John Glaser is CEO of the Health Services Business of Siemens Healthcare.

I’m not clear on your exact title and the scope of your job. Maybe you could explain that to me.
The exact title is CEO, Health Services Business of Siemens Healthcare. I’m responsible for, across the globe, the healthcare IT business. This is and Soarian, Invision, MedSeries4. Not only the products, but also the services that go with them … the hosting, managed services, implementation services. That is the pretty typical portfolio that I’m responsible for.
Almost never do provider CIOs become vendor CEOs. What motivated Siemens to pick you for the job and for you to take it?
Their motives were a couple. One is that having lived like I have for two decades on the customer side of it, I would bring an orientation to know what it’s like to go through CPOE implementations to what it’s like to sit in front of the board and request a capital budget. And that perspective would be helpful and useful in the course of the normal discussions one would have with a vendor.
I suspect that the other thing that was attractive to them was the demonstrated ability to lead and manage a complex organization, so there’s a high likelihood that I could actually get something done. Partners HealthCare isn’t the same as Siemens, but nonetheless, Partners HealthCare is a large, complex, highly matrixed organization.
I think the third is that I have a knowledge base of this industry, from CHIME circles or having spent time at ONC or to HIMSS or a variety of Institute of Medicine committees. There’s an understanding of the range of healthcare at the government level, but also because a number of these groups are part of our multi-stakeholders. How to plan things.
That’s probably a series of reasons – the customer orientation, the leadership ability, and the sheer knowledge that comes if you spend a lot of time in this industry.
The reason for me is that I spent 22 years at Partners, both 15 years at Partners itself and seven years at the Brigham and Women’s prior to that. I think we did some pretty good work and we have a lot to be proud of in that. But it can happen to anybody, if you get an itch, to try something different. That itch initially led me to spend some time with ONC and that itch continued.
When Siemens called and said, “Janet Dillione has moved on. Would you be interested in the CEO position?” I thought, well this would be … I’d learn a lot by sitting on this other side of the industry that I know and have been part of for quite some time.
It may sound corny in a way, but I believe deeply in the fact that the technology can improve care. I’m going to give every waking breath I have to that. I thought, I can have an impact – different, but a significant impact – by sitting on the vendor side of this. I have impacted Partners, but you can have a different impact. It was new, it was interesting, it had a wide streak of altruistic ability or potential there. That was the reason I decided to do that.
It’s a bold pick for them, not because you’re not qualified, but companies at that size that are conglomerates with international spans usually have someone they’ve groomed internally or they pick some interchangeable business leader that really doesn’t, in their minds, even need domain-specific knowledge. Is that an indication that Siemens is changing, or has it always been brave enough to say, “We don’t follow the mold and groom people by moving them from manufacturing nuclear weapons and sticking them in healthcare?”
I think it has learned, particularly under Peter Loscher, the new CEO – and I had an interview with him – that they believe you have to be careful in the idea of the interchangeable CEO. There really is deep domain knowledge that comes with it, and a series of relationships that can be very important. They are increasingly picking people that come from an industry who know that industry well and hence are likely to be much more effective at developing strategies and knowing what will work and what will not work.
Obviously you’re complemented by all kinds of people who know how do to the finance stuff that goes in the vendor community and the sales and marketing that goes with that. There’s a lot of corporate talent that can be applied. So I think they’re careful with the interchangeability idea. Sometimes that works, but sometimes it doesn’t.
I also think that they understood that here you’re putting someone who’s the CEO of a large business unit who you haven’t seen demonstrating their stuff for some period of time. They probably thought that on that, while I’m unproven in our situation or context, there is proof elsewhere. One of your earlier questions about having customer perspective and stuff like that, he brings that to the table.
I think it was a bold move on their part, a smart move on their part. It’s certainly not a typical move.
The most important question – is your office nicer than what you had at Partners?
