Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…
News 8/21/09
Obama people bring healthcare PR show to Chicago bearing taxpayer gifts
Research article: eICUs may or may not work, but we didn’t really have time to check that out
Medsphere gets a sale
From I.T. Guy: “Re: Cape Cod Hospital. Apparently they made the decision to pull the plug on Meditech after a long relationship and install McKesson.” Unverified.
From Jules Verne: “Re: Check out these earnings.” Ancillary systems vendor Aspyra (warning: their site has loud and gratuitous Yanni-type music to accompany an otherwise stark site) files a horrendous 10-Q: a loss of $1.6 million on revenue of $2.1 million. The company says it will have losses and negative cash flows for the foreseeable future, meaning it needs financing or to sell shares (not likely: 12 million shares are already out and trading at 19 cents, 66% off the year-ago price, valuing the whole shebang at just over $2 million). I might have to ask our new financial expert Ben Rooks to lay out what options the company has (beyond the obvious – sending everyone home).
From Dr. T: “Re: hospital in Taiwan using the PBX-to-Skype gateway. I had been to this hospital and seen this working. It is very effective and the carts are battery operated with standing space for the nurse to actually ride it. The cart accommodates a fixed touch screen along with MAR drugs.” I’m getting a brainstorm … nurse golf carts with a built-in Pyxis machine, a Skype headset, and maybe a drink holder and MP3 player. They can be like those golf course ladies who sell snacks to the people pretending to exercise by riding around on carts of their own and swinging a club occasionally between beers. Patients pop their “give me drugs” bedside button, the nurse gets a Skype message, the eMAR pops open the onboard Pyxis and pops out the med, and the nurse careens off to dispatch it to the patient. Actually, the Taiwan hospital does have a pretty good idea, although Segways would be cooler.
From Sylvester Stallione: “Re: boards. Are you an advisor or board member of any companies that you haven’t disclosed? I don’t see it mentioned on your About page.” I’m not. Nobody really is interested in me as me, only as Mr. HIStalk, and that’s not happening. Sometimes companies ask for advice, but in the rare cases where I have the time and interest to do it, it’s free (and of corresponding value).
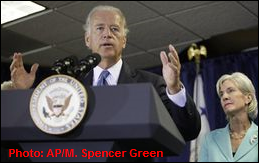
Vice President Joe Biden, HHS Secretary Kathleen Sebelius, and ONCHIT head David Blumenthal visit Mount Sinai Hospital in Chicago to talk up the administration’s healthcare reform programs and to announce $1.2 billion in ARRA grants for Health Information Technology Regional Extension Centers and state-level information sharing projects. The public wasn’t invited and the dignitaries wouldn’t take questions from reporters. Maybe I’m cynical (OK, I’m cynical for sure), but it mostly seemed like a PR visit to put some positive spin on the administration’s floundering healthcare reform program, sending the politicians with some Uncle Sam financial lollipops to hand out. The best quote came from an ED nurse at the financially dying hospital, which recently had less than two days’ cash in the bank: “We’re spit at. We’re swung at. We’re kicked. We have urinals thrown at us. We have bedpans thrown at us." That’s always the bad side of some of us paying for the care of others like we do for welfare and other entitlement programs: sometimes the recipients are nasty ingrates that make us wish we’d spent the money on someone who appreciates it.
