HIStalk Interviews Don Menendez, President, White Plume Technologies
Don Menendez is president of White Plume Technologies of Birmingham, AL.

Tell me about yourself and the company.
I began my career with IBM. I’ve been in software for a long time. I got into healthcare in the late 1980s. I joined a company that had a billing operation, a Unix-based PM system, and an RCM element. The real interesting thing was that we had a shared resource, a large IBM mainframe that we were selling time on. Clients didn’t incur technological or cost risk — they paid on a monthly basis. We didn’t even know it, but we had an ASP before we knew what it was.
That’s how I got to the healthcare side of it. We sold that company to a publicly-held company and then I was looking for a problem to solve. I believe software should solve real problems in a simple way.
I looked at two things. There were two big gaps in the workflow in the physician offices that I saw. One was, back in 1999, clearly the EMR gap. I felt from a timing perspective and the amount of disruption that it would cause for physicians the timing didn’t make sense at all.
There was another one that was kind of interesting. It was what we ultimately got into. It was the automating of the front end of a revenue cycle management process.
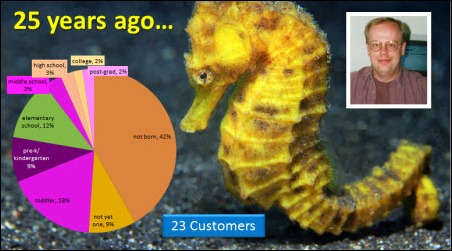
It had been the same for quarter of a century. I’d always known that the first time you automate a manual repetitive, complex, confusing process, that’s when you get to ring the bell financially for your costumers, as opposed to what version 10.1 does for him. That was what this area was. A lot had been done on the back end, but very little on the front end. We felt that if we could push the process use technologies and know-how at the front end without negatively impacting the doctor, we had a real winning solution for him.
Why would practices that already have a PM/EMR system need your products?
It’s really interesting because probably in the last 18 months, the great majority of our new clients are exactly that – people who have an EMR already installed and a PM system.
I think what happens is this. We approach a number of these practices when they’re in an EMR evaluation stage. Many of them feel like they’re going to be able to achieve the results that are provided by the kind of solutions that we provide once the EMR is implemented. What a lot of them seemed to find out was that for any number of reasons, they’re all different. The EMR solution is working well, but they’re not satisfied with the results they were able to get as it related to the automated charge capture and coding process.
Sometimes these physicians find the charge capture process too time-consuming and they won’t do it, or it just doesn’t work for them. Other times it doesn’t match the workflow within the practice of how to do what we call post-encounter coding, taking that encounter and adding all the additional things to it necessary for it to get paid correctly. It’s not all done by the physician, and so there are some real workflow issues.
Other times, what ends up happening is they come to us because they’ve figured out that to solve this problem, they’ve had to hire additional administrative people just to do additional work to get the charges in correctly now because they’re starting with physicians than a different manner they started before.
While they took a step forward in the clinical process, it seems like they either made no progress on the RCM side, or worse yet, they took a step backwards. It’s been really interesting that most of our new business is coming from those folks. I would not have predicted that, to be honest, three or four or five years ago, but that’s really what happened.
Do you think it’s a surprise to physicians that when they finally get a PM or an EMR system, much of the benefit accrues to someone else?
My personal opinion is it’s all across the board. For some of them, they predicted that forever. They were very skeptical in the beginning and it was borne out. For others, they were skeptical and it’s borne out differently. They’ve really gotten some value out of it.
In our particular area, the niche that we serve, and what we’re trying to accomplish — quite frankly, the functionality that we provide is an afterthought for both the physician practice and the vendors that are trying to sell the EMR product. Automated charge capture and coding is an afterthought. Many times is an afterthought in the design process, during the sales process, and during the implementation process.
For what we do, they really haven’t thought much about it during the evaluation and implementation process. But when they get down to the point where they’ve rationalized all that technology and are starting to move forward, we find the administrative people say, “We’ve taken a step backwards” or “We made no progress on this at all, and we didn’t realize that there were something out there that could solve some of these problems.”
Describe how your system works differently from the PM and EMR.
