Jim Traficant is president of Harris Healthcare Solutions, the healthcare business of Harris Corporation of Falls Church, VA.

Give me a brief background about yourself and your new job. Congratulations, by the way, on being promoted to president.
Thanks. It’s a great privilege.
I’ve been at Harris now for 10 years. I worked at a small business prior to joining Harris, so I’ve experienced both large and small companies. I’ve worked in government and commercial business. I’ve got 25 years’ experience as a technologist and as a business executive, but my passion for transforming healthcare comes as a result of being a patient.
I’ve had two liver transplants. The first one, my neighbor saved my life. We were the fifth to have the surgery, the first that weren’t related. I have had two transplants in between an episode of sepsis.
In my experience traversing the healthcare market, I learned that people are passionate about their work in healthcare, obviously. They have lots of data, but what was missing was information.
After my second transplant, I sent a note to the Harris CEO asking to take the company into healthcare. Harris is a pretty large company. We move information with lives at stake in every market we serve, like defense and intelligence. We have two million passengers that ride on our Harris Network for the FAA. I knew if we could move information in healthcare like we did in those other markets that we could save lives, make a difference, and maybe even create a business.
Five years ago, I didn’t know if I would ever get to work again. To be honored by working at Harris and leading us in healthcare is a privilege I could not have imagined. It’s just terrific.
Harris has mostly been known, as you said, as a government contractor. It seems like that may not necessarily be the case going forward. Will the company go after the commercial healthcare markets?
The way I like to describe it is that Harris will have a significant role to play in helping to shape the future of healthcare, and healthcare is going to have a significant role in shaping the future of Harris. It’s a really good match.
Tell me about the strategy behind the Carefx acquisition.
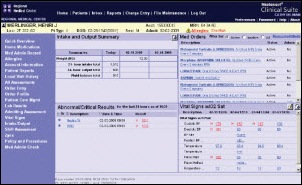
We were really fortunate. Early in our healthcare venture — we’d been at this for four years now — we were awarded the Nationwide Health Information Network Connect program. We were working on behalf of the Federal Health Architecture to integrate the largest creators of health information, like military health, the VA, and Indian Health Services, so they could share information securely with each other and then provide that information to the largest consumers of health information at the federal level, like National Cancer Institute, the CDC, Social Security — which spends, you know, a half billion dollars a year just trying to find health information so they can determine benefits.
We had a couple of breakthroughs in that process. One was that Social Security used to take on average 83 days to find health information to determine benefits for our citizens. When they went through the gateway that we created for the Federal Health Architecture, this program called Connect, they went from 83 days to 24 seconds getting that information. That’s the kind of transformation I think the nation’s looking for out of IT being applied in healthcare.
A second thing we learned was that over half of the care provided for our active duty and retired service members comes out of the private sector. If we were going to play a role in transforming healthcare, it wasn’t sufficient that we could just get the federal sector connected to try and create a tipping point in health information exchange. We had to connect it to the private sector.
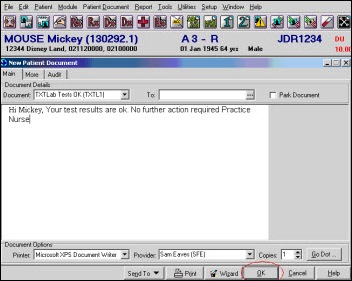
What Carefx brought to us was this real strength in the private sector. They were at over 800 hospitals globally, over 650 in the US. What we had done at the federal level to provide this integration and connectivity connecting the infrastructure, they did on the commercial, side but in a different context. They were able to take the information from where it was created and deliver it to the computer screen and organize it the way a clinician thinks and works according to their workflow — labs, images, med reconciliation.
It seemed like a perfect fit. Culturally, it was a perfect fit. They’re just great talent, great people, very deep in the healthcare domain, and really able to inform this rich technology base that Harris has as we move out and try to play a role in transforming healthcare.
That acquisition was a pretty strong signal of the interest of Harris to get into the commercial space. Do you see the potential for more acquisitions, or do you think Harris will be more of a builder than a buyer?
I would say this about Harris. It’s a great company. It has answered national priorities in almost every dimension over its hundred-plus year history. Healthcare is a national priority that’s going to require bold thinking and a strong presence and Harris is one of those companies. We’ll continue to grow organically, and I would expect over time that we’ll do more acquisitions. We’re committed to playing a key role in healthcare, so all of those options are going to be in play.
Healthcare divisions of big and broad conglomerates seem to lose some of their innovative capabilities. Do you see the Harris culture being different?
We have a very rich culture. In fact, it was one of the surprising things for me when I came out of a small business into this large, now six billion dollar company.
