Pam Pure is CEO of HealthMEDX of Ozark, MO.
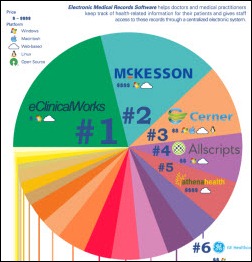
Let’s get the obligatory McKesson questions out of the way. What are you proudest of from the time you spent there and what regrets do you have?
I look back at McKesson with great memories. I’m very proud of our team and I’m very proud of what we accomplished.
We took a business that was basically going nowhere in the ‘98-‘99 time frame. We built a strategic plan and brought together a series of products — clinical products, imaging products — that we could deliver as a really robust solution to our customers. Over the eight years that I was there, we built great customer relationships, built a great working organization, and put some customers on the road to full clinical implementation and physician connectivity. It was a great time, a great experience, and I look back on it with a lot of pride.
In terms of regrets, I don’t really have any. I look at that as a great chapter in my career, a chapter that I’m very proud of. I learned a lot and it was a great launching point to this next chapter, which I recently started and I’m really excited about.
What led you to leave McKesson?
It was the right time, time for a new chapter. I left the organization and began thinking I was going to take a year off and just spend some time with my family. Things went on a whirlwind from there until I ended up HealthMEDX.
As you’re watching now from the sidelines, were you surprised by the announcement about Horizon Clinicals and Horizon Enterprise Revenue Management being de-emphasized in favor of Paragon?
I know this is going to be hard for a lot of people to believe, but I really don’t spend a lot of time watching McKesson. I’ve made a conscious decision, like when you send your kids off to school. You have to let them go. A really important transition point for me was letting McKesson go.
There’s a lot of great people there, a lot of smart people there. I rely on them to make the best decisions for the company and for the customers. I hope they will continue to do that because I think we set a precedent of putting our customers and employees first.
But you know what? I really don’t follow it. I’ve tried very hard not to have an opinion on McKesson, but just to support their continued success.
What is it about HealthMEDX and the post-acute care market in general that simultaneously got you to come there and for investors to acquire the company?
I left McKesson and I had this grand plan that I was going to take off a year and travel with my kids and do things like exercise and get fit. Shortly after I left McKesson, my mom was diagnosed with a really serious Stage 4 cancer. She had a lot of surgery and a very long rehab, which she experienced in my home.
And you know, here I am — I think I’m like Miss Healthcare, because I think I’ve been involved in healthcare for 27 years, so I must understand it — but here I was in the middle of helping someone I love recover from something very serious. It was the most challenging thing I’ve ever done, because it was very, very difficult to figure out how to manage her care.
My mom got back to the point where she could live at home with my dad. We went on a two-week vacation, came back, and my father had a heart attack in our driveway. He had quadruple bypass surgery and then he moved into the Pure Rehab Center, at which point over the door came up Pure Rehab Center the sign. We shipped him home about eight weeks later.
Three months later, my mother-in-law had a stroke. In this very compressed eight-month period of time, I had three people — who are very independent, very successful in their own lives, very healthy — all go through these major post-acute events at three fabulous health systems. In every case, I was so disappointed and so stunned by the lack of follow-up support.
While I was at home dealing with the emotions of taking care of parents and in-laws, I had a very introspective time. I said, what am I going to do next? I don’t want to go back and do another very large company. I would really like to help figure out how to solve this problem in the post-acute space.
I started spending time with my parents’ friends, my in-laws’ friends in trying to understand how they were dealing with managing their home care, moving to retirement communities, moving to assistant living organizations. As I started digging into this, I found that these organizations were very disconnected. It was confusing for my parents and their friends to deal with healthcare and follow-up. There are many people involved doing the same things, many different locations, and it was totally a paper system.
I approached the private equity firm and said, “I would really like to do something in the post-acute space to figure out how we can build a technology-enabled system that could be connected back to the health system. Post-acute care is going to be very strategic moving forward, and it’s got to be more connected and it’s got to be more automated.” That’s what began my journey at looking at companies in this space.
The question I should have asked you earlier but I was hung up on the McKesson questions is to describe what HealthMEDX does.
HealthMEDX provides an integrated technology platform that manages a patient in a post-acute environment. If they’re not in the hospital and they’re not in front of a physician, we automate it – home care, hospice, skilled nursing, assisted living, rehab, retirement communities, transitional care organizations moving from the hospital back out to the home. Anything that doesn’t occur in the hospital or doesn’t occur in the physician office — we can manage the patient through that experience.
