HIStalk Advisory Panel: IT and Patient Outcomes 8/15/12
The HIStalk Advisory Panel is a group of hospital CIOs, hospital CMIOs, practicing physicians, and a few vendor executives who have volunteered to provide their thoughts on topical industry issues. I’ll seek their input every month or so on an important news developments and also ask the non-vendor members about their recent experience with vendors. E-mail me to suggest an issue for their consideration.
If you work for a provider organization (hospital, practice, etc.), you are welcome to join the panel. I am grateful to the HIStalk Advisory Panel members for their help in making HIStalk better.
This month’s question: Why has healthcare IT not uniformly improved patient outcomes?
Vendors and Products Don’t Align with Clinical Needs
- Doctors don’t see technology as an ally in helping them take care of patients. Please see the article recently published on Medscape. The default mode of healthcare practice in the US is to practice defensive medicine (defense against lawsuits). Examples like those given in the article above don’t raise a healthcare provider’s confidence in technology. Notice how the article specifically gives the example of vendor contracts that say if something goes wrong using our technology, it’s not our fault.
- We have focused on a computer fixing a workflow problem while at the same time becoming more dependent on computers to tell staff what to do.
- With few exceptions, the vendor community supports our efforts to enhance and embellish the product with each deployment. In some cases, neither the vendor nor the client has an incentive to collaborate with other vendors, or other clients, to ensure that every deployment of IT is better than the previous one. This is getting better, but we still have much to do in this regard.
- Some outcomes take a long time to improve, longer than the HC IT has been in use. Some HC IT focuses too much on documentation without a balanced approach to deriving outcomes information let alone being integrated into the care process sufficiently to affect outcomes.
- The answer is in part within the question: IT implementation has not really been uniform across the care spectrum. As most realize, systems are often if not usually built from a developer / programmer standpoint, reaching out to address a problem rather than starting with a problem (or "job to be done") and working back to develop the necessary system to perform that job. This has lead to numerous issues of usability, human-computer interface problems. More importantly, and more fundamentally, many systems simply aren’t designed to improve patient outcomes. They’re built from the start to support billing, financial management, documentation, etc. As a corollary to the above, rarely is the clinical environment placed at the center of the system. This is evident in the approach vendors generally take with deals: focus on administrative and IT needs (decision-makers) with lesser attention devoted towards those who both use and see the actual patient effects.
- The Jurassic Park line, “Just because we could does not mean we should"says it all. Not every EMR or HIT app needs to be adopted or will prove to be of value. Not all of them are created equal. In many instances, it has been the technology that drove the cost with very little benefit.
- Clinical decision support that follows the rights (right clinician, right intervention, right time, right level of alert logic, right ease of use ) is almost non-existent, except for the simplest medication alerts. Apologies to Jerry Osheroff, I don’t think he gets this quite right. Until the biggest EHR players improve their CDS functionality, and there are good guidelines for turning structured knowledge into CDS, I don’t think we will get very far. We will, but I am waiting for the ability to use a general purpose programming language on data in the EHR to create new levels of CDS that are actionable. Further, I bet not much of this happens locally until the EHR players are forced to have some "skin in the game", some liability for the CDS that is already baked into their model install. It is just silly that each of 5,000 hospital CDS committees have to decide whether an aspirin after an MI is a good thing, or whether you ought to check a cholesterol every couple of years on a statin.
- There are many factors that contribute to uniformly improving patient outcomes. But one issue that is still a work in progress is developing and deploying a system to provide the right information to the right people in the right place at the right time. Integrating data on previous care that a patient receives from their primary care physician during regular clinic appointments, with emergency encounters, possible inpatient episodes, care provided at an ambulatory care organization, etc. pose a unique challenge to collect all of these disparate encounters and the data generated. While EHR systems bring together some of these important data elements, there are still gaps (for example — data on an emergency room visit while a patient is out-of-state on vacation). Additionally, even if data is integrated together, all of these indicators and data points need to be filtered and targeted to improve upon a specific outcome (e.g. reducing the likelihood of myocardial infarction readmission). Recommendations on improving outcome and supporting information need to be concisely delivered to the proper places when care is provided, to the physician when a patient presents at the emergency room with chest pain to the care coordinator prior to discharge.
- While there has been considerable time spent integrating healthcare IT into related systems of care, there needs to be a more systematic approach, time and resources spent integrating into the process of care – specifically clinician workflow so the tools are optimized.
