News 5/2/12
Top News
Castlight Health raises $100 million in Series D funding, raising its total to $181 million. The San Francisco company offers online tools to help consumers choose providers, evaluate cost and quality, and understand their healthcare benefits. Above is a TV news report about the company.
From Reckless Speculator CIO: “Re: Allscripts. Glen will appoint someone from HealthCor to the board to placate them and save his Teflon self. I think he said after the Misys merger, ‘Given the choice to control the boardroom or executive suite, always choose the executive suite.’” I tweeted Monday that big Allscripts shareholder HealthCor Management is urging the company’s board to replace Glen Tullman as CEO or put the company up for sale, saying his 13-year record of underperformance is not acceptable, particularly with the HITECH tailwind and high returns to shareholders of the company’s competitors (Cerner and athenahealth were named). They point out the company’s strengths, such as Sunrise and EPSi.
From Customer CIO: “Re: Allscripts. Stock prices don’t mean much to us as a customer, but I would like to know what the company disagreement was about. Perhaps over resources for its clinical products vs. a new inpatient revenue cycle product.”
From EMRwatcher: “Re: Allscripts. Glen wants to engineer a buyout of the company. He’ll probably get fired first, but that will make it easier for him to spend time getting the cash together.”
From MDRX Files: “Re: Allscripts. They should be well positioned for the shift of focus to the ambulatory world with clinical integration and accountable care. Epic is benefitting from their solid vision and impeccable execution, but the door is open for Allscripts to raise the bar as the only company designed to deliver on the future. Everybody else has inpatient baggage that will slow them down. I hope Allscripts takes advantage of the stock plunge to go for it. The software side of the industry needs fresh thinking. Some companies will become commoditized as data an information prevail as strategic and they’re so entrenched in their transaction processing history that they can’t fathom any other world. Epic has the advantage of not being publicly traded and not required to deliver quarterly numbers, but maybe an Allscripts shakeup was what was needed to invigorate them to take a bolder view of the future.”
From Global Travelin Babe: “Re: Allscripts CEO debacle. I have no idea if it has any merit, but I heard they’re going after a few brand name, reputable CEOs to get their mojo back. Two names mentioned were Ivo Nelson from Healthlink and John Glaser of Siemens.” That sounded pretty off the wall, but I asked both Ivo and John since I like to get answers when I can. They say, not surprisingly, that they have not been approached and wouldn’t be interested.
From Kermit: “Re: healthcare IT from a doctor’s point of view. This is a monthly show for the Mass Medical Society, produced at a local cable access station where I volunteer. Given my links to health IT, I suggested this topic.”
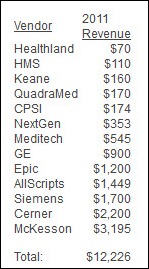
From Vince Ciotti: “Re: Susan’s inquiry about the size of the healthcare IT market. The top 13 vendors had $12 billion in revenue in 2011, so I’d guess the total market is at least twice that with all the niche players and consulting firms.” Above are Vince’s numbers.
From Dragon Man: “Re: Mike Mardini. The founder and CEO of Commissure, the radiology speech recognition company acquired by Nuance in 2007, is leaving. He was also the founder and CEO of Talk Technology, acquired by Agfa in 2001.” Unverified. No change in his LinkedIn profile so far.
From HIPPA Hound: “Re: Raleigh newspaper’s series on hospital profits and low levels of charity care. Not new since it was reported last week, but it has struck a few nerves.” Politicians (including the ever-present Sen. Chuck Grassley, who will no doubt write a scathing letter of inquiry that yields nothing) get worked up about about the ongoing series, which I’m sure is exactly what the newspaper planned. Every newspaper follows the same formula when trying to goose dying circulation: (a) write a huge and endlessly publicized series on some hot button topic, with or without solid facts and objectivity; (b) refer to their own series in some high-and-mighty editorials; (c) prod everyday people enough times about the topic du jour until they get enough outraged quotes to yield let another article; and (d) pester people in power about their articles until somebody finally at least pretends to share their outrage and makes vague promises about coming down hard on the villains. That’s about as good as it’s going to get from the dead tree folks whose readers avoid making eye contact with the politics and world news sections as they make a beeline for the sports page and comics.