[Laughs] It is truly bigger. I’d be comfortable living in a trailer for the rest of my life. You know, seriously, I don’t need that much. I’m a pretty simple guy in a lot of ways. It’s certainly bigger with a couch and whole bunch of tables and you could put a bowling alley in there if you wanted to. You have to plan on three minutes extra just to go from one end to the other. So it’s nice. It’s a nice place. That’s cool. That’s kind of neat. I don’t need all that space, but I’m certainly not going to start walling it off and living in something the size of a phone booth.
It seems like the hardest thing to get used to would be the incredible span of control that you now have. It was big at Partners, but it was somewhat localized and now it’s international. Has that been a struggle to understand, much less to change to how you want it run?
At Partners, I had 1,500 staff. At that point, you don’t know who most of the folks are. You don’t know all the things that are going on or that are being done. You can know that when your staff is 100, but you cannot know that when it’s 1,500.
One of the challenges of going from a staff of 100 to 1,500 is that your efficiency becomes more abstract and you’re more removed from the daily reality of stuff. So that I’ve gotten used to years ago and just realize that you’re very dependent on the folks who report to you and you trust them and they do good work and every now and then there’s an issue and you have to handle it.
When you come to Siemens, which has a staff of 4,800, it’s the same phenomenon. I don’t really know who all these people are or what they’re all doing or exactly what’s going on here or there. But you’ve got a team that is much closer to you to help you.
The thing that’s been a really steep learning curve is that this is a complex, large organization. It’s matrixed. I’ve been trying to figure out who does what. If you want to float an idea, how exactly does that work? Not only the formal way that it would work, but if you really want to vet an idea and build an alliance, who are you building an alliance with? That has been navigation in a complex organization both politically and formally how you get things done. It’s something you have to learn and I think it will take a while to learn.
Because it is global, you realize that the healthcare system in Japan is different and the healthcare system in Germany is different. These differences are real. It can be cultural differences in addition to the fact that Japan has 9,000 hospitals. Golly, that’s almost twice the number in the US. Average length of stay is almost three weeks. It’s just a different healthcare system, and hence you have to understand that and how systems work and that the role of the physician and the nurse can be different. In the US, things that the nurse does, in other countries, the doctor does that. Documentation is not the same as it is in the US. You have to understand that and appreciate all of those kinds of differences so that you can be effective.
The other is that there’s so much going on. There’s 1,000 customers and we’re in on the order of 20 different countries here. At any given moment, there’s some issue somewhere or something not working like you’d like it to work. You have to triage and knowing what to pay attention to and what not to. That takes a little bit of an experiential gain and refinement of antennae. The analogy that I use sometimes is that when you have your first kid and they cry, you’re all over it, but by the time you have your third, you can distinguish a cry that matters from one that doesn’t.
It’s been a steep learning curve in lots of different ways: complex organization, different countries, really learning about products and what they do and the services and where they’re strong and where they’re not so strong. I’ve been making a boatload of visits out to customer sites, who are they and what are they doing and what are the issues? It’s really neat if you want to be in a mode where you’re learning a lot all the time. Man, this is terrific.
It must be easier for you since you know a lot of the CIOs out there.
I think that’s true. When you’re sitting across from a CIO colleague, you know exactly what their life is like – the issues they face and the things that are hard for them. I get to meet with a lot of CEOs and a couple of times I met with board members. Shoot, I remember sitting across from the CEO of Partners and the CEO of the Brigham and Mass General and what they worry about and how they think.
Certainly a lot of the CIOs I know by name. You can be in these meetings and think, golly, I remember exactly what things were like. And it wasn’t that long ago that I had conversations about capital budgets and strategic direction and what should we do about Meaningful Use and personal health records, all that stuff. It is a very familiar territory.
When you entered discussions with Siemens about the job, was there an agenda on their part about wanting change, or was there an allowance that you’re going to want to make changes?
As you know, they went through some tough years when Soarian first came out. In the last couple of years, it’s been a nice recovery. I don’t think it’s complete, but a nice recovery. You see that KLAS score, you see that in sales, etc. It’s a nice recovery.
The basic directive is to continue the recovery. Let’s see what we can do here, let’s make it as good as it can possibly be.
Within that direction, I got a chance to look at the team, at the budget. Basically the FY11 budget was nailed down, but in a couple of areas we’ve got to add some investment if we really want to do this well. I was able to re-open the budget and insert some things along those lines.