Usability/Integration Issues
- I think Dr. Rick’s excellent articles have shed light on the usability issues of EHRs. He mentioned some data on how short-lived human working memory is. EHRs can take 5-10 seconds to respond to every mouse click. These long delay times make it difficult to keep a coherent stream of thought going when documenting, especially when providers get interrupted (appropriately) by office staff who need something or the other. In the end, what gets produced are long canned narratives about generic patients. When the note is read a few days later by the provider or someone else, they see a generic note that tells them little about the patient. Our EHR would take 45 seconds to a minute to open a chart in the mornings. By the late afternoon, it was five minutes to open a chart. That’s typically caused by memory leaks. We (a medical clinic) had to call a technology firm that says its been in business for 20 years to tell them they had memory leaks! Now all charts take about 45 seconds to open.
- The main problem is usability, which involves both design and implementation. Many HIT systems are simply not designed well. They are often trying to "replicate the current way of doing things" with the idea that this will improve adoption. However, it turns out that computers are lousy at being paper, and so can never match up. However, computers are really good at being computers, and so the best HIT software takes advantage of the unique properties (e.g. complex data analysis, data visualization) and enables a better experience. Additionally, good design should start with observing the real needs of the end user (not just listening to what a user thinks they need), and most importantly should involve an iterative process which acknowledges that the programmer and physician should work closely for months to fine tune a system. However, the second problem may be even more worrisome. The same EMR system can be implemented in so many ways that the results can range dramatically. A recent editorial talked about how EMRs cost a lot, and slow down doctors, and introduce new errors, and are thus not ready for prime time. But the fact is that while this is a reasonable conclusion based on many experiences, it is a short-sighted view of the potential of what can happen when a good EMR is implemented well. I think the best use of an EMR is to allow for automation and delegation of various parts of the workflow to empower a team to do more care and to do it consistently – thus resulting in both higher quality outcomes as well as less work for physicians.
- Technology in and of itself is useless and even detrimental unless built and used correctly. In order to have a positive patient outcome, in my mind, a technology theoretically should be easy to use, be actually useful (for the user or the patient), and have minimal negative impact (on workflow or patient care). A breakdown of any single one can result in a subpar result. Patient outcomes may not have improved universally because current healthcare initiatives don’t necessarily encourage focus on all items. Also things like “usability” can be oftentimes extremely difficult to create.
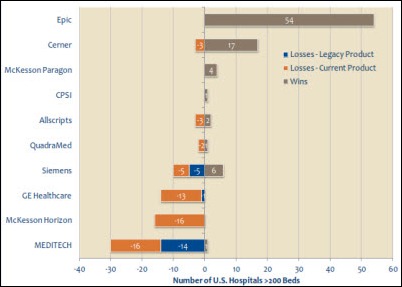
- The hodgepodge of company acquisitions that has created a market where products have never been integrated. One of the reasons Allscripts is collapsing is because of an inability to integrate Eclipsys products. I find it hard to believe that companies that size, with the resources they have, can’t integrate two products. Clinicians have to sign onto several products multiple times a day to get information they need. It is guaranteed that in such a system there will be conflicting data in different databases increasing the risk of patient harm. Maybe this makes systems like Epic better, but that also stifles innovation. EHRs aren’t going to improve with markets dominated by companies like Epic as is being demonstrated everyday right now.
- Too many disparate systems that don’t talk to one another. Even with HL7 messages, there is still a lot of variance. All it takes is sending something in the wrong HL7 field to cause a problem.
It’s the User, Not Just the Technology
- A dependency on the skill and performance of the user related to the IT solution in question. The use of the word "uniformly" makes me consider that every user will create a different outcome. As an example, an electronic health record relies on inputs from various sources in order to aggregate the patient history and then present a user with information to make decisions. The term "decision support" is bandied about with great import these days but as the term implies the tool is there to simply support the clinician’s capability to make a decision. Almost all technology is just that, a support system to assist the clinician or user. The same can be said of a technology such as the Da Vinci Robotic Surgical System. In the hands of a great surgeon, the outcomes can be outstanding. In the hands of a first year surgical resident, the outcomes probably will not be the same.
- That is like asking why the carpenter’s apprentice who was recently trained on how to use a hammer, router, etc. (insert your specialized tool or technique of choice) hasn’t improved his/her ability to create beautifully crafted cabinets or furniture. It takes time to become competent, proficient, and then the master of skills with the usage of newly introduced and evolving tools. This describes skills improvement for the individual. To obtain uniformly improved skills and thereby products / outcomes, it takes even more time to build an organization or industry of skill masters. Our digital society that expects instant gratification and results has forgotten that it takes time and commitment to master skills and provide high quality products and services. This obviously is an oversimplification, but I think an appropriate analogy to the usage of a healthcare IT to improve outcomes.
- While this question is understandable given all of the federal government’s promises and expectations of what HIT will do to improve patient outcomes, the question reveals a lack of understanding of what IT in general can and cannot do. Healthcare IT (and in fact any IT investment) on its own can do nothing; it is only when used in conjunction with improved workflow and processes that patient outcomes can be improved. That is what we should be measuring. There is a reason why IT is called an “enabler”, and a “complementary” technology (like electricity). On its own, IT (like electricity!) has no value, and therefore won’t (can’t) improve anything. It has to be used in conjunction with changes in workflows and processes in order to improve outcomes.