From Kaiser Roll: “Re: Kaiser Permanente’s innovation award winners. Here’s the list.” Some of the technology winners:
- Knowledge Builder, which provides a way to import clinical algorithms into a rules engine to identify appropriate treatment conditions that are likely to occur, such as kidney stones
- OpQ, an operational dashboard that extracts information from the data warehouse and Epic Chronicles database every 10 minutes to allow outpatient managers to oversee staff assignments and patient flow.
- Specimen Transfer and Tracking (STAT), a chain of custody tracking system for specimens that would replace paper logs.
- Ambulance on the Information Superhighway, an inter-facility transportation clinical documentation tool.
- Nurse Advice Chat, an online chat function for the nurse advice center.
- Matching Clinical-Facility Data, tools to integrate various information sources to determine whether the physical environment, such as patient room characteristics, affect patient outcomes.
- Hospital Capacity Grid, a one-screen view of activity and capacity across a 21-hospital region.
- BirdDog, which sends lab results to the mobile devices of ED clinicians.
HIStalk Announcements and Requests
Welcome to new HIStalk Gold Sponsor nVoq. The privately held Boulder, CO company offers the SayIt speech recognition solution, exclusively endorsed by the AHA with vocabulary support for over 35 medical specialties. The SaaS-based SayIt is being rolled out in both ambulatory and inpatient healthcare settings, where users gain productivity within minutes as they dictate SOAP notes and other text directly into their EMR with no integration required, even using voice commands to navigate through their templates and operate other applications. SayIt is delivered as a low-cost Internet subscription, so users can use it at work, at home, or on the road. The company is interested in expanding its service delivery network and welcomes inquiries to VP/GM Debbi Gillotti. Thanks to nVoq for supporting HIStalk.
Here’s a video I found of Microsoft’s Bill Crounse MD talking about nVoq.
Acquisitions, Funding, Business, and Stock
Allscripts expands its stock repurchase program to $400 million from the $200 million that was approved a year ago.
Kansas City, MO startup Cognovant raises $500K in a seed round to launch its first product, the PocketHealth personal health record. The basic version will be a free App Store download, with paid upgrades available for versions that handle more complex needs and allow use by multiple family members. The founders are Joe Ketcherside MD and Stan Pestotnik RPh, who were executives at TheraDoc before it was acquired by Hospira.
McKesson announces Q4 results: revenue up 10%, EPS $2.09 vs. $1.62, beating expectations on both. Technology Solutions revenue was down 2% and profit was down 20%. John Hammergren said in the conference call that several Horizon Clinicals customers have committed to moving to Paragon and conversions have begun. He also said that while EMRs are important, customer success will be driven more by performance management, analytics, care coordination, and payor capabilities, and that RelayHealth is well positioned for the MU Stage 2 emphasis on connectivity.
Sales
Perry County General Hospital (MS) selects RazorInsights’ ONE-Electronic Health Record for its 22-bed critical access hospital.
Southwest Medical Center (KS) contracts for Summit Healthcare’s Provider Exchange for integration with physician offices.
West Tennessee Bone & Joint Clinic selects SRS EHR for its 11 providers.
Fletcher Allen Health Care (VT) will use the CapSite hospital purchasing database, which gives subscribers access to research studies and thousands of real-life contracts, proposals, and RFP responses covering healthcare IT, imaging equipment, professional services, and medical devices from 1,400 vendors.
Somerset Medical Center (NJ) signs a renewal agreement for secure e-mail services from Zix.
Perinatal Quality Collaborative of North Carolina will implement a wireless clinical support system from San Diego-based startup Cognitive Medical Systems.
