News 11/16/12
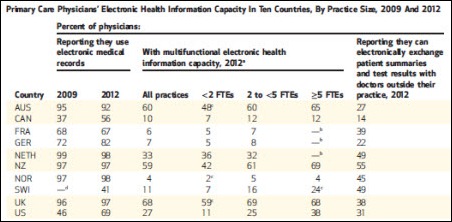
Sixty-nine percent of US primary care physicians report using EHRs, up from 46 percent in 2009, while about a third of doctors say their patients have the ability to e-mail the practice and have online tools to request appointments, referrals, and prescription refills. The study of 10 “high-income” countries also finds that despite health reform initiatives, a high percentage of physicians in all countries complain of untimely access to information from hospitals and specialists.
From Mango Mel: “Re: UNC. As you mentioned, they are going Epic.” I heard that rumor again today from an excellent source. If it’s true, that gives Epic all of the big hospitals in the Triangle area of North Carolina, which is almost all of the beds there now that they’ve recently added Duke and the just-announced WakeMed. Other NC users of Epic are New Hanover, Vidant, and Novant.
From The SFTreat: “Re: GE Healthcare layoffs. True – a number of staff from the Seattle office are gone.” We’ve run several rumors suggesting that the layoffs were going to happen Wednesday. A Boston article says the company confirmed that 10 percent of its Vermont workforce has been let go, but the company declined to give specifics. Our GE contact said that fewer than 50 employees were impacted and no office closures or product retirements were involved. According to the official response:
“In fact, GE HCIT is maintaining its focus on the needs of integrated care delivery, and in conjunction with our strategy, we are making choices to redeploy some portions of our resources and capital into new areas of product and service innovation. While these types of decisions are never easy in the near term, we are confident that they are necessary to meet the current and future needs of our customers.”
From Candace: “Re: research and think tank institutions for healthcare technology. What do you think of IDC Health Insights? Can you recommend other research centers? I’m a recent college graduate doing a research project.” I don’t have any experience with any of them, so I’ll open the floor to readers willing to help. Don’t they sound like swell places to work, though, just sprawling back at your desk thinking in a swanky office park?
From DeanInsider: ”Re: rumor of doctor resignations. Not the case. Dean is pleased to have become an Accountable Care Organization and has always put patients first.” I assumed that was the case, but several hospitals have announced layoffs they’re blaming on PPACA. The latest: Wake Forest Baptist Medical Center, which will eliminate 950 positions. A local professor there says hospitals must plan for at least one year of lower payments, reductions in federal grants, and the high cost of EHRs.
HIStalk Announcements and Requests
nice “@ingahistalk: Bowtie Confidential 11/10/12: Tweet Accountable Care Act and its Effects on the Board of Directors bit.ly/S9bQkV”
— Farzad Mostashari (@Farzad_ONC) November 11, 2012
HIStalk Practice highlights from the last week include: MGMA members give Medicare the highest marks among seven top payers. The country will be short 52,000 family physicians by 2025. An 87-year-old doctor who charges $5 an office visit says he didn’t select his profession for the money. Physicians must participate in PQRS in 2013 to avoid 2015 penalties. A list of the worst passwords for 2012. Rob Drewniak of Hayes Management Consulting discusses the need to educate board members on the ACA and its implications for their organization. Dr. Mostashari, by the way, gave Rob’s post a thumbs up. If Dr. Mostashari is reading HIStalk Practice and you aren’t, maybe it’s time to consider what you’re missing. Thanks for reading.
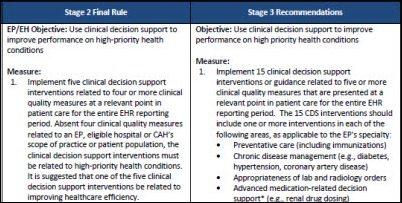
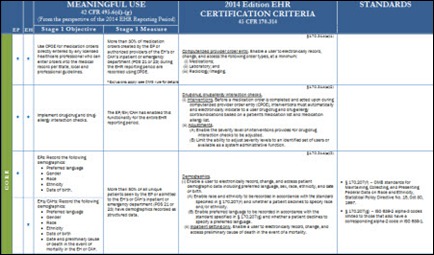
We ran a link to the draft Meaningful Use Stage 3 rules earlier this week, but just to be clear, this is a draft document not yet available for public comment even though its title is “HITPC Stage 3 Request for Comment.” You’re seeing it as it came from the Policy Committee.
Inga’s been a good girl this year, so here’s her Christmas list for your consideration: (a) sign up for spam-free e-mail updates to HIStalk, HIStalk Practice, and HIStalk Mobile; (b) friend, like, and connect with us on all the social not-working sites; (c) send us news and rumors; (d) review and impulsively click some of the much-appreciated sponsor ads to your left, search and navigate to their details in the Resource Center, and send your consulting RFI viral with the RFI Blaster; (e) tell other folks you read our sites because when it comes to our marketing channels, you’re all we have; and (f) give yourself one of those wrapping-your-arms-around-yourself hugs and pretend it’s Inga since it will take her awhile to get to each reader personally. I’m just happy reading down the list of 2,850 impressive folks who have signed up for Dann’s HIStalk Fan Club and thinking how cool that is. That’s the first place I look when considering somebody’s request for an HIStalk-related favor.
