Top News

The FCC votes 5-0 to approve allow wireless patient monitoring systems such as those being developed by GE Healthcare and Philips to share a frequency spectrum that was previously used exclusively for aircraft testing. Hospitals using the new systems will be able to monitor patients anywhere in their buildings without connecting them to hard-wired instruments and limiting them to specific areas such as ICUs. In-home patient monitoring via Medical Body Area Network devices will also be supported, so that body-worn sensors can communicate wirelessly with an in-home station that will send data to a hospital or other provider.
Reader Comments
From Raydonia: “Re: downtime of Transcend Systems/Nuance on 5/21. They are paying full-time transcriptionists the princely sum of $60 for the day of downtime. As of this writing Tuesday, we are down again. It’s a big deal. At-home workers don’t have the rights that on-site workers have. Any questions and you’re told, ‘Be glad you have a job.’” Unverified. I’m probably the last person you’d want to have soothing you since I’m not usually too sympathetic to career-related gripes. If you don’t like the job and have better prospects, you should take the better job. If you don’t have better prospects, then I agree with the company – the market is telling you something and you should be glad you’re working since lots of people aren’t. In this economy, knowledge workers and those with skills that are in high demand but limited supply are going to be treated very well, but the rest will be have to reset their expectations since the threat of automation or offshoring is always there (hello, HP layoffs). I don’t mean to be a downer, but our parents and schools are feeding us the “dream big and do whatever makes you happy and you’ll be rich and famous” story that doesn’t usually match reality unless you’re freakishly smart, cunning, connected, hard working, or lucky. I think that’s one reason the unemployment rate isn’t going down much – people are holding out for yesterday’s comfortable, high-paying jobs that are gone for good for many of them. In your case, I concur that being paid a “salary” based on piecework seems odd, but if that’s the work arrangement you signed up for, then I guess being paid just the base amount for days you can’t work is consistent, even though it sucks when it’s not your fault that there’s no work to do (kind of like minimum wage restaurant servers who would starve without tips). Hopefully they’ve got their systems back to normal since I’m sure your hospital customers are as anxious as you are to reconnect.