What is most different about that client base compared to physician practices and hospitals?
For the most part, post-acute providers have more long-term patient care responsibility. I visit some of our customers that are skilled nursing homes. The patient might be there for 12 years. These post-acute providers or even a rehab center – these providers are kind of like the last check to make sure the patients gets as healthy as they can be. They finish the care.
In the hospital or in the physician office, treatment tends to be very episodic — finish off and go. In the post-acute center, it’s more focused on how do we get the patient back, how do we get this person back as good as they can be, and where is the right end place? I think there is more focus on managing the patient back as opposed to managing an episode.
That’s changing in health systems, and obviously with risk-shifting and ACOs, there is a great focus on the patient. That’s why I think these post-acute organizations are going to become more strategically important.
That market wasn’t really considered all that sexy by most people, where institutions were perceived to have both financial challenges and technology challenges. How did HealthMEDX turned out to be the biggest vendor in it?
The uniqueness of HealthMEDX comes in two areas. Most technology players in the post-acute space focus on one segment. You’ll see a lot of home care companies, you’ll see a lot of rehab companies, you’ll see a lot of skilled nursing companies. Most of those companies do one thing.
I think the difference and the magic of HealthMEDX is it’s a patient-centered system that knows it has to manage the patients. Where they are doesn’t matter in terms of how the care is automated and delivered.
If you look at our customer base, it’s very diverse. We do these large, national, senior living retirement communities. We automate the whole community. We do post-acute transition programs, where it’s a program for 14 days to get the patients from the hospital to home. We do home care, we do hospice, we do rehab. We have a large presence in all of the different segments of the post-acute market.
A big part of our strategic thesis was that post-acute care providers are going to diversify and consolidate. Nobody just wants to be a skilled nursing home or just an assisted living these days. They want to provide rehab services or home care services. The technology needs and the requirements of these organizations are changing.
Do you think federal reimbursement changes will encourage growth or consolidation, changing the way these organizations compete with each other as well as competing with hospitals?
We’re going to see a lot more networking between post-acute providers and hospitals. More sharing of the risk. When you look at readmissions and the health system focus on reducing readmissions, there are a lot of post-acute providers that can help them get there, in terms of managing the patient once they leave and trying to keep the patient form coming back.
A lot of the changes in the regulatory environment and in the risk-shifting environment will cause the post-acute providers and the health systems to become more tightly integrated. Some health systems will acquire more post-acute providers. I see some purchasing nursing homes, assisted living, some building retirement communities where they’ll have full management of the patient. Then I see a number that are building very progressive networks with regional post-acute providers to manage their patients once they go home.
There was a time when hospital CIOs really knew next to nothing about physician practice systems because they weren’t relevant to their organizations. Do you think that they’re going to be pushed into gaining the same expertise in long-term and home care systems?
I absolutely do. It’s very interesting to watch, because we all watched in the ‘80s and the first half of the ‘90s as the hospital markets started to automate it. It started with financial automation, then clinical automation, and then connectivity. We watched the physicians go through the exact same evolution – financials, then EMR, and then a huge focus on connectivity. That became the continuum of care.
I think we’ll see an extension in the continuum of care. I think that extension will include the people who are responsible for the care of the patient after they leave the hospital and after they leave the physician office. I think we’re going to see the exact same thing. Those post-acute care organizations have billing today. They’re now beginning the journey for an electronic clinical record. I think the journey for that electronic clinical record and health system connectivity will almost occur concurrently because of their importance in an ACO environment.
Those of us on the hospital side might assume that we’re doing cool stuff that should find its way into nursing homes and home care. Are those organizations things that hospital people could learn from?
There will be a great deal of information shared and a great deal of learning on the health system in the post-acute side as we build this collaboration and extend the continuum.
The hospital market today is much more experienced with implementing advanced clinical systems. The lessons learned in terms of process flow and workflow automation will be essential to the success of some of these post-acute care providers and will help us figure out the right way to make handoffs … what happens when a patient is discharged, what happens when a patient shows up in the emergency room. The health system and hospital clinicians are more system savvy and can help direct those handoffs, which I think will be great.