People
The Allscripts board of directors elects Dennis Chookaszian as its chair. He was previously chairman and CEO of retirement advice site mPower and had retired in 1999 as chairman and CEO of insurance company CNA. He’s been on the board since September 2010.
New Jersey Hospital Association’s Healthcare Business Solutions affiliate appoints Michael Guerriero (MedAssets, Eclipsys) VP of business development.
Telemedicine provider Virtual Radiologic names former US Oncology COO George Morgan as CEO. He replaces Rob Kill.
Vocera Communications subsidiary ExperiaHealth names Elizabeth Boehm (Forrester Research – above) director of patient experience collaborative and Christine Henningsgaard (Accretive Health) national practice leader.
Elsevier promotes Hajo Oltmanns to president of its CPM Resource Center.
Joanne Wood, SVP of client services of Meditech and president and COO of LSS Data Systems, died Sunday, April 29. She was 58.
John Wade, former VP/CIO of Saint Luke’s Health System and former HIMSS board chair, passed away Saturday, April 28. He was 71.
Rick Brown, founder of the UCLA Center for Health Policy Research, died April 20 at 70.
Announcements and Implementations
Bon Secours Mary Immaculate Hospital (VA) goes live on Epic as part of Bon Secours Health System’s $200 million EHR initiative.
Lifepoint Informatics introduces CPOE Connect, a plug-in solution that allows vendors and commercial labs to offer seamless lab order entry using existing EHRs.
Preceptor Consulting, which offers go-live support and clinical training for EHR implementations, is supporting the implementation of the Cerner IView charting flowsheet at all campuses of Emory Healthcare.
In Canada, The Collingwood General & Marine Hospital goes live with PatientOrderSets.com.
Government and Politics
The American Hospital Association tells CMS that most hospitals will not be able to meet proposed Stage 2 Meaningful Use requirements, warning that, “many of the proposals put regulatory requirements ahead of actual experience with these technologies – an approach that will likely have unintended consequences."
Meanwhile, CHIME urges the government to give providers more time to prepare for Stage 2. Among its specific recommendations: a 90-day EHR report period for the first payment year in Stage 2.
The General Accountability Office (GAO) recommends that CMS verify provider requirements band collect more information before paying out EHR incentives.
Technology
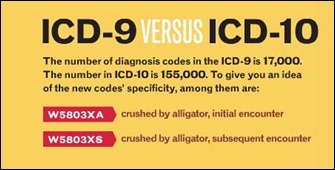
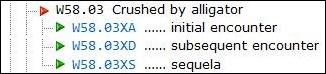
MedAptus selects problem search technology from Intelligent Medical Objects for its Professional Charge Capture solution, which will allow clinicians quick access to diagnoses when completing charge documentation using ICD-10.
Wyse Technology integrates Imprivata OnSign into its thin and zero clients, offering No Click Access for Citrix and VMware View that supports roaming between locations with badge validation.
Valued Relationships Inc. signs with AT&T to provide remote patient monitoring services for VRI’s nurse-staffed telemonitoring center. The service will capture information from wireless health devices in the home, such as scales and blood pressure cuffs, and issues triage alerts to the monitoring center when appropriate.
More information on the technologies used by Max Healthcare, the first two hospitals in India to earn Stage 6 EMRAM recognition from HIMSS. They include WorldVistA EHR (a free offshoot of the VA’s VistA), the open source Mirth integration engine, and a homegrown hospital information system. Dell Services manages its IT operations, including the EHR implementation, running all IT infrastructure into a private multi-protocol label switching cloud hosted at a remote data center.
In the UK, Blackpool Teaching Hospitals NHS Foundation Trust rolls out 900 Samsung Galaxy Tab tablets to clinicians in a deal with Vodafone.
A Massachusetts psychologist creates what she says is the first evidence-based treatment app for obsessive compulsive disorder. Live OCD Free costs $79.99.
Other
KLAS reports that half of providers anticipate buying or replacing a business intelligence solution in the next three years. In alphabetical order, the top five most considered BI vendors are IBM, McKesson, Oracle, QlikTech, and SAP.