On the Jobs Board: Workflow Automation Project Manager, Technical Trainer, Product Analyst, User Interface Engineer.
The most common grammatical crutches I have to edit out of the interview transcripts I run, sometimes in truly startling numbers: (a) “really”; (b) “sort of”; and (c) starting sentences with “so” like someone telling a bar stool yarn. I was at a doctor’s presentation today and counted the number of times she said “sort of” and was up to 79 in the first 30 minutes before I tired of the exercise. I’m not annoyed, just sorry that the power of what she was saying was needlessly diluted by subconscious speech tics.
Acquisitions, Funding, Business, and Stock
CACI will acquire Emergint Technologies, a provider of HIT services and analytics solutions.
WellStar Health System pays $20,000 for the trade name, trademark, and other assets of the bankrupt Center for Health Transformation, the for-profit healthcare think tank founded by Newt Gingrich. WellStar intends to convert it to an independent, nonprofit collaborative of 20 non-competing health systems in the Southeast, focusing on sharing ways to improve quality and reduce costs.
Salt Lake City-based Remedy Informatics gets a $6 million investment from Merck. The registry and research informatics company is headed by Gary Kennedy, so I assume it’s related to the former RemedyMD. I interviewed him in early 2007 and was pretty impressed, although the hospital-type database products seem to have been de-emphasized in favor of the life sciences ones.
Sales
WakeMed Health & Hospitals (NC) will invest $100 million over five years to implement Epic.
The DoD and VA award Document Storage Systems an EHR integration subcontract.
Oakwood Healthcare (MI) renews its multi-year IT outsourcing contract with CareTech Solutions for $120 million.
People
Harry Jacobson, MD, former vice chancellor for health affairs at Vanderbilt and CEO of Vanderbilt University Medical Center, joins digiChart as chairman, replacing G. William Bates, MD, who was recently named chairman emeritus.
Net Health systems, a provider of IT systems for wound care, hires Kelley J. Schudy (Allscripts) as VP of sales.
Announcements and Implementations
The National Basketball Association will use Cerner’s HealtheAthlete health management platform for all of its teams.
The LSU Interim Hospital and 11 clinics are live on the Greater New Orleans HIE, which will connect to the state-wide Louisiana HIE by the end of the year.
The Pennsylvania eHealth Collaborative signs up 3,449 providers for DIRECT messaging, exceeding the federal government’s goal of 1,000.
Lakeland Regional Medical Center (FL) goes live on Cerner clinical applications with implementation assistance from Healthcare Clinical Informatics.
Elsevier announces the launch of Health Care: The Journal of Delivery Science and Innovation. It will focus on applied healthcare IT and health reform. Founders and co-editors are Amol Navathe, MD, PhD (Brigham and Women’s, Harvard Medical School, Wharton School) and Sachin Jain, MD, MBA (Boston VA, Harvard Medical School, and Merck).
North Mississippi Health Services (MS) wins a Baldrige Award.
Innovation and Research
Got a flair for design and patient-friendly medical information? ONC and VA are running a Health Design Challenge for creative types who can make CCD/Blue Button information easier for patients to understand. Three prizes are offered in each of four categories (Best Overall Design, Best Medical/Problem History Section, Best Medication Section, and Best Lab Summaries) ranging from $1,000 to $16,000. The deadline is November 30.
Other
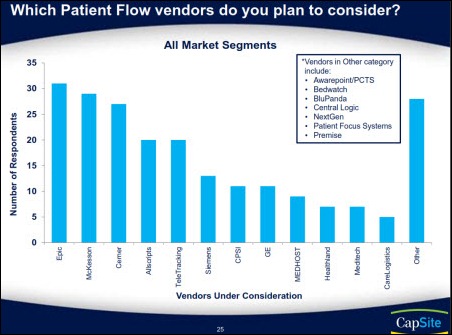
A CapSite study finds that almost one-third of hospitals plan to invest in patient flow solutions within the next two years. Leading vendors include TeleTracking, McKesson, Epic, and Meditech, while the vendors most often being considered are listed in the graphic above.
Speaking of CapSite, a HIMSS webinar this Friday afternoon will cover “The CapSite Acquisition and What It Means to You.”
Bill Hersh provides an update on the clinical informatics subspecialty for physicians. Details are being worked out about the grandfathering and initial exam process, but Bill says the first candidates will sit for their test in October 2013.
Allscripts responded to our reader’s question about whether MyWay users will be released from their contracts if they decline the company’s offer of a free upgrade to Professional.
“Allscripts is providing a free upgrade, and the contract does not allow for cancellation of current leases. Allscripts is dedicated to working with our clients to help them succeed, and we believe the upgrade provides the right benefit for the long term.”