On the post-acute side, what’s very interesting to me is that the location of the patient is really insignificant in the care of the patient. For the most part, hospital systems and physician systems have been very visit specific and episodic in the way that the data is managed. Especially with HealthMEDX, the post-acute view is much more patient centered, just naturally patient centered in the way the product was built, with the assumption that the system has to follow the patient — the patient doesn’t follow the system. Just a lot more flexibility in how the technology can be deployed and the intelligence of the product to know the right way to bill.
Some of the biggest changes in healthcare IT have been driven by government changes, like reimbursement or Meaningful Use. Do you see that happening in the market that you’re in? Will hospital software companies need to build or to buy to get into that market or be left behind?
The post-acute market has similar regulatory requirements that are getting more complicated and more intense and I believe are driving the automation of the EMR in the post-acute market, very similar to what happened in the hospital and the physician market. Subtle incentives to automate, so you can electronically transmit clinical data and electronically transmit some more complex financial information. The regulatory push is definitely there.
Many of these post-acute organizations are selling “directly to patients,” quote-unquote, in terms of the value they can provide and the quality of care. In many cases, patients are making a very definite choice of where to receive their care and the technology infrastructure is becoming more important. Patients want families, want their parents in organizations that they feel are safe, with quality systems and services. Technology is becoming part of that decision process and the shifting reimbursement and relationships with hospitals.
We’re going to look back and see the next three years as a critical time in terms of hospitals and physicians being able to follow their patients home. To do that, the post-acute technology and post-acute connectivity is going to become essential. I think the progressive post-acute organizations realize that and are moving more rapidly than we expected.
How is selling and supporting customers in your market different than it was for hospitals and physician practices?
From a selling perspective, customers are very focused on three or four things that are very important to them. There is more clarity of what they are looking for. When you look at a hospital or health system, it is a very complex sales cycle with a lot of decision makers and a lot of stakeholders at the table. The post-acute environment tends to be more focused on exactly what’s required and is not as large and long.
When you look at the company over the next five years, what are your priorities?
It’s a great question, because I just really am excited about the potential to help build the technology-enabled post-acute world.
When I look at the next three to five years, the first thing that we can do is help these post-acute care providers build an electronic medical record that includes all of the information for the patient, whether they’re receiving home care, whether they’re receiving rehab, or whether they’ve had to move to assisted living. We can build one integrated record to manage that patient. I think Job #1 is supporting the consolidation and the diversification that’s happening in the post-acute market with an electronic clinical record. It’s really essential.
The second thing that is going to happen — and it’s going to happen quickly — is helping health systems connect and build relationships with these post-acute organizations so they have the capability to follow patients home. That will require a lot of work with health systems in terms of setting up the infrastructure and the process flow of moving a patient home or moving a patient to an assisted living or a rehab organization. Also being prepared to take the patient back when they show up in the emergency room or have to come back for services. Health system connectivity supported by industry standards — I think that’s Job #2.
Job #3, once we get that going and these post-acute providers are automated and they’re connected, there will be great learnings in terms of analytics. Where’s the most cost-effective place to send a patient? How quickly do you discharge them into transitional care? How long should transitional care last?
I’ll tell you this great story. A post-acute customer who’s trying to develop a specialty in transitional care said, you know, if a patient comes in for hip surgery and it’s scheduled, and you look at that same patient is not scheduled — they fall down and they break their hip. The patient who falls down and is unscheduled spends 10 days longer in transition care. And you know what we figured out? They need mental health services, they need emotional support. The fastest way to cut those 10 days is support for dealing with the stress of the trauma and the unplanned medical experience.
I really believe, and what I’m most excited about, is once we are able to automate the post-acute space and connect it, we’ll be able to figure out questions like, where is the most cost-effective treatment location? How do you move patients through the continuum of care in a quality, cost-effective manner? Because now you really have the continuum.
Any concluding thoughts?
I’m very excited about the business. We’re about to open an office just outside of Boulder, Colorado, so we’ll be expanding to two offices. We’re growing quickly.
For me personally, I’m just thrilled to have the opportunity to focus on a segment of healthcare that I’m extremely passionate about after dealing with some very traumatic personal experiences. I wake up in the morning believing that a company like ours can impact the way that care is delivered in the post-acute environment.
I would also say that I’m equally focused on building a company culture where people come to work and feel as excited and passionate about what they’re doing as I do. I’m really looking forward to that.















































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…