One of the things that many don’t know about Harris is that defense and intelligence invest very dramatically in Harris to take the state of the art in a number of technical disciplines and advance it or apply it in unique ways. In combination of significant investment plus what we contribute, we do about a billion dollars of research and development a year.
What we’ve seen is there are great parallels in healthcare to the challenges that have been faced in these other markets. I’ll just give you an example. What we saw post-9/11 in the intelligence community was we had all of the data. What was missing was a situational awareness at the national level that would be able to piece together all the information that was in these isolated pockets.
In healthcare, what we see is a very fragmented market. There’s lots of data, but it’s isolated with stovepipes. It needs to be connected. Then we need to make sense out of the information and create situational awareness for healthcare just like we do for intelligence.
The other corollary we see is when you think about what an intelligence analyst does, they sift through a variety of information sources and then apply judgment in a time-critical fashion with national security and lives at stake. We provide that information on a global scale and enable that capability. It’s exactly what physicians do. They have to piece together information on disparate sources and apply judgment in a time-critical fashion with lives at stake.
We see this transference of technology from our core markets into healthcare as a totally logical and compelling way for us to do this. All this innovation that exists really distinguishes us from a lot of the players in healthcare.
For example, from a security standpoint, we are very unique nationally for ability to secure information and move it anywhere in the world and any device authorized to see it. In healthcare, it’s not going to be, “Can we secure information in healthcare?” It’s going to be, “Can we translate our security in a way that can be meaningful in healthcare, that they can afford it, that it can be used in a very efficient way?”
The innovation exists in Harris. I would say these other companies have innovation as well, but the passion, the national mission, the sense of purpose applies directly. One of the ways I like to communicate healthcare inside Harris and also with our potential customers is that Harris is uniquely trusted at the intersection of life and data and every market that we serve.
It’s a very natural extension for us to move into healthcare. The response we’re getting in healthcare, I think, is evidence of the fact that we really have something to offer.
Harris is used to taking on projects with a large price tag and large scale. Who do you see as your customer in healthcare?
We started at the federal level because it was familiar. We knew how to compete. There are also some real strong forces at play when you look at military health. Harris being a defense contractor — that’s a logical place for us to participate.
The Department of Veterans Affairs — how do we take care of our servicemen and women who served us so well for so long? Those entities are not only providers of care, but they are payers. We knew there would be alignment and rewarding of enterprise solutions that would deliver efficiencies that would help us provide better care at a lower cost.
We began there and got traction almost immediately, moving our technologies from the intelligence community for imaging, for example. We created an architecture for military health. We acquired a company in the VA that allowed us to do imaging across the enterprise for the VA, and then connectivity between DoD and the VA, not only from the integration or interoperability standpoint, but also for images and photographs and scanned documents, all of those being shared and able to be associated with a health record.
We knew that to transform healthcare, we had to move into commercial sectors. We’re not looking at healthcare in the same way we would look in defense or intelligence. We recognize that the buying and the programs tend to be much smaller in size, but we believe and we’ve demonstrated we could move technologies and do it very efficiently and create compelling solutions that will be affordable and transformative in the healthcare context.
We’re very excited about what this market has to offer. Just from a business context, it’s hard to deny that it’s four times the size of the Defense Department. I think that’s why others are pursuing it. We’re looking at more as a chance of, if we can make a difference in healthcare, focus on the transformation, then the money will take care of itself. So far that’s been the way it’s played out.
You mentioned the VA and the DoD. I’m interested in the conversations being held about whether they should buy or build or how they can agree on a single system. You have a unusual perspective and viewpoint. What are your observations?
I think we have to be careful in one sense. I think there needs to be seamless system. It can’t be that the information struggles to come back from theatre to stateside and then into the VA. And then we have to think about the continuum. It doesn’t stop there. It has to be able to be connected to the private sector as well. That’s when ONC and some of these federal initiatives become really important as we set the foundation for how healthcare will happen in the US.
The military mission is different from the VA mission. I think we need to make sure that whatever we come up with, I’m not sure one size fits all. But we have to make sure that we can fit the military mission primarily for the military, and then make sure that what we’re providing for the VA is able to provide a continuity of care that bridges both the military as well as the private sector.
I don’t know if you can do that in one off-the-shelf system. You might be able to. I don’t think anybody knows, to be honest.
The other thing that the VA is challenged with, but I give them credit, is they get to work through these very hard solutions on a very large scale in a public way. Everybody’s watching every move they make, so if there’s any flaw, it gets exposed and printed. Most enterprises don’t have that type of scrutiny.
What the VA and the military have been able to do — quite extraordinarily when you look at enterprise healthcare in managing multi-millions of patients and doing it securely and on that scale — they really helped advance healthcare in the United States. I commend them for what they’re trying to do. I’m not sure what the solution needs to be, but they got the right minds looking at it and I’m confident they’ll come up with the right answer.