The team had gone through a set of changes over the summer. Tom Miller, who was in the interim role, was orchestrating that. He and I talked all the time about who to put in what chair and what chairs to leave open for when I arrived. There was a real willingness to let me put an imprint on it, both people and roles, but also what is the agenda and what does the budget look like?
Soarian was a punchline for a number of years, but it’s suddenly the overnight success. With the recent KLAS recognition, it’s real. Obviously it was on that trajectory before you got there unless you’re a true miracle worker, but what’s changed and where does it go from here?
I’ve got to give Janet Dillione and Tom Miller a lot of credit for orchestrating that. To your point, coming in with a KLAS score of #3 overall – terrific, golly, that’s not where it was a couple of years ago. It was a lot of focus. There’s no substitute for saying, “We’ve got trouble with quality of software here. We’ve gotta focus.”
That’s not something you turn around in a week. That takes months and can take years. Plus you’ve got to put up with a customer base that’s saying, “Oh my God, I got trouble in River City here” and to help make sure that they don’t wind up in a bad place and stay the course, etc.
In the times I got into trouble with Partners, it was when systems were not behaving like they ought to. There is no substitute for just focusing and putting the best talent you’ve got on it. It’s like a form of guerilla warfare – day in and day out, week in and week out. You get enough small and medium-sized victories and you’ll get through it. In the meantime, you provide air cover for the team, trying to keep the distractions or whatever away. There was a lot of focus getting into that, focus on product, focus on service. It sounds simple, but man, that’s not an easy journey to go through.
So I think that’s a credit to the folks who were there and to Janet and Tom who preceded me. Where to from here? We’re entering a decade of healthcare which will be one of the most profound we’ve seen in 40 years. You’d probably have to go back to the Medicare and Medicaid act to see something as substantive as this. Healthcare is a payment system. When you change that, you change the industry in a very big way.
The Affordable Care Act and the financial changes and the private sector response moving to bundles and episodes and prove your quality and we’re going to pay you in a holistic sense, which is managing a diabetic over the course of a year or managing a total hip surgery through the rehab phase as a single payment, and by the way, prove quality to get your money.
That will be a big change. The level of financial risk will be a lot higher. There will be lots of experiments and Congress will futz with it, but hardly likely to materially change it in the near term. It was not lost on the Republicans that we’ve got a problem here in healthcare cost and quality. So that will be a hell of a time. It will be a hell of a time for providers – doctors, hospitals, health systems – but it will also be for those of us who serve them through products and services.
To be specific about it, if you look at the stuff we have, we’ve gotta have a stronger ambulatory-based story offering. We’ll continue to work with NextGen, but you’ve gotta have that integrated suite. I think Epic and Cerner have shown the value of that in the market.
We have to have much stronger analytics than we currently have, because you’re going to want to know if a diminished quality score’s going to cost you a lot of money or it’s not. We have to have better interoperability offerings that go with this. We’re going to grow the services base that we have because people put out a lot of money on this stuff and they go through this tough exercise of getting it in and now the stakes are higher and they want to make sure that they get yield. I think we’ve got some strong stuff.
I think the Soarian inpatient clinicals are strong, revenue cycle is strong, but you’ve got to round out ambulatory, round out analytics, round out the interoperability and the services base.
I can see partnering or acquiring on the analytics side, but there’s only so many ways to skin the ambulatory cat. What can you do there?
We’re looking at that now. We’ve got a couple of ideas on the table. Obviously we’ve got a relationship with NextGen, so we’re engaging them in the conversation about how they might help with that.
In a way, what an EHR does is pretty well understood. You have to write prescriptions and record a problem list and things like that. That doesn’t diminish the challenge, but in some ways there’s not a lot of mystery here. These things have been around for several decades.
I’m going to fast-forward five years from now, in which there’s a big shift in payment and you’re responsible for cohorts, for population management. You’re going to get paid by bundles and episodes. What exactly does that do to the ambulatory record? How different is it? That’s the analysis that’s underway – how different is that?