From Pop Top: “Re: HL7. They are encouraging vendors to put the ‘Care Connected by HL7’ logo on their splash screens. Do you think any vendors will do this?” I don’t know why they would. Users are the ones who see the splash screen and they don’t care about HL7. Other than giving HL7 free advertising, I don’t see the benefit. And not to be overly critical since I’m probably the worst at aesthetic design (as readers who are always complaining about the HIStalk format can attest), but the logo looks kind of cheesy to me – harsh and badly proportioned wth an unpleasant 3D chiseled effect. Not to mention that the HL7 part of it, even though it’s their regular logo, is hard on the eyes. White on black looks like a DOS screen.
From Annie: “Re: Cerner. Consulting SVP David Sides resigned last week.” Unverified. His bio is still up and his LinkedIn profile says he’s still there.
HIStalk Announcements and Requests
 Some nuggets you might have missed this week from HIStalk Practice: former Medic and A4 CEO John McConnell shares insights on HIT startups, Meaningful Use, Allscripts, and more. Dr. Gregg discusses the data-drenched world of HIT and the need for tools to keep things simple. A glitch leads to the rejection of 450,000 Humana claims sent through the Availity clearinghouse. Is the direct primary care model just a new name for concierge medicine? My take on banning smart phone pics in doctors’ offices (hint: good luck with enforcement.) A physician seeks opinions on drchrono. ONC promotes device integration for ophthalmologists. What do these news bits, interview, and opinion pieces have in common? None can be found on HIStalk, meaning you best pop over to HIStalk Practice to ensure you remain in the know. While there, click on a sponsor ad or three and educate yourself on some cool offerings. And don’t forget to sign up for the e-mail updates. As always, thanks for reading.
Some nuggets you might have missed this week from HIStalk Practice: former Medic and A4 CEO John McConnell shares insights on HIT startups, Meaningful Use, Allscripts, and more. Dr. Gregg discusses the data-drenched world of HIT and the need for tools to keep things simple. A glitch leads to the rejection of 450,000 Humana claims sent through the Availity clearinghouse. Is the direct primary care model just a new name for concierge medicine? My take on banning smart phone pics in doctors’ offices (hint: good luck with enforcement.) A physician seeks opinions on drchrono. ONC promotes device integration for ophthalmologists. What do these news bits, interview, and opinion pieces have in common? None can be found on HIStalk, meaning you best pop over to HIStalk Practice to ensure you remain in the know. While there, click on a sponsor ad or three and educate yourself on some cool offerings. And don’t forget to sign up for the e-mail updates. As always, thanks for reading.
Listening: brand new from Slash, excellent guitar-heavy rip-it-up rock that’s loaded with licks reminiscent of the best of the 1970s and early 1980s: Deep Purple, AC/DC, Whitesnake, and of course Guns N’ Roses. Nobody’s making straight-ahead hard rock these days, especially the kind that sounds like a real band instead of one guy and a laptop. It doesn’t exactly break new ground, but it’s going to be killer at summer gigs like Rocklahoma this weekend. And I can’t help cheering for Black Sabbath, together on stage again (minus drummer Bill Ward over money issues) after a seven-year hiatus and Tony Iommi’s lymphoma, opening their Birmingham, UK show last week with 1971’s amazing Into the Void.
Dr. Rick is back from the NIST-ONC EMR usability meeting. I asked if anybody recognized him since I work in an anonymous vacuum and always wonder what that’s like. He said a few folks did, including Farzad Mostashari. Rick will be providing a meeting recap after he gets caught up on his ophthalmology work.
On Healthcare IT Jobs: Application Analyst II, Assistant Director IT-Medicine, Hospital Software Analyst II, System Architect, Cerner Testing Project Manager.
Welcome to new HIStalk Platinum Sponsor Clinithink. Healthcare solution vendors use the company’s cloud-based CLiX natural language processing engine to turn free text medical notes into fully coded structured data (ICD-9, ICD-10, SNOMED CT) that payers, providers, and analytics companies can use to improve quality, increase revenue, and meet reporting and regulatory requirements. Structured data entry via check boxes and drop-downs makes like easier for the computer, but the richness of the patient encounter is often locked away in the detailed narrative of those providing the care. CLiX converts that data to information for everything from capturing Meaningful Use measurements to providing doctors with smart search capability for research that understands “bronchial hyperreactivity” as being related to “asthma.” Thanks to Clinithink for supporting HIStalk.
Here’s an overview I found of Clinithink’s CLiX on YouTube. It shows the user’s narrative popping up SNOMED CT codes.
Acquisitions, Funding, Business, and Stock

Kony Solutions closes on a $15 million third round of funding, led by Insight Venture Partners.

Healthcare payment network InstaMed secures $14 million in new capital.

Shares of Scotland-based charge master systems vendor Craneware drop by 15% after analysts speculate that its US customers might be chasing Meaningful Use money rather than buying its financial software, at least until next year. The company indicated in January that the situation was exactly that, but predicted a quick reversal of the trend. Other analysts agree with that earlier assessment, saying demand is already recovering.

Compuware reports Q4 numbers: revenue up 21%, EPS $0.12 vs. $0.16. Its Covisint subsidiary, which offers HIE and cloud-based services for healthcare, had annual revenue of $74 million, up 34%.

Nashville Medical Trade Center signs its biggest tenant so far, the RFID in Healthcare Consortium trade group. It will use part of its 80,000 square feet for The Intelligent Hospital, the hospital replica you saw in the downstairs exhibit hall at HIMSS in Las Vegas earlier this year (it was doing big business each time I checked). HIMSS will have 25,000 square feet in the building, which has 1.5 million square feet.

University of Maryland spins off Analytical Informatics, Inc., which will offer radiology dashboards and eventually expand into BI and quality tools that cross systems.
Philips shares drop after its CEO warns that the European debt crisis may hurt imaging sales there.
Sales

Kosair Children’s Hospital (KY) selects Amcom Software’s clinical alerting middleware and smart phone communication solutions, planning to integrate it with their GE Healthcare Telligence nurse call system, GetWellNetwork interactive patient care system, and Cisco wireless IP phones and smart phones.
Omnicell closes on its previously announced acquisition of MTS Medication Technologies, a provider of medication adherence packaging systems.
Tri-State Gastroenterology Associates (KY) selects eMerge | ENDOTM for procedure documentation and workflow for its endoscopy center.
Lakeland Healthcare Group (IL) selects Merge Healthcare’s complete radiology cloud solution.