- The effective deployment of technology has a number of requirements, of which the actual technology may be the smallest piece of the puzzle. At the end of the day, improved patient outcomes are a combination of provider decisions and judgment, patient compliance, adequate monitoring of efficacy of treatments and the use of technology to support all of those. The last item on that list is dependent upon the provider learning and adopting the technology to its full (not necessarily fullest) capabilities. Any one of these factors has the potential to derail the process, so if we don’t look at the process holistically, we shouldn’t expect uniform improvement.
- Lack of leadership on the provider side and lack of appreciation and understanding of HIT on the hospital executive side (one executive in charge of 11 hospitals did not know who Todd Park is).
- Ultimately it is not HIT by itself that will change outcomes, but what people do with it and how providers use it. Even HIT left unchecked can be harmful. I made more mistakes with electronic prescribing than I ever made on paper. I do not believe that we should stay on paper at all, but until we are all connected out there on the Medical Internet and the information flows freely, we will not reap the benefits of technology. One article in the Economist called "When the carpet calls the doctor" failed to explain how a device attached to the carpet that sends a signal to the doctor when the patient is about to fall is going to prevent that fall. Is the doctor or nurse supposed to get in the car or fly to the rescue? How about the apps that would monitor the patient’s weight or glucose — what will one do if the patient will not use it? Who is going to sit in a tower 24/7 to monitor all this and who pays for it? Not much is being said about that. As excited as I am about HIT, I do realize that our bigger-than-life expectations may not be materialized — not soon enough, anyway. Hope this helps, as it is written in between rounds at three hospitals, two of which are still on paper.
- Because IT alone won’t accomplish anything. If you take a bad process and simply duplicate it with IT solutions, you still have a bad process.
- I would be mildly surprised if it had. In my view, outcomes will improve with decreased variability (with the most likely shapes of the outcome curve you can prove this mathematically) and clinical decision support. Theoretically, EHRs reduce variability with templates and order sets, but I have seen few real world examples of templates standardizing care, except in very limited areas, like DVT prophy. Clinicians still go off and do their own thing after the initial orders are in, and the templated H+P is done.
Variations in Implementation
- Probably the top reasons would include: variability in the technology itself, variability with the implementation, and variability of the adoption/use of the technology by the end users. All of those areas of variability exist at every hospital (even those within larger health systems who attempt to "standardize" their efforts). It should surprise no one, then, that "Healthcare IT" does not have uniform results. A poor implementation of even a very good technology solution will not have the same results as a good implementation. Similarly, poor adoption will not yield results from the effort to implement the technology (or may yield negative results directly due to the hybrid environment created by poor adoption where some are using and others not using the technology). Additionally, any negative outcome will be blamed on the new technology being implemented even if something else is actually to blame. However, I would posit that a good implementation with good adoption and engaged end-users with even a mediocre technology solution has the potential of generating positive results for patients.
- There is nothing uniform about the way we deploy healthcare IT solutions. We are often inwardly focused and insular as we define, design, and deploy the solutions that we must implement. We are often working very hard to leverage the technology we have acquired so that we can make the best use of scarce resources. We seldom take the time to measure our own local progress. We surely struggle to make time to share lessons learned with others. Our local efforts often limit the extent of our reach, while also limiting our ability to measure what impact we may have had.
- Just because your facility has implemented an EMR system, regardless of how mature the model is, it doesn’t mean the facility is using that technology to improve outcomes. Case in point: our facility is in the last stages of an EMR implementation. We are incorporating what our clinical team believes is industry best practices and evidenced based care i.e. Elsevier and Zynx, and we are going to reduce the variation in care that not only drives cost up but produces varying outcomes. We went on a site visit to a hospital who has already implemented this system but are using terrible practices. That is not the fist place we went where we saw this. It takes real leadership to stand up and say we are going to do it a specific way that uses evidenced based/best practice care. The IT systems can readily support an organization who is trying to do this with real time clinical behavior reporting. This will start to drive outcomes.
- Healthcare IT has not been uniformly distributed. The inequity among hospitals will be even deeper. Hospitals that are EMRAM level 6 or 7 and hospitals in rural areas that could benefit the most from health IT but cannot afford it.
- Lack of consistent adoption. Lack of understanding on how some technology can impact outcomes. Lack of discipline in organizations to use what they have. Poor BI use that would help isolate areas of improvement.
