News 3/21/12
Top News

Misys, whose only remaining healthcare-related product that I recall is Misys Open Source Solutions, agrees to be acquired for $2 billion by Vista Equity Partners. Competing offers are possible despite a simultaneously announced Misys profit warning after Q3 revenue slid 12%. If the deal goes through, Misys will join a family of Vista-owned companies that includes Sunquest and Vitera.
Reader Comments

From HIMSS Benefactor: “Re: HIMSS13. Almost all the decent hotels are already booked. What happened? The W French Quarter has a few rooms left at $909 per night! Too much hassle … will have to skip this one.” I just checked the HIMSS online booking site and they’re showing 13 hotels available to attendees, starting at $155. The four-star Marriott on Canal Street is $230 per night and appears available, as is the close-by Courtyard at $180. I tried several of the travel sites to see if maybe HIMSS hadn’t locked down the whole block, but all showed no rooms available. Major concerns about infrastructure readiness abounded when HIMSS last went to New Orleans in 2007 and the experience was uneven in many hotels and restaurants. Having too few or too expensive hotels would give HIMSS a black eye it doesn’t need after massive attendance in Las Vegas. Let’s hope they just haven’t released all the rooms yet since we’re nearly a full year away. Otherwise, I’m going rent a house or two for the week, bring in sleeping bags, and run a HIMSS Hostel at exorbitant nightly rates. I don’t know where I stayed last time – I only remember that it was forgettable.
From The PACS Designer: “Re: SMArt. With the release of the iPad, TPD thought it would be the right time to mention The SMArt Platform created by the Children’s Hospital Boston and Harvard Medical School. Travis Good alerted us a year ago about it and mentioned that there is $5,000 prize challenge for the winning design. The SMArt platform is envisioned to be an app store for health, with applications geared towards both patients and providers.”
From Doreen: “Re: HIMSS. You should rent one of the tiny booths for around $5,000, use the fact that you have the greatest advertising strength on earth for healthcare IT to tell people you’ll be there, have guest booth hosts like Ed Marx and Dr. Gregg, and offer giveaways.” I had to embellish the idea, of course, by suggesting that (a) I set it up like a welcome center and offer information on HIStalk’s sponsors, or (b) I find some other company in tiny booth Siberia and tell them I’ll be their next-door neighbor and bring lots of traffic their way if they’ll pay for my space. Then I recruit volunteers to serve as my proxy to host the booth in rotation. I was excited about putting out kegs of beer until I Googled the price at the Morial Convention Center: $450 for crappy domestic brands.
HIStalk Announcements and Requests
Medicomp commemorates Inga’s participation in its Quipstar game on the HIMSS exhibit hall floor with a video. Note the Shoe Cam pictures, security entourage, the IngaTini in her hand, her green M&M snack, and the carefully placed reflector thingy that I bought her as part of her disguise. She was scared to death, but determined to earn Mobile Loaves & Fishes the $5,000 charitable donation offered by Medicomp in return for her involvement.
Welcome to new HIStalk Platinum Sponsor Jardogs. The Springfield, IL company connects patients, providers, and communities with its Jardogs FollowMyHealth Universal Health Record, an ONC-ATCB-certified cloud-based solution that aggregates information from disconnected organizations (it was recently selected by Iowa Health System, I recall). Patients become gatekeepers of their own information from anywhere in the world using a single comprehensive view instead of running around to a bunch of individual, proprietary patient portals. They can electronically complete physician-requested forms that are pre-populated with the practice’s EMR information, check in for appointments, and get real-time updates. Providers improve their patient relationships and address ARRA incentives for patient access (send reminders, provide electronic copies of results and med lists, share information per patient authorization, and connect to public health registries). The company also offers a patient kiosk that streamlines registration and data collection. Next up: home and wellness applications, such as for home physical therapy and potentially for home monitoring. Thanks to Jardogs for supporting HIStalk.
Acquisitions, Funding, Business, and Stock
RCM provider MD On-Line acquires MD Technologies, a provider of RCM products and the Medtopia Manager PM system.
Axial Exchange announces that its care transition solutions, Axial Provider and Axial Patient, are available for cloud deployment. The Raleigh, NC-based company offers care coordination and communications applications that connect first responders, hospitals, physicians, and health plans via a clinical dashboard.