In a way, you can bring in consultants and smart people to help you take you through it, but if you look around the country, there are risk arrangements in place now. There are people doing population management now. You can learn a lot from them. So we’re plotting out the specifics of that. I think we need to get a little crisper, frankly, in our own assessment.
You mentioned Epic and Cerner. In all but the smallest hospitals, that’s where all the action is, with maybe Allscripts becoming a player, although two of those three weren’t very strong on the ambulatory side and had to become that. Can you gear up in time as people make their decisions now?
I think that’s fair. I think obviously the faster we get this done, the better, but we’re not going to have it done by the end of this calendar year, that’s for sure.
There’s a normal replacement pattern that goes on in this industry. At any given time, there’s enough people who have said, for whatever reason — my incumbent vendor, I’ve had it. There’s a normal churn you can arrive at. I don’t believe that you get to the year 2015 that nobody buys any more for a period of time. Even through the Meaningful Use ebb and flow, there’s a normal churn that goes on.
An unknown at this point is whether there is a second wave coming. There’s a first wave that was Meaningful Use induced. People scrambled to round out their portfolio to get their payment. There’s a second wave probable. The second wave has two things that will drive it. One is a whole bunch of people got to Meaningful Use by cobbling things together. By hook or by crook, they assembled this piece and that piece and they jury-rigged this and jury-rigged that and by golly, they’re going to get it done in 2011 and 2012 to get their payment. But they know that this is not a long-term answer. They’re here for the couple of years until they get to Meaningful Use payment, then you go into this couple of year window before the penalties start kicking in and they may say let’s do it for real at that point.
That will be one phenomenon, because not everybody did a wholesale replacement. I may not have the capital, I’ve got other commitments, so I’m just going to cross the finish line in whatever fashion, but not a long-term fashion by any stretch.
The second is the read, and it’s hard to know, whether the payment reform stuff will cause hospitals to say, hey listen, we made a commitment a couple of years ago, but boy, given what is coming down the pike here, this just isn’t keeping up with what we’ve gotta do. Is it an EHR or ambulatory? Sure, but it’s different enough that we need a different set of capabilities to complement the normal core set.
I think we’ll see both play on top of the normal churn that goes on. Obviously I’d rather have it sooner than later, but I don’t believe that if you’re not there at a particular point in time there won’t be a shot.
You mentioned Soarian, which is clearly the new star. What happens with Invision and MedSeries4? Will those customers be encouraged to move to Soarian, which doesn’t seem like a good fit?
We’ve got some work to do on Soarian before you could legitimately turn to an Invision or MS4 customer and say, listen, the things that you like about MS4 and Invision, not just the feature function, but the cost of it, that we can get you that in Soarian, too. So we have some work to do to fill out some Soarian gaps. There’s still development engine that has to go on for a couple of years.
We’re increasingly hosting it and using the cloud techniques of virtualization so you can drop the cost of hosting it down to what it would cost you to today to host MS4. In addition, there’s been some really nice progress on getting the time required to do an implementation down and the variability of implementation down such that the conversion process is relatively inexpensive and relatively quick. We still have some work to do there.
We won’t move anybody unless they want to until we’re in a good position to say, you’ll not only be equivalent, you’ll be better off, and they’ll have the same price points and the same brief, straightforward implementation that they’ve seen before. The timetable is slightly fuzzy around the edges, but some people are moving now. I think it will be a couple of years before we’re in a great position to really tell the rest of the base that it’s in your interest to move rather than stay where you are.
You’re making a lot of changes and you had to start there almost immediately by overseeing layoffs. How is employee morale?
I think it’s pretty good. Obviously as you know and you cover, we’re moving 475 jobs offshore. It seems high, but we’re adding about 600-700 positions in other areas. It’s a combination of working with the folks who are affected over a two-year period of time and saying, hey, we’ve got this role over here and happy to fit you in there and retrain you if you’d like to do that and make sure that we do all that we can so that you land well. The other part of it is making sure that we reduce as much as we possibly can the people who wind up out of a job.