Indiana Orthopaedic Hospital selects the anesthesia information management system from Surgical Information Systems.
People

Former WellPoint VP Ryan Miller joins Availity as SVP of strategy and corporate development.

Todd Helmink (Allscripts) has joined The LDM Group as VP of strategic partnerships.
Greater Houston Healthconnect, a regional health information network, names Philip Beckett PhD (Baylor College of Medicine, RosettaMed) as CTO.
Announcements and Implementations
The US Olympic Committee announces that GE’s continued sponsorship will include the use of Centricity to manage the care of the 700 athletes participating in the London 2012 Olympic Games.
Iatric Systems and Order Optimizer announce the availability of an evidenced-based order set platform for Meditech Magic using Iatric Systems’ OrderEase solution.
MED3OOO announces the general availability of InteGreat EHR V6.5, which includes Quippe technology from Medicomp Systems.
RelayHealth and Greenway Medical complete a development agreement to exchange data between hospitals and ambulatory clinics.
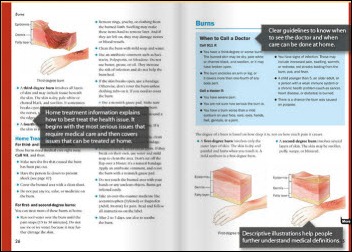
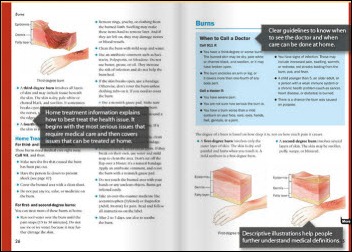
Healthwise wins a Center for Plain Language award for its course on coronary artery disease. The non-profit company’s course combines easily understood content that is personalized by user type (recent coronary event, someone whose symptoms have subsided, etc.) Healthwise has previously won similar awards for its arthritis and low back pain materials.
Government and Politics
Representatives Michael Burgess MD (R-TX) and Gene Green (D-TX) introduce legislation that would require states to require hospitals to disclose information on charges for certain inpatient and outpatient services and to require insurance companies to provide enrollees a statement of estimated out-of-pocket costs for healthcare services.

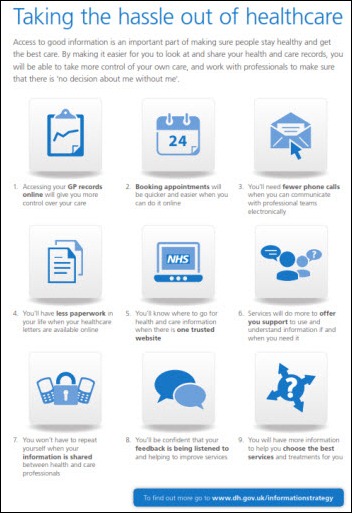
US CTO Todd Park, writing on The White House Blog, announces the Presidential Innovation Fellows program. He’s looking for 15 innovators to spend 6-12 months in DC starting in July to work on one of five projects:
- Open Data Initiatives (entrepreneurial use of government data for societal benefit, including but not limited to healthcare)
- Blue Button for America (consumer downloading of their own health information)
- MyGov (access to government information)
- RFP-EZ (development of a platform to make it easier for the government to buy technology from startups)
- The 20% Campaign (move US aid payments from cash to electronic payments)
Innovation and Research

Three students at a Ugandan university win a prize for their smart phone-powered fetal monitoring system, which analyzes fetal sounds and produces a plain-English description that midwives and birth attendants can understand. The device costs at least 80% less than an ultrasound machine.
A study finds that OptumRX’s text message prescription reminder program improved medication adherence, with 85% of patients taking their at-home oral meds correctly vs. 77% without the reminders.
Technology
Cerner is looking pretty smart for buying up 65,000 IP addresses from bankrupt Borders for $12 each. The IPv6 kickoff is in a couple of weeks, but the transition is expected to take up to 10 years, meaning Cerner hedged its bets in being able to run in dual stack mode with the additional old addresses.
Other

The main Delaware newspaper covers the Delaware Health Information Network, which it says has enrolled 92% of the state’s providers. The front page story’s key figure is Christiana Care Health System CIO and DHIN Chair Randy Gaboriault, who had a recent positive experience with the value of shared medical information during a heart attack scare. He says his mother was not as fortunate – she died a couple of months ago after being treated by an unconnected hospital that did not have her history available, which he is convinced led to her unfortunate outcome.