In the UK, University of Lincoln and the local hospital trust develop a prototype of an orthopedic surgery training simulator that uses the Nintendo Wii to mimic the use of a surgical drill, allowing surgeons to improve their hand-eye coordination.
Sales
The non-profit United Health Organization (MI) will use video-to-handheld technology from JEMS Technology to connect patients requiring specialized medical attention with off-site physicians for consultation. Volunteer specialists who can’t leave their practices can visually examine the patient and provide treatment recommendations from their mobile devices.
DR Systems announces new contracts for its Unity CVIS with Twin Cities Community Hospital (CA), Good Shepherd Medical Center (TX), Healthcare Partners Medical Group (CA), and St. Luke’s Cornwall Hospital (NY).
The Maryland Department of Health and Mental Hygiene awards CSC a $297 million contract to replace the state’s Medicaid management information system and to provide fiscal agent services. The contract is for five years with three two-year options.
The Maricopa County (AZ) Board of Supervisors approves a $4.55 million contract to NaphCare for EMR licenses and installation services for its correctional healthcare system, which lost its accreditation in 2008 for issues that included poor recordkeeping.
People
Two weeks after agreeing to serve as CEO of Cal eConnect, Ted Kremer withdraws his acceptance and announces plans to stay on as executive director of the Rochester RHIO after learning that Cal eConnect’s funding is uncertain. Cal eConnect interim CEO Laura Landry will assume the CEO post.
Legacy Health System (OR) names John Kenagy PhD as interim SVP and CIO. He was previously with Providence Health & Services.
Healthcare analytics company Qforma appoints Valerio Aimale MD as chief of advanced products, William Howard PhD as SVP of new product development, and Delphina Perkins as director of client services.
Authentidate Holding Corp. names former Viterion Telehealthcare CEO Sunil Hazaray its chief commercial officer.
Announcements and Implementations
Cookeville Regional Medical Center (TN) implements MEDHOST’s EDIS.
Susquehanna Health Partners (PA) adopts Summit Healthcare’s Downtime Reporting System to address its business continuity and data protection needs.
Practice Fusion launches its research website to help public health agencies and physicians predict and manage outbreaks.
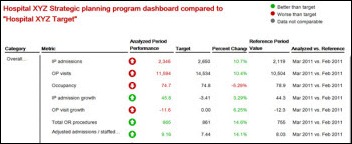
Objective Health, part of McKinsey & Company, announces the release of its Objective Scorecard performance dashboard and analytics solution for hospital executives.
UPenn Health System goes live on Brainware and Ascend solutions for accounts payable automation, helping it manage paper invoices and integrating with its Lawson ERP system.
The EZ DERM iPad EHR adds speech recognition using Nuance’s cloud-based technology. I accidentally strayed onto the cool new EZ DERM video above on YouTube. The company modestly calls its product “The Best EHR in the World.” I can’t vouch for that, but it might well make the best EHR videos in the world.
SAIC’s COO talks up the company’s Vitalize Consulting Solutions acquisition in Tuesday’s earnings call: “SAIC’s acquisition of Vitalize Consulting Solutions continues to support strong, double-digit growth in the commercial health IT arena.” In not-so-positive news, SAIC racked up a $161 million Q4 loss after setting aside $500 million to settle a criminal investigation involving cost overruns on a payroll system it developed for New York City.
Government and Politics
ONC releases a new version of its Connect software that incorporates updated technical standards and descriptions for the NwHIN Exchange. Connect version 3.3 supports such functions as patient discovery, document queries, and information retrieval.
Louisiana behavioral providers say that the state’s new Medicaid reimbursement software, which was supposed to make their claims submission easier, isn’t working. Providers say they can’t always enter new client information and some of what they’ve entered was lost, the progress notes function isn’t working, and nobody’s been able to bill for their services.
Other
TeleTracking posts a fun video of The Capacity Blues, a Cajun-flavored piano tune written and performed by one of its employees in honor of its upcoming New Orleans patient flow symposium.
Divya Shroff MD, HCA’s chief clinical transformation officer, writes a company blog post called Can Access to an EKG on your Phone Save a Life? in discussing the company’s collaboration with and investment in AirStrip Technologies. Her example involves door-to-balloon time for cath patients, with the potential to send EKGs directly from the ambulance to the cardiologist as both are in transit to the hospital.