Hospitals using electronic ICU systems like those sold by VISICU/Philips think they are improving safety and outcomes, but a 100-hospital study of those facilities shows no improvement, according to a Robert Wood Johnson Foundation study. But here’s the kicker: it appears that the methodology used was to just do a bunch of interviews about why hospitals bought the technology and ask their opinions about the benefits received. I didn’t see anything in the article suggesting that the authors actually looked at outcomes data of any sort. So, the conclusion isn not that eICUs don’t work, it’s that hospitals that use them think they do; therefore, they don’t see the need to do outcomes studies of their own (notice also that the article appears in Health Affairs, which is a health policy journal, not a clinical journal). Here are the takeaways: (a) nobody knows if widespread adoption of eICUs would save money, improve outcomes, or increase intensivist coverage (even after reading this article, which you might think would try to answer that question); (b) hospitals use eICUs to improve outcomes and utilization of specialists; (c) eICUs would work better if they were more interoperable with other clinical systems (gee, I wonder why clinical systems vendors aren’t more cooperative about interfacing to the product of a competitor like Philips?); (d) hospitals that don’t use them don’t believe they are worth the effort and cost (duh, and why even bother surveying those who don’t have them?); (e) here’s the money shot: “All ten respondents from eICU hospitals were enthusiastic about the technology’s impact on ICU performance, particularly on quality and safety. They all emphasized the benefits of redundant processes in the care of critically ill patients, whose clinical conditions can worsen rapidly.” So why in the world would the opinions of the non-adopters be relevant in any way? If you were considering buying a particular car, which would influence your decision: (a) asking 100 owners of that model if they like it and having every one of them say yes, or (b) asking 100 people who don’t even own a car at all why they haven’t bought one? The article doesn’t even answer the question that serves as its title: “Does telemonitoring of patients – the eICU – improve intensive care?” It seems like a pitch to have further eICU studies funded by government grants. The organizations with which the authors are affiliated get most of their income from grants. I suspect correlation, if not causality.
Informatics Corporation of America will add XML-based quality reporting capabilities from Mark Logic to its clinical portal.
NextGen gets several community health centers as new customers. ARRA will help a lot of them pay for new IT systems, so it’s a market that could be pretty hot.
HP, which bought EDS for almost $14 billion less than a year ago, is whacking the top-heavy salaries of the former EDS employees to be in line with what other HPers make, which is also a lot less since they cut salaries on the HP side in February. Some employees will take a hit of more than 30%.
Adena Health System (OH) extends its contract with MEDSEEK to automate physician referrals and to let patients view estimated out-of-pocket expenses before tests or procedures are performed.
The just-finished and sold out e-MDs user conference in Austin provided CME credits to physician attendees, which was apparently well received.
Scot Silverstein had a great idea to follow up on my “should I disclose vendor non-disclosure terms”. His thoughts: I shouldn’t have to do that because vendors should, as he says eloquently, “in an atmosphere of transparency and in deference to patients safety and to hospital governance, should gladly and transparently do so if such language exists in their contracts.” Great idea. OK, here’s what I know: Medsphere says it does not put nondisclosure language in its contracts. A reliable Meditech source says they don’t either. So here’s the challenge to Cerner, Epic, Eclipsys, McKesson, and other vendors of clinical systems: tell me that your standard contracts don’t prohibit customers from freely talking about software defects that could have patient safety implications and I’ll proudly announce that on your behalf right here. Or if your contracts do include such language, tell me why. I still feel creepy that when I worked for a vendor long ago, we were instructed to lie to customers who were anxiously reporting patient-endangering bugs, resulting in some wildly over-the-top telephone histrionics by thespianically challenged support reps. A typical overheard conversation: “Oh, you’re kidding – you don’t get a warning when entering that order?” (meanwhile, the rep is giving adjoining cube mates a laughing nod and making an overtly suggestive up-and-down fist movement that indicates a serious lack of concern that somebody’s loved one may be at risk because we as the scumbag vendor didn’t want to admit defects that would get us sued or replaced).
Medsphere gets a sale to 60-bed Beauregard Memorial Hospital (LA).
Weird News Andy found this article, which describes the previously illegal practice of hospitals paying doctors a cut of whatever cost savings their treatments generate. CMS is testing the practice in, as you might expect, graft and corruption rich New Jersey, where the concept of healthcare vig is well established in a less reputable way.
”Experts” in Australia say that too-rapid implementation of e-prescribing could compromise patient safety, citing a government study that found one hospital’s system doubled the rate of medication errors because it defaulted to the maximum dose and auto-refilled.
CMS is shopping for claims auto-denial software that will cut the $10 billion in improper payments it paid in 2007. These are the folks urging adoption of patient-critical computer systems, right?
OhioHealth goes live on a remotely hosted version of the EMPI of Initiate Systems, running on the interoperability platform of Accenx.