Lack of IT Support
- The CIO/IT Director doesn’t always get it. If we don’t understand the business of our organization, there is no way that we will provide the tools necessary to analyze / improve our business. A good example is that of business intelligence. My organization doesn’t think it is necessary or quite frankly, even understands what it is. I know that we have to have better analysis, and that in order to do that, I have to provide the appropriate tools. If I wait till the organization gets behind BI, it won’t happen for another 2-3 years and then it will be too late. I’ve searched out a solution that makes sense in our environment and began the implementation 12 months ago. The next step is to push it out to the organization and educate the management team on its value.
Meaningful Use has Distracted Clinicians and Vendors
- The emphasis on Meaningful Use metrics over the past years has led to a significant percentage of adopters to be focused almost exclusively on meeting those criteria that would allow for bonus attainment. These tools have the possibility to bring focus to a singular patient’s health issues and treating that patient as a unique individual with unique needs. This can be done efficiently and effectively when the clinician is able to utilize the tool as they see fit. Instead the clinicians become distracted by unnecessary hurdles mandated by someone sitting on Capitol Hill. The emphasis on evidence-based medicine and population health also distracts somewhat from the unique physician / patient experience by moving the focus up a layer or two from the primary interaction. Eric Topol has written a great deal about this.
The Healthcare Business Model Stands in the Way
- Our supply driven healthcare system and culture that needs to change. For-profit HIT, hospitals, and so on that has made us pursue the highly profitable but not always the most cost effective or valuable course of action.The only one whom I saw commenting on that was Peter Orszag, who said that it will be difficult to reconcile years of marketing in healthcare and direct-to-consumer advertising with customer satisfaction and reducing costs. We want to retire on 401(k) plans that invest heavily on healthcare companies and we want them to be profitable, but squirm when it comes to paying for it and attempting to cut cost. We cannot have it both ways.
Benefits Will Be Realized Only when Quality can be Measured
- Most providers / clinical entities are still trying to get past the data entry hurdles. Not yet at a point where most are focused on measuring quality. No defined quality standards that most agree on. Multiple groups with multiple standards, and these are not aligned with EMR companies.
- There is nothing stable about the environment into which we are implementing systems. The regulatory climate, the scientific environment, and the relentless pursuit of discovery creates a dynamic setting into which we are deploying systems. Collectively, this often prevents us from thoughtfully, comprehensively, and accurately measuring the impact of our implementations. So to some degree, we don’t really know if we are making a difference. We don’t always measure the things that matter, and sometimes we aren’t certain of the aggregate benefit of our collective actions.
- Healthcare IT has not uniformly improved patient outcomes because we have few clinicians with sufficient vision and understanding of the potential that can, in turn, influence the change. The CIO/Clinical IT employees cannot produce the level of influence needed and it will take a lot longer to move from a world of data collection to a world of data analysis. In addition, we still take too much of an individualistic approach to patient treatment. Evidence-based medicine has not been accepted in any of the organizations with which I’ve been affiliated.
- There have not been enough in-roads in the establishment of systems where data has been uniformly stored and then shared. Taking those outcomes and running them through statistical engines is the holy grail to improve outcomes. It takes time to build the foundation to support this future endeavor.
- Patient outcomes have not been well defined and continue to elude us. A patient who does well after open heart surgery may do so because he has a supportive family as opposed to one who lives alone. HIT cannot alter that; it can only help measure it.
- Our litigation-crazy society has made it almost impossible to share and be transparent about mistakes and medical errors,HIT induced or not.
- I do not believe we learned any lessons yet. Someone should interview those hospitals that spent in the $100 million range IT budgets or the ones that made mistakes so we can all be enlightened.
- The most obvious answer is that healthcare IT has been used in different ways, and to different degrees, from one provider to another and from one department to another. Now that healthcare IT is becoming more broadly adopted, and as advanced analytics are developed to empower caregivers more, patient outcomes are expected to improve. Any discussion of outcomes should recognize its limitations. For example, some medical conditions lend themselves to objective measurements of improvement, while others don’t. Despite the extreme complexity of healthcare, there’s a natural desire to measure the end result, the output of the process, in objective and simple terms. Did the patient get better? If so, how much? Did the patient population get healthier? If so, how much? But not every patient with the same diagnosis(es) will get better in the same way. Can an objective measurement adequately convey the difference? Some patients won’t get better at all. For a terminal patient released to hospice, for example, shouldn’t we instead be asking whether the patient and loved ones feel they were treated with respect, dignity, and compassion? For them, that is an outcome. Acute care hospitals should follow the lead of the subacute sector, which focuses heavily on such measurements. For non-terminal cases – those that indeed may be expected to get better – were they and their loved ones kept informed throughout the stay, or did they feel frustrated by a disjointed, piecemeal system of specialists, which mostly kept them in the dark? Were they informed and guided through decisions? These considerations should be incorporated into any meaningful discussion of "outcomes."
















































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…