I’m watching interviews filmed at HIMSS in Las Vegas by EHRtv that our pal Eric Fishman MD has been posting. Here’s one with Matthew Hawkins, CEO of Vitera, and here’s another with Shareable Ink’s Stephen Hau.
In England, hospital officials admit that they ordered the IT department to clone and snoop around the computer hard drive of a whistleblowing doctor who complained about unqualified staff and and was later fired. His boss justified the action, saying she had heard from employees that he was on the Internet a lot and wasn’t seeing enough patients.
The local newspaper interviews eClinicalWorks CEO Girish Kumar Navani.
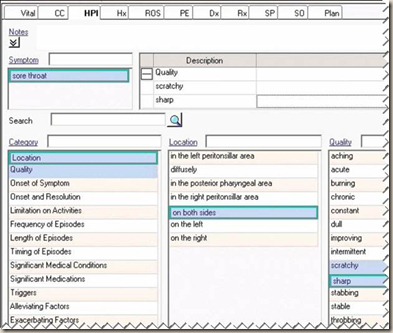
Dr. Wes says EMRs bury doctors in data without giving them useful information:
There’s so much data that we risk doctors becoming lost in it. It is entirely possible that we are in danger of not being able to find our most important clinical signals amongst the noise and clutter of all the data. Worse: time with patients is disappearing. Our health care information gold rush has acquired teams of programmers to feverishly implement a myriad of bureaucratic information system requirements in just a few short years. To this end, these programmers have been extremely effective. But almost as incredibly, these same programmers have little perspective of what physicians do or how we interact with patients and THEIR data. As a result, doctors are not only confronted by all of this this information placed before them, but waste precious time sifting amongst the data and continue to be the fall-guy for data entry. Codes, quality measures, documentation requirements and, oh, yeah, the progress and operative notes, are all being entered by doctors. In return, our screens have become crowded intersections of buttons, flags, options, icons, colors, warning alerts and (if we’re lucky) text. Oh yeah, and a new “upgrade’s” coming next week.
Note to companies: just in case you can’t spell HIPAA correctly, at least leave it out of the press release’s big-font headline.
University of Louisiana at Lafayette is looking for healthcare geeks to participate in its free Cajun Code Fest on April 27-28. Speakers include US CTO Todd Park, Intel’s Eric Dishman, and the guy who founded Priceline.com.
A Crain’s New York study finds that the 25 highest-paid New York City hospital executives earned a combined $60 million in 2010, with New York-Presbyterian’s Herbert Pardes topping them all again at $4.3 million.
Sponsor Updates
- CapSite GM/SVP Gino Johnson will provide an overview of the HIE market at next week’s 4th Annual Health IT Insight Summit in Boston.
- Liaison Technologies will offer Preventice’s wireless monitoring technology to collect and transmit patient data via its cloud services.
- Bloomberg Businessweek profiles Digital Prospectors Corp.
- CTG Health Solutions will participate in the Allscripts Central Region Users Group meeting in Des Moines, IA on April 19.
- Trustwave completes its acquisition of M86 Security.
- Health Care DataWorks selects Health Language’s Language Engine to map disparate data into its data warehouse.
- BESLER Consulting will use the Inventu Flynet Viewer to give its hospital customers access to the Medicare Common Working File stored on 14 CMS mainframes, allowing faster and more efficient claims review.
- DIVURGENT’s David Shiple discusses the proposed MU Stage 2 emphasis on personal health records vs. low consumer interest in using them in a blog posting.
- The local paper discusses Premier Health Partners’ use of MEDSEEK’s predictive analytic tools for targeted consumer mailings.
- Merge Healthcare and AG Mednet partner to integrate AG Mednet’s image collection platform with Merge’s Clinical Imaging Management System (CIMS) to enable higher quality images and data flow directly into Merge’s CIMS and EDC solutions.
- Capsule announces that it has surpassed the 1,000 mark for healthcare organizations using its medical device integration solution, including 200 new customers added in the last four months.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.













































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…