We have to make sure people understand what’s going to happen in the provider community. The financial pressures will become significant. I mean scary significant. They will be turning to us and saying, “You’ve got to reduce your costs.” Then it won’t be the normal arm-wrestling with a vendor that goes on – that will be real. What we cannot do is be in a position where they cannot afford us. If that is the case, we will have failed them. And what we cannot do is fail those who, day in and day out, deliver care. That is just not why we’re here.
Whether it is hosting costs will be reduced or implementation costs being reduced or support costs being reduced, we have got to reduce the cost, because they are in a position where they will need that if we are to serve them and serve them well. I remind them, not that they need much reminding, that at the end of the day, there are real physicians and real nurses taking care of real people who are just like us and the people that we love and our job is to serve them. That’s fundamentally why we’re here and we’ll fail to serve them if we become increasingly out of cost reach.
That obviously, to your point, had a morale plunge. I think overall morale is pretty darned good, because what people see, as in earlier this week, Number 3, that’s pretty darned good given where we were. Man, we’re getting’ our mojo back. We have some work to do, but golly, all that hard work over the last couple of years, that’s starting to pay off. And then they hear from customers who are live with CPOE and are pleased with that.
I think the net of it is the feeling that after a struggle, they’re back and they’re where they want to be, mindful of all the work still to be done. By and large, it’s pretty high. The morale is pretty darned good, mindful of all the challenges we face and some of the tough choices we will continue to have to make.
If companies have a personality, and I tend to think they do based on their corporate culture, Siemens always to me seemed really rigid and conservative and quite cold. It just never seemed like it was a very fun, creative, and hip kind of company based on the Web site and the marketing materials. Do you think that’s accurate and do you think that needs to or will change?
I don’t know that it’s accurate. It’s an engineering company at its core. It’s a 76 billion euro company, 420,000 people and all the stuff they do. They do fast trains, they do windmills, they do water purification plants, they do MRIs. They’re an engineering company.
One of the things that comes with an engineering company is a drier appearance. They’re not inherently marketeers. They believe if you engineer a perfect product, people will realize the spec and they’ll buy it. Sometimes I think the coldness is really engineers. They’re not cold, they just don’t understand the need for sizzle and pizazz and that kind of activity.
There’s a need to change that. They understand that it’s not inherent in their DNA that they know how to be more flashy. I don’t know that it’s cold, it’s just engineering-like, for lack of a better word.
I think we have to, and part of the things I got more money for, be more effective and out there in marketing and methods and stuff like that. It matters. People won’t inherently buy from the spec sheet. They’ll need certain messages and understanding and a sense, particularly, of the human-ness that comes with healthcare, and that we’re part of that. That we’re trying to change. It won’t always be easy because at their core, they’re engineers.
Do they get your sense of humor?
[Laughs]. Frankly, the real reason for leaving Partners is that I’d used up all my jokes. I had to find a brand new audience. They were going, “Uh no, not again, not that one, I’ve heard that 26 times.” You can’t help be in certain meetings and not come out with this, that, or another, so I think they appreciate it. At times, I have to use my judgment about which ones to use internally versus which ones I can use in a public setting. So far, they’ve shown me they’ve got a sense of humor and they’re quality individuals.
Your stint with ONC probably changed your perspective. We’ve talked about this before. How do you feel about the time you spent there in advising the government and what’s your feeling about how it all turned out?
I thought that was one of the most extraordinary years that I’ve ever had. There you are, in the middle of them, where you’ve got legislative language that says, we need this definition of Meaningful Use and we need it fundamentally by Labor Day of last year, and you realize that Blumenthal didn’t show up until the last week of April. You’ve got three months to get this thing because then it’s got to go into the rule-making process and all that other stuff.
Listening to all these ideas, and they came from all over kingdom come, from small physician practices, public health people, patient advocates, Web 2.0. There were a lot of ideas, but we can’t crush the clinical community, either. We’ve got to narrow this thing down and that’s your job, to come up with a definition of Meaningful Use that’s a good balance that pushes the envelope, but that’s also in reach.