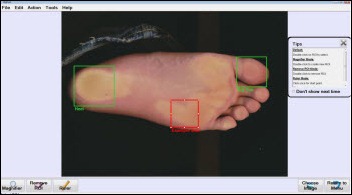
Our whole approach was that you can’t slow the physician down for an administrative task or process. It just didn’t make sense. It was counterintuitive to do that. Everything that we’ve done has been designed around that. The part of the process that starts with the physician needs to help them with their productivity, or certainly not slow them down.
This is an odd thing. It sounds counterintuitive, but when we started this business 13 years ago, the great majority of physicians out there — I’ll bet 90 to 95 percent of physicians — were marking encounters on a paper encounter form. They would spend somewhere between three to 10 seconds with that form. That would be enough information to start the process so they can get reimbursed with that encounter. That’s a pretty high standard against which to take an electronic system and try to make that work.
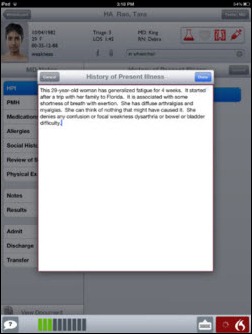
We’ve focused on the charge capture device, whatever that is, to be productive for the physicians. We’re agnostic towards that. We don’t care. We’ve always had a real open attitude. The best way to get a charge into the system is whichever way is the best for the individual doctor. It could be an iPad. It could be another tablet device. It could be an iPhone, an Android, or other mobile devices. It could be EMRs, keyboards, and lab systems. It could be paper. Regardless of the tool used to capture that data, it should complement and leverage the process and the workflow of the practice. That’s what’s important.
Like most software companies, we learn on the back of our customers. We’ve been doing this same very focused process for 13 years. They’ve taught us a bunch about how it works. It’s not slowing the physician down. It’s not pushing administrative tasks to the physician. It’s leveraging productivity and accuracy on the front end of the process as opposed to the back end of the process where most of that’s been.
How does it integrate with the PM/EMR?
We originally integrated with PM systems because EMR adaption was so minimal that it just wasn’t an issue for most of our clients. We probably have upwards of 30+ different interfaces that have been in place for quite some time now. Over the last three or four or five years, we have been doing many more EMR interfaces, so that once the doctor is finished with the patient encounter from an EMR basis, they will send us the important bits of data that we need for the charge encounter.We’ll run it through our automated workflow and coding system and then electronically send it to the PM system as if it had been keyed in by the PM system itself.
Obviously, there’s a real benefit there when you got an environment where there’s one PM system and a different vendor for the EMR system. We provide a nice middleware bridge for them just to pass the data, but when we pass it, we clean it up.
I notice you just brought AccelaMOBILE for mobile capture of physician hospital charges. Explain how physicians bill for the hospital services they provide.
It’s really interesting. In the ambulatory setting when they’re in clinic, the administrative personnel will put all sorts of procedures and processes in place around the physician to make sure they get the information they need to get an encounter paid. But when those physicians go out to the hospital, they’re on their own.
It’s almost like the Wild West out there. It’s every way possible you could think about it. Some are doing along 3×5 card. Some of them get a rounding list printed off from their PM system and they jot those things down. I’ve seen physicians jot it down on their scrubs. They run into a colleague in the hall and they do a consult that nobody knows about and they forget do it. They go to the football game or the music recital right from the hospital and they lose their charges.
One of the big problems with mobile charge capture is just getting decent good data back to the billing staff so they can clean it up. That’s the real allure of mobile charge capture and the concept of AccelaMOBILE. It’s always been about getting the form factor and a technology used by the physicians.
We looked at doing this 10 or 12 years ago, but the technology just wasn’t there. But now, with physicians being 10 years younger than they were, they’re accustomed to the form factors of smartphones and iPads and those kinds of things. We can now at least solve that first part of the problem — we can get the data back to their billing office in a legible manner that’s complete about what they were doing in the hospital. That’s what the real excitement of the mobile product is.
The second piece is that once you get the data in, it does need to be cleaned up and appropriately done so that you get paid for it. The mobile product is the front end for remote charge entry by the physician. That is complimented by our back-end suites of products that do the workflow and the coding on it.
For some companies, it’s a whole different ballgame to develop their first mobile application and do it right. What did you learned in bringing out AccelaMOBILE and seeing how physicians are using it?