Fairview Health Services (MN) fires CEO Mark Eustis, presumably after being embarrassed by never-ending press caused by the heavy-handed patient debt collection tactics allegedly employed by Accretive Health, which he brought in. Of course he also could have been fired had Fairview lost a ton of money by not collecting aggressively enough, so there’s that fine line thing.
As already reported here thanks to a tip from reader Gran Cru, Partners HealthCare (MA) takes a $110 million write-down on its soon-to-be dumped Siemens financial system, dropping its Q2 net income to $5 million vs. last year’s $71 million. As also reported here, bringing in Epic will cost another $600-700 million.

A scrub nurse at a Washington urology practice sues Robert Weissman MD, claiming that he threw an intra-operative tantrum that included cursing at her, throwing instruments, and finally intentionally stabbing her in the finger with a needle that he had just withdrawn from a patient’s scrotum.

Weird News Andy finds this story to be weird and wonderful. A Baltimore area high school freshman develops a 3-cent paper sensor that can detect cancer by indicating high levels of a particular protein, making it cheap enough to use in routine screening. Over 200 researchers he asked to help him test his invention turned him down, but now he’s working with a Johns Hopkins researcher, he has won $75,000 in the Intel International Science Fair (above), he has patented his device, and a San Diego biotech firm has offered to help him perform the FDA-required clinical trials.
WNA also likes this spooky security camera video from the ED of St. John’s Mercy Hospital in Joplin, MO as it was being hit by a tornado a year ago.
Dr. Jayne wants to play Weird News Andy in finding this obituary of a “crazy woman” characterized by her family as “De Facto empress of the hell she lived in.” I almost ran out of fingers trying to tally her former / present, living/dead husbands, not to mention her “friends at the Lakeside Trailer Park.” The family also noted that among the folks who will miss her most are Anheuser-Busch, Philip Morris, and the Ohio State Lottery. Her loved ones concluded with some sound advice: “Everyone dies, but not everyone lives. Mom lived. She lived hard, but she lived full. So, ‘Don’t cry because it’s over….. Smile because it happened!’ Light your smoke and raise your glass and remember the last thing she said to you that made you laugh so hard you thought you were going to wet yourself; but this time don’t hold back. Because she never did. “

I was startled to see this pop up on my LinkedIn page.
The executor of the estate of a 102-year-old heiress says everybody robbed her blind before she died, convincing her to give them extravagant gifts. Her daytime nurse got $31 million, the night nurse was given $1.1 million, her two doctors got $3.1 million, and Beth Israel Medical Center got a $6 million Manet painting for allowing her to live in the hospital for years even though she was healthy. Her attorney says she gave the gifts because she was generous (and he got only $60,000).
Sponsor Updates
- Practice Fusion announces the availability of customizable endocrinology templates.
- Cooper Green Mercy Hospital (AL) goes live on Stockell’s InsightCS Revenue Cycle Inofrmation Management system, including patient access and patient accounting.
- TELUS Health Solutions and Orange partner to develop remote monitoring solutions for chronic disease patients.
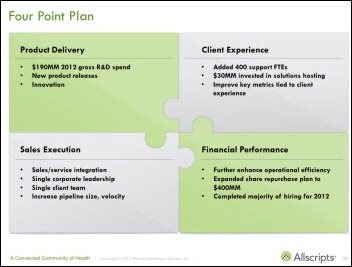
- Allscripts releases a white paper by CMOs Doug Gentile MD and Toby Samos MD that explores insights from ACO pioneers.
- Lifepoint Informatics is sponsoring G2 Intelligence’s Laboratory Outreach Conference June 6-8 in Las Vegas.
- The Advisory Board Company’s Crimson team will lead two breakout sessions at the 3rd Annual Health Datapalooza June 5-6 in Washington, DC.
- CareTech Solutions announces that its clients Barnes-Jewish Hospital (MO), Touro Infirmary (LA), and Wheaton Franciscan Healthcare (WI) have won 2012 Aster Awards for their websites.
EPtalk by Dr. Jayne