That’s just a really interesting, cool conversation to be in the middle of that and realize it’s not only complicated and hard to figure out, but whatever you do figure out has a phenomenal impact on the industry. You better be darned careful and thoughtful about it. It was just really neat to be in the middle of a very formative time, Meaningful Use and Regional Extension Center grants, all that kind of stuff.
As I mentioned in one of the things I sent you, I came out of there with an extraordinary respect for the government. Whether it’s Blumenthal or all the people who work at ONC, but also the folks that work for CMS and the Office of Management and Budget – they were smart people who worked their butts off and wanted to get this right and very receptive to feedback from people who were out in the community. This was a terrific set of characters and human beings and professionals.
I think what they did in an amazingly short period of time is extraordinary. There are clearly things you might have done a little bit differently, but jeez, when you look at how well the Meaningful Use definition was done and the various grants they had to get out the door and the standards they did … give a lot of credit to the Policy and Standards Committees and all the time spent there … that was just really remarkable. I think it was remarkable for me. It was an extraordinary piece of work done by all those folks in an amazingly short period of time.
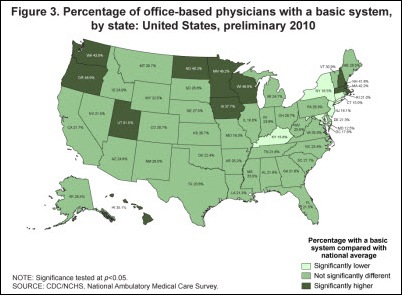
One of the things you come out of that with was an appreciation of the challenge of how diverse this country is. There were conversations about Meaningful Use where it was said that this has to work at Mass General, big old academic medical center, but also it also has to work at Seward Community Hospital in Alaska. Three beds, average occupancy 0.8. I though, 0.8? You’ve gotta be kidding me. If you were at Partners and said 0.8 occupancy, people would say you’re off by two orders of magnitude. But it has to work there to make all that happen.
I also have an appreciation for policy. What we did in these meetings at Siemens is think about how far down in bed size can you move. You say, if we did this, if we did that, we could get to 50. Actually, because of the way healthcare works in this country, you’ve gotta get even further south than that, because from a policy perspective, what you can’t do is strand the 20-bed community hospital. You can’t strand the solo practitioner, because that is so much of the care in this country. It’s interesting to me that the policy angle factors into business decisions because business decisions, if they are done well, also help support a broader national policy.
If we look back in two years and we’re doing your report card of how you’ve done at Siemens, how will we know you did a good job?
I’ve been asked a couple of times by people at Siemens the same question. I say, I’ll know we’ve done a good job if those who are our customers say to us, “Our care is better. It’s safer, higher quality, more efficient. We run a more effective operation and we do all the things we wanted to do as a provider and our strategy and our goals and our plan, because of the work we did with you, because of the products you have and the services.” If they say that, and uniformly or 90-odd percent, then we will have done well.
Obviously there’s numbers that you’ve gotta meet and this that and the other, and I’m not naïve about the need to do that, but that won’t be the success metric. Whether we’re 3, 2, or 1 on a KLAS score here, there, or in between – those would be great, but that will be the real – that you walk into one of these places and the CEO shakes your hand and says, “Working with you guys has been terrific, in fact it’s been essential for doing all the things we’ve done.” Then we’ll know that we’ve done a good job and I’ve done a good job and we can be pretty darned pleased with all the time, effort, money, and anxiety that we’ve put into this.
Any final thoughts?
You’ve got good questions, as you always do. I’m having a great time. I think we’ll do some good. I think we have done some good.
I came out of 22 years at Partners believing deeply in the mission of what they do. That is so part of my fiber that it’s kind of scary … sounds a little nauseating, frankly, at times, almost too much of a Boy Scout. But I believe it.
What I think we’re going to be able to do is we’re going to help those places do that. I honestly feel really good about that, that whenever I punch out of my time on this planet, if I can say that we helped a whole bunch of people do good things and care better … not a bad run. I’ll be OK with that.


























































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…