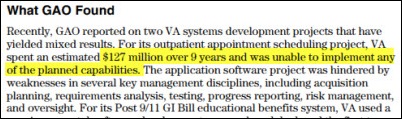
Have the taxpayers seen value from their projects?
I’d have to say yes. They have seen value. You have to remember that the VA has led in a lot of instances. Ninety percent of all doctors trained in the United States go through a VA facility in the course of their training, so there’s a benefit broadly to the US for what the VA has done that we can’t lose.
At the same time, there are new technologies and new systems that are coming into healthcare. I think the VA, very strategically, is looking, “Hey, we’ve been doing it our particular way, but that doesn’t mean it has to be the way we do it going forward.” So again, I give them credit that they’ve been self-reflective and wherever they can leverage commercial investment and solutions, I expect that they will do that more, not less, but time will tell.
Harris recently announced the joint venture with Johns Hopkins Medicine to do some work with medical imaging products. I’m curious what the scope of that project is.
Hopkins saved my life on more than one occasion. My first transplant was there. I had sepsis and they again saved my life a second time. I knew a lot of the physicians there.
I went back to them and after I was given the privilege of starting a healthcare business. I said, “Look, you saved my life, maybe even saved my career.” We started working together. What materialized is when they looked and saw the kinds of things we could do in imaging. I’ll just give you an example.
In the intelligence space, somebody at the edge of the network — one of our servicemen or women serving in harm’s way — makes a request of imagery of some type. We go through a discovery process and find what’s been requested and enhance it with additional information that would make it more germane to their circumstance. We deliver it anywhere in the world on any device authorized to see it in near real time. It is awesome. Harris is literally a national asset in the imaging context.
What we see is a very unique ability to translate some of those technologies to healthcare in an accelerated way and create solutions that didn’t exist previously. That’s the opportunity we see at Hopkins. They’re the most trusted name in healthcare. Harris, I’d like to argue, is the most trusted name in secure information management. When you put those two things together, it enables Hopkins to leverage the information sciences in very unique ways, in this case particularly imaging, and help fuel the transformation that the nation’s looking for. We’re very excited about what’s possible in that relationship.
When you look at what healthcare IT advances are out there or potentially coming, as a technologist and a taxpayer and a patient, what gets you excited?
A couple of things. I think that when we move from a disintegrated, fragmented, and we can argue primarily paper-based system — although there’s a lot going on to digitize it. But if we had a digital system versus a paper-based system, it would better than what we have, but a far cry from what we need.
What has to happen is it has to be a connected framework for healthcare — where instead of walking into a hospital with your life at stake and your information carried under your arm in a notebook with some CDs in your hands hoping somebody can make sense out of this and figure out how to save your life — that the information shows up when you do and it’s a complete picture of your health. And now we take the knowledge base of these tremendously skilled and dedicated clinicians and enable them to take more information and apply judgment against it in an accelerated way. We will totally transform healthcare.
If we get to a data-driven care delivery model, OMB has said we will take out one-third of the national spend. When you look at the impact nationally of healthcare, the cost of healthcare in the United States and what we get as a return that investment, we’re not getting nearly the return that we need.
The technology will not in itself transform healthcare, but it will enable that transformation. I consider it a privilege and my life’s calling to be part of that transformation, leveraging the rich technologies of Harris to make it happen.
Doctors don’t want to type into a computer all day and patients have no interest in entering their information into personal health records. Do you think there’s a challenge that we may either not have anybody willing to create data or that there won’t be enough people sitting on the back end to monitor and react to it?
I think we’re going to get better at this. We’re in the very early stages of a transformation and it’s a little bit awkward right now.
I came out of the aerospace world previously. We used to fly satellites, for example. Like in the Apollo 13 movie, they’re staring at streams of paper that are flowing and guys are sitting down and doing math equations trying to solve hard problems. Then we went to the computer, and all we did was emulate what we were doing on paper. We did it on the computer. We would look at strings of bits and bites and try to make sense out of it.
Eventually we advanced the interface so that we could run constellations of satellites with one or two operators. We did that because we were able to distill the information from bits and bites and go from data, to information, to knowledge.
That’s going to happen in healthcare. It won’t be that we’ll supplant the clinician or the judgment in healthcare, but we’re going to give them a stronger knowledge base from with to apply judgment and be able to deliver it in a simple, easy to assimilate way. It’ll just become part of the workflow.
I really think we’re just in an awkward phase of transition. This is going to get to a point where it will be second nature, just like it is for us on our smart phones and how we engage even socially using computer technology. It’s certainly going to transform healthcare.