Weird News Andy says this never happens to him while listening to NPR. A former Doctor of the Year ED doc faces a long list of charges after hitting several cars in a parking lot while allegedly under the influence of drugs and alcohol with NPR cranked up loud in her Outback. She says her accelerator got stuck on her way to Whole Foods to buy a Thanksgiving turkey, but police found pills and prescriptions she had written for herself.
WNA labels this story “Hello Terry Schiavo.” Scientists performing a functional MRI on a man who has been in a vegetative state for 10 years find brain wave patterns that suggest he is answering the questions they’re ask him. The scientists believe the patient is aware of who and where he is.
Sponsor Updates
- Leslie Kelly Hall, SVP for policy at Healthwise, joins a panel discussion on patient engagement framework at next week’s National eHealth Collaborative Webinar.
- Visage Imaging will demo its Visage 7 processing technology, including work-in-process capabilities, at this month’s RSNA meeting.
- Merge Healthcare will unveil its mobile and Internet platform for patients during RSNA.
- Greater Baltimore Medical Center (MD) reports a reduction in paper output and waste since deploying Access Intelligent Forms Suite and Wacom STU-500 signature tablets.
- TeraRecon previews a pay-as-you-go option for use of its iNtuition advanced visualization tools by physicians who perform aortic repair procedures.
- Kareo offers tips for increasing practice revenue in its November newsletter.
- The Canadian Health Informatics Association awards TELUS Health Solutions its Corporate Citizenship Award for achievements in health and technology to improve patient outcomes.
- McKesson will combine its Episode Management software with the Prometheus Payment model to support large-scale bundled payment programs.
- DrFirst will embed Halfpenny Technologies’ Integrated Technology Framework for CPOE and results delivery within its Rcopia e-prescribing platform.
- White Plume Technologies’ Laura DeBusk and MED3OOO’s Cindy Cain will discuss the impact of ICD-10 on operations, compliance programs, and cash flow in a November 29 Webinar.
- Aprima will integrate Alpha II claim scrubbing technology into its EHR and PM solutions.
- HIStalk sponsors earning a spot on the 2012 Inc. 5000 List of America’s Fastest Growing Companies include Beacon Partners, Culbert Healthcare, Cumberland Consulting, Digital Prospectors, eClinicalWorks, Enovate IT, Etransmedia Technology, Greenway, GetWellNetwork, Hayes Management Consulting, Kareo, Iatric Systems, Impact Advisors, Ingenious Med, iSirona, maxIT Healthcare, MED3OOO, MEDSEEK, Passport Health, Virtelligence, and Vocera.
- HIStalk sponsors included on Deloitte’s 2012 Technology Fast 500 ranking include Etransmedia Technology, Greenway Medical, MModal, MedAssets, NexJ Systems, and Vocera.
- Sandlot Solutions unveils the final results of eHealth Initiative’s 2012 Annual Survey of HIE Initiatives.
EPtalk by Dr. Jayne
The American Academy of Family Physicians releases a summary of the 2013 Medicare Physician Fee Schedule. Increases will only occur if Congress takes its annual action to block the reduction that is scheduled for January 1.
AAFP also publishes (subscription only) its 2012 EHR User Satisfaction Survey. Of 3,088 viable responses (as in previous years, several hundred responses were excluded because respondents said they did not use EHR or didn’t identify their systems) 31 vendors account for 92 percent of the systems. The highest counts (over 200 responses) were reported with Allscripts, Centricity, eClinicalWorks, Epic, and NextGen. As someone who has been documenting with EHRs for more than a decade, I find some of their survey questions suspect. For example, “This EHR helps me see more patients per day (or go home earlier) than I could with paper charts.” They certainly didn’t control for the dramatic increase in federal, regulatory, and payer scut work that has added to the bottom line of my work hours. Even if I was on paper, I’d be seeing fewer patients and going home later just for that reason.
The authors recognize that “practice size is independently related to satisfaction,” noting that except for a few systems, the majority of “large practice” vendors fall towards the bottom and “small practice” vendors hit near the top of satisfaction scores. The cutoff for vendor inclusion was 13 responses, so there is question on whether they are statistically significant. Some of the highest ranking systems are relatively untenable in enterprise environments, so I feel for administrators whose physicians will be marching into the office with the article in hand, demanding that Cerner be de-installed in favor of Praxis, SOAPware, or my favorite: Point and Click EHR.
Another doomsday prediction finds that we’ll need 52,000 more family physicians by the year 2025. I can almost guarantee that if you figure out how to pay them what a cardiologist makes, you’ll get them.
A good friend sent me a link to the “Jane and the Doctor” YouTube video. It’s an oldie but a goodie if you haven’t seen it. For those of you in the implementation trenches, know that you are not alone and there are many others of us who hear the same tired complaining from physicians all day long.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.














































































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…