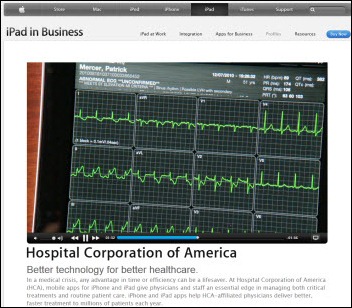
Is it easier to focus when viewing content on an iPad vs. a television? Maybe. Pediatric neuroscience researchers note that while children will look away from a TV screen 150 times per hour, they are less likely to look away from an iPad. This is felt largely to be because of the touch interface being directly aligned with the action on the screen. This could help children learn more effectively, although scientific studies of how devices affect child development can take three to five years. The iPad’s relatively short time on the market in effect makes all of us (not only children) guinea pigs.
Seasoned IT staffers sometimes comment to me that new physicians seem like they’re getting younger. Recent actions to shorten medical school may make this more of a reality. Citing the nationwide shortage of primary physicians as well as increasing student debt, schools are compressing primary care training. Those who have already decided to pursue careers in primary care will experience fewer vacations and elective courses. Schools are also offering accelerated programs for certified physician assistants who want to pursue medical degrees.

With smart phones being everywhere, practices are considering asking patients to refrain from taking pictures while receiving care. Although providers are mandated to maintain privacy, patients are not. I was reminded of this a couple of years ago while riding on my hospital’s float in a community parade. A patient stepped out from the crowd and called up to a surgeon riding next to me, “Hey doc – my husband’s hemorrhoids are much better!” (And yes, those are cow-print balloons.)

One of the challenges of being a medical informaticist is doing the right thing with data. The recent USPSTF recommendation against routine PSA-based prostate screening is an interesting case study in data-driven clinical decision making. Numerous consumer groups are coming out against it, much like they did with revised mammogram recommendations in 2009.
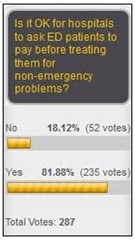
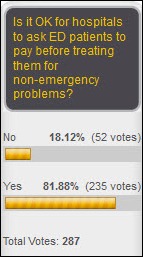
Several readers responded to Monday’s Curbside Consult that discussed whether patients presenting to the emergency department should pay before being treated for their non-emergent condition. One reader notes,
One strategy implemented in a southwest US health system was to assess but not treat such patients. A triage nurse did the full assessment and scheduled them with a new PCP in the a.m. This reduced ED use by the patients over later months. They even had virtual staff to interview and set up the follow-up for smaller EDs. I think this was presented at the last CHIME meeting.
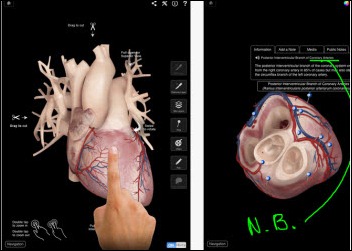
Isabel Healthcare releases a mobile version that offers Apple-using clinicians additional clinical decision support at the point of care. Subscriptions are available in weekly, monthly, and annual varieties, making it ideal for rotating medical students and occasional users. I’ve used Isabel (via EHR integration) for some time and it’s extremely valuable.

Florida State University researchers have created the Pacifier Activated Lullaby device, which musically reinforces premature newborns who must develop the ability to coordinate a suck / swallow / breathe response for feeding. The specially wired pacifier and speaker system plays a lullaby each time a baby completes a successful sucking motion and has resulted in shorter hospital stays and reduced costs. The FDA-approved device reduced neonatal ICU stays by an average of five days. It’s a cool an innovative device that I almost missed reading about – the sending address on the press release had University misspelled, making me think it was spam.

Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.









































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…