What would you say are the most significant opportunities and threats to healthcare IT as an industry?
That we allow it to be digital and fragmented is the biggest threat.
Once we connect the framework for healthcare, there’s going to be innovation in healthcare in an accelerated, unprecedented way that healthcare has never experienced previously. There’s going to be an enablement of a system approach to healthcare that has never been possible previously. We’re going to see competitive models. We’re going to see efficiencies delivered.
We’re going to go through a transformation. I’m not sure how quickly it will happen. It might take us five years. I hope it happens in less than 10, but we’ll get to a place where the information flows in healthcare like it does in other industries.
The biggest risk is that we continue to behave as if digitizing is sufficient, we continue with proprietary technology, we continue in monolithic systems.
My confidence in healthcare is that it’s just part of the transition. It will be the first phase of the transition. It won’t be the endpoint. We will certainly get to a place where we’re operating in a system framework, information flowing securely and ubiquitously. It will patient-centric, data-centric — a whole network built around patients. I think that’s the biggest opportunity. It takes advantage of what America’s great at, and that’s innovation and technology.
I think we’re in a great spot to lead the world and help to transform this. I think it’s going to go from a terrific cost and drag on our national economy to fueling our national economy in ways that we have not imagined.
Do you have any concluding thoughts?
First, thank you for doing this interview. I really appreciate it.
I also would like to thank the caregivers in healthcare. They’re the unsung heroes. They’re the part of the healthcare system that’s yet to to be tapped. I think they know a lot about how we can improve it. I think this future state of technology is going to make it more efficient, better care, lower cost, and transform this economically in the United States.
The last thing I would say, and this is personal, is I’d like to thank the people that work with me at Harris Healthcare for their passion and dedication. I like to say the two best days in a person’s life are the day you’re born and the day you know why. We are fulfilling what for me is a dream. The people that are working with me are just the finest. That goes for the latest part of our family at Carefx — just great people, committed to making a difference. I’m just proud to be associated with them.
![]() From Baywatch: “Re: UCSF. The CIO is leaving involuntarily. Looks like the board finally figured out that the Centricity debacle was as much of a leadership problem as a software problem. The Epic project is floundering and bleeding money, with poor direction and an incompetent staff.” We asked a UCSF press contact, who replied: “Mark R. Laret, CEO of the UCSF Medical Center, today announced that ‘Last Friday, CIO Larry Lotenero notified me that he will retire at the end of June, completing 10 years of service to UCSF.’”
From Baywatch: “Re: UCSF. The CIO is leaving involuntarily. Looks like the board finally figured out that the Centricity debacle was as much of a leadership problem as a software problem. The Epic project is floundering and bleeding money, with poor direction and an incompetent staff.” We asked a UCSF press contact, who replied: “Mark R. Laret, CEO of the UCSF Medical Center, today announced that ‘Last Friday, CIO Larry Lotenero notified me that he will retire at the end of June, completing 10 years of service to UCSF.’”![]() From TopCrush: “Re: AAOE meeting. I’m at the American Association of Orthopaedic Executives in Orlando this week, along with a few hundred other folks and about sixty exhibitors. ACOs are definitely a concern for these guys. Orthopedic docs are scared of being left out and worried about the financial ramifications. Kind of funny but they have a VIP entrance for participants that have been coming for years or on a chapter board. AAOE set up a fun Sports Lounge in the middle of the show floor – shuffle board and fuse ball included.” Thanks for the update from the field. I wish I had a special door I could walk through every once in awhile, just to make me feel more important.
From TopCrush: “Re: AAOE meeting. I’m at the American Association of Orthopaedic Executives in Orlando this week, along with a few hundred other folks and about sixty exhibitors. ACOs are definitely a concern for these guys. Orthopedic docs are scared of being left out and worried about the financial ramifications. Kind of funny but they have a VIP entrance for participants that have been coming for years or on a chapter board. AAOE set up a fun Sports Lounge in the middle of the show floor – shuffle board and fuse ball included.” Thanks for the update from the field. I wish I had a special door I could walk through every once in awhile, just to make me feel more important. ![]() Mr. H semi-left me on my own tonight, just in case you were wondering why there are fewer smoking doctor images that usual. Mrs. H deserves a date night every once in awhile and I hope he is taking her somewhere special.
Mr. H semi-left me on my own tonight, just in case you were wondering why there are fewer smoking doctor images that usual. Mrs. H deserves a date night every once in awhile and I hope he is taking her somewhere special.







































































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…