I’ll sound like a broken record, but we’re dealing with high-knowledge professionals that are extremely busy. They were trained to see one, do one, and teach one. That’s the way we try to do the user interface. It has to be simple, it has to be quick, it has to have very few clicks, it has to provide them shortcuts necessary so that they can get into the technology and get out of it very quickly. That’s a continually improving process, and frankly, our physicians are the ones that teach us the most about that. But the simpler the better for them.
How hard is it to make a business case for a practice that may have stretched themselves to buy another new system and now you’re offering them a different one still?
A big issue for everybody is the bandwidth of the practice. Intellectual bandwidth, time to do another project, certainly finance is a commitment, that kind of thing. That is a big issue for us in the marketplace at this juncture, but we try to do things to minimize that. Our whole approach is focused on minimizing that.
We believe that if you’re seriously looking to improve your automated charge capture and coding process on the front end, you can take a look at what’s out there in the marketplace. You can evaluate the systems. You can evaluate what’s available and how it’ll work, probably within a week or two if you could devote a little bit of time to it.
For us, implementations are typically three days. We’re in and we’re out. It’s a pretty quick process, so it’s pretty light as it relates to the staff itself, but the bigger issue is just the idea that you’d even think about looking at something there.
On your website, it says that HITECH has skewed the EMR market and the vendor accountability to customers with what was described as a checkbook and a gun. How do you see the EMR/PM market evolving over the next several years?
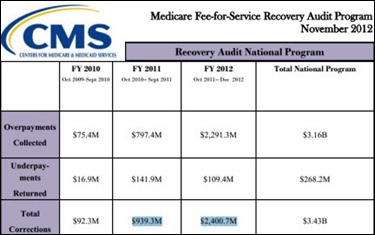
I’m bullish about that, for two reasons, primarily. We believe that once Meaningful Use settles down a bit, the same market forces that have been in place for years will be refocused on, and that’s downward pressure in reimbursement — we don’t see that changing – and increasing complexity and cost associated with physicians figuring out how to get that reimbursement. We expect the focus to shift back to operational efficiency in the ambulatory setting.
I may be wrong about this, but it seems as if none of the current incentive programs are really incenting operating efficiency for the practice. What they’re about is about driving data. Once that moves a bit, I think we’ll play really well, and that as they start to turn towards maximizing efficiency again.
The other piece, the wild card that everybody’s talking about and knows about, is ICD-10. It’s a huge, huge threat to physician productivity and to revenue cycle performance. That’s not about driving data — although for the government it is about driving data — but to practices just trying to see their patients and do what they need to do, it’s a huge threat to both those areas. That’s where we focus. We hope that it doesn’t get pushed out. It’s a distraction. We understand the importance long term about it, but we think it’s an unfortunate distraction.
We think that once all that quiets down a bit, it will return to some of the basic issues. Frankly, they’re going to be harder. The economics are going to be different in an acute setting than it is the ambulatory. The hospitals are buying up all these practices. As they move out of that acquisitive mode and they start to try to rationalize their acquisitions, I think there’s going to be more focus on maximizing operational efficiencies. They’re going to look for help in the ambulatory setting with revenue cycle systems and that kind of thing without having staffs.
Any concluding thoughts?
I’m grateful for the great team we have here. I started this because I thought that business is a part of the fabric of life. You can do both. You can have a great team, you can compete effectively, you can be profitable, but you can have a place where people can live balanced work lives. I’ve been fortunate that the folks that decided to work here really care about our customers and find ways to solve problems. I’m grateful for that.
I’m grateful for that and I’m grateful for our customers. We have learned so much from them about the challenges that they face and how to make our product a better result of that. Software companies learn on the backs of their customers. I’ve been in the software business since I got out of college and they never get credit for teaching us, but they do teach us. I’m grateful for that.
This is a great time to be in the business. I don’t know what’s going to happen, but as long as physicians wake in the morning, see patients, and hope to get paid for what they do, they’re going to need to get encounter data to the payer and we seem to know how to do that pretty well. There are lots of different ways of making that happen, so we think that means that there’s going to be an opportunity for us. Even as a small player, we’re bullish on what the next three to five years might look like for us.



























































Move your quotes to where they should be and it's no longer politics-in-the-blog, but instead a fact that's true at…