Garden City Hospital (MI) contracts with CareTech Solutions to support new AMICAS radiology workflow modules.
The backup generator fails at Fletcher Allen Health Care, taking its Epic system offline.
Capital Health CIO Gene Grochala is intereviewed about its implementation of Keane’s clinical system, which he called “a diamond in the rough … a sleeper” that the hospital’s clinicians scored 93 on a 100-point scale.
Cardinal Health’s Q4 numbers: revenue up 10%, EPS $0.86 vs. $0.96, but meeting expectations. The sexy part of its business will be spun off on August 31 as Carefusion, leaving Cardinal as basically a warehouse and truck delivery operation for drugs.
Sometimes I wonder if doctors pay attention to pre-med economics: this one is proud to do his own network wiring and PC maintenance, thus turning his own valuable time into that of a $30 an hour technician. You can’t accumulate wealth if your time is spent doing low-value chores like computer programming or screwing around with PCs, which is really more of an expensive hobby than a frugal handyman gesture when the only thing you have to sell is your time.
Odd lawsuit: a patient given what appears to be a single dose of the very common sedative Ambien during a hospital sleep study sues the hospital, claiming the drug blinded and paralyzed him. Ambien is not known to cause either problem.






Your note above about Cape Cod Hospital. Wrong…they’re going with Seimens, not McKesson. They’ve been named Vendor of Choice.
I thought I just read an article in the Feb. Healthcare Informatics talking about how Cape Cod had this long and wonderful relationship with Meditech and happy to still be using them.
Oops…I didn’t read the last line of that article…they we starting the replacement search. Sorry
I’ve actually seen more nasty ingrates with really good insurance than without. Nobody actually feels like they pay their own insurance anymore, and there’s nobody more entitled than somebody who has “really good insurance” when you tell them they can’t get an MRI for the back pain they got after shoveling snow for the first time in a year.
Does anyone have a list of clients Meditech has lost in the last 12-18 months?
“Sometimes I wonder if doctors pay attention to pre-med economics: this one is proud to do his own network wiring and PC maintenance, thus turning his own valuable time into that of a $30 an hour technician.”
Actually, I know 2 dentists and coupel of doctors that do the same thing and they do it because they really enjoy getting their hands dirty messing with wires, trying to figure out pcs, etc. Also for them is a stress reliever activity, and they brag to their friends about their pc skills. And when it gets too complicated, they do hire technicians to come out and check what the problem is.So I think they do know the economics, is just that they want to play around with computers.
Mr. HIStalk, looks like your cynicism is getting in the way of seeing some of the reality in the recent Biden, et. al. conference at Mt. Sinai. The real purpose, as you noted was to announce the $1.16B that will go out in 2010 in support of estab. some 70 extension centers and also help with the formation of State RHIOs, Now we both share some concerns as to whether or not this is a good investment, but the reality is that Congress has given HHS a piece of legislation in ARRA that must be spent and spent quickly for the “meaningful use of certified EHRs”. Now that we have some semblance of what meaningful use means, we now need to establish the infrastructure to support meaningful use (the RHIOs) and effectively select and deploy certified EHRs (extension centers).
For those wanting to know more about the two, did some digging and put up this post: http://chilmarkresearch.com/2009/08/21/spigots-are-opening-1-16b-for-hit-in-2010/
While the extension centers will share “best practices” (which have been written about for about the past five decades), will they also share knowledge of “worst practices?”
Implementing best practices and recognizing and eradicating worst practices (the “nasty stuff”) are two different beasts.
More succinctly, I would like to ask ONC how their strategic and tactical plans differ from the plans of the NPfIT that have led to its current state, which according to the House of Commons Public Accounts Audit Committee is not pretty (summary at http://www.publications.parliament.uk/pa/cm200809/cmselect/cmpubacc/153/15304.htm).
The Clinic’s emerging business segment is a fascinating one to watch. A few months ago the Clinic licensed a piece of internal technology and announced plans for a reference lab as well. As you say, a place to get more revenue. I do wonder, though, how many hospitals have developed innovations that have broader value (financially and otherwise), but those innovations never see the light of day because it’s not part of the “core mission.”