![]() A Weird News Andy wannabe sends this story about man with a toothache who made a poor choice of dentists: the girlfriend he had just dumped. She sedated him and removed all 32 of his teeth, saying she had tried to remain professional, but couldn’t help thinking “What a b—–d” as he was unconscious before her. Most of us gals have had that feeling once or twice.
A Weird News Andy wannabe sends this story about man with a toothache who made a poor choice of dentists: the girlfriend he had just dumped. She sedated him and removed all 32 of his teeth, saying she had tried to remain professional, but couldn’t help thinking “What a b—–d” as he was unconscious before her. Most of us gals have had that feeling once or twice.
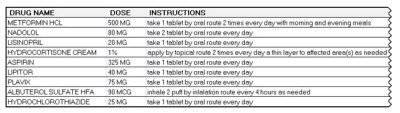
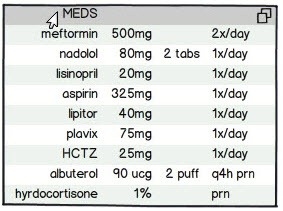
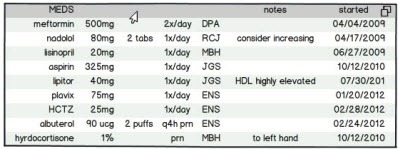
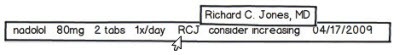
The real Weird News Andy wonders who will update EHR med lists if the FDA allows drugs for hypertension, diabetes, infections, migraines, asthma, and allergies to be sold without a prescription, possibly justifying that practice by requiring pharmacist counseling.
Here’s a fun SNL parody video that T-System created as an opening to its user group meeting. It has a lot of details that are worth a rewind, for instance at the 1:30 mark, where development VP Bill Hall is stereotypically sucking down what appears to be a Red Bull.
In the UK, North Bristol NHS Trust admits to a huge budget overrun in its second try at a successful Cerner rollout after problems with the first. Most of the extra money was spent on additional support people.
The Dr. Oz Show partners with Temple University Health System and Practice Fusion to run a May 19 “15-Minute Physical” event in Philadelphia, where 1,000 people will be screened and the resulting analytics report presented to the city by the end of the day.
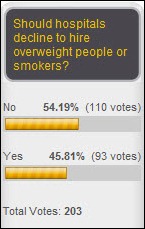
Facebook urges its users to post their organ donor status. Self-proclaimed pundits crow that Facebook is naïve in thinking that sticking a “donate” label on your profile provides legal consent, but they’re missing the point: the idea is to use social networking to encourage people to sign up with state registries. Your Facebook profile will outlive you, so your organs might as well follow its lead.
Sponsor Updates
- Cumberland Consulting Group promotes Saman Pourkermani to executive consultant.
- Merge Healthcare releases its Merge Honeycomb Archive archiving application.
- Beacon Partners is named by Boston Business Journal as one of the region’s fastest-growing companies.
- Baptist Health System (AL), INOVA Health System (VA), and Park Nicollet Health Services (MN) select LRS software for secure document delivery from their Epic footprints.
- T-System outlines its pending response to the proposed MU Stage 2 rule to ensure it addresses the needs of EDs.
- Olmsted Medical Center (MN) extends its partnership with MED3OOO through 2017.
- Teletracking hosts a free networking lunch May 11 in Baltimore featuring Kevin Capatch, director of supply chain technology and process engineering for Geisinger Health System.
- Intelligent InSites joins the Cisco Developer Network in the wireless / mobility category.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
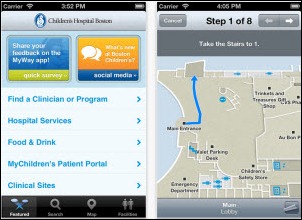
More news: HIStalk Practice, HIStalk Mobile.






















































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…