon. Agree 100%