Robert H. “Bob” Lorsch is president, CEO, and chairman of MMRGlobal of Los Angeles, CA.

Tell me about yourself and the company.
I sold my business in 1998 for several hundred million dollars to AT&T. After the company was sold, I have spent many years focused on philanthropic activities – California Science Center, Cedars-Sinai Medical Center, St. John’s Hospital, and a variety of other organizations.
In 2000, I myself was diagnosed with a rare form of thyroid cancer. Despite the fact that I was extremely connected to doctors, hospitals — both as someone who’s been in the Los Angeles community for many, many years and as somebody who had supported these organizations — I was personally subjected to the task of selecting the guy that was going to be the surgeon who was going to go into my neck and deal with my cancer.
In the course of that, I quickly realized that having the disease was only one aspect of what I had to deal with. But the real aspect of what I had to deal with was the emotional trauma of what goes with being diagnosed with the disease and the challenges that are placed in front of a patient in terms of collecting and getting information so they can get competent physicians to give them knowledgeable and informed information to deal with their situation.
I must tell you that I’m not sure that dealing with the cancer — which was a six-hour operation where I was completely out of it — was probably easier in the long run than the months of agony and emotional torture of trying to figure out if I picked the right doctor, how was I going to get copies of my medical records, what the diseases meant, etc.
In 2005, someone showed up at my house and said, “I think you should go in the electronic medical records business” because Bush had signed an executive order in 2004 suggesting — or ordering — that everybody in America have an electronic health record within 10 years. I took a look at that and I said, “You know, interesting concept. I’m not interested, though, in competing with GE, Cerner, Allscripts, McKesson, and all the giant companies in the industry.”
But nobody had focused on the personal health records side of the house. I decided that that would be something I was interested in and we formed MyMedicalRecords.
Everybody assumed that that would be a really hot sector because people were Googling medical issues, symptoms, and drug side effects, yet for the most part personal health records didn’t do very well. Google shut theirs down, presumably because patients don’t really want to enter that information themselves manually. How have you found that to be with your personal health record?
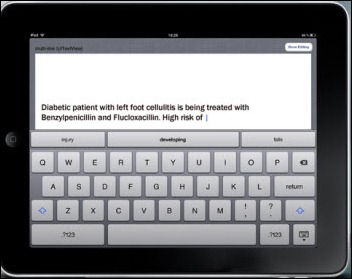
Our personal health record doesn’t really require the patient to enter anything manually. We have a completely different perspective on what goes into a personal health record and the ease of utilizing a personal health record.
We give a patient what we call a lifeline number, which is a 10-digit telephone number. We basically have a personal health record that is completely connected, completely interoperable with not only any hospital, physician, or medical professional in the United States, but any hospital, physician, or medical professional in the world based, on the backbone of the telecommunication system.
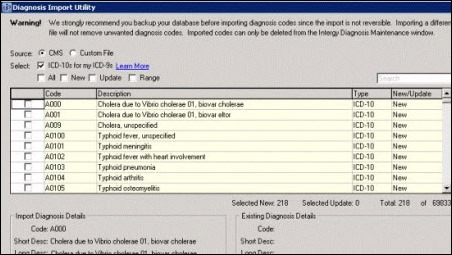
If you go to a doctor, you have a right to get your medical records in the United States. All you have to do is tell them how you want them. You give him or her your lifeline telephone number, and when you leave the office, they fax your record or e-mail the record to you so you can upload the record and it goes right into your account.
As a patient, when I look in my account, I’m seeing medical records from my physician. I’m seeing medical records from Cedars-Sinai. I’m seeing medical records from St. John’s. I’m seeing medical records from Long Beach Memorial. I’m seeing medical records from private practices. I’m seeing medical records from my orthopedic guys. I’m seeing medical records from my father. All consolidated into one place that requires me to actually input nothing but look at the document and select the file folder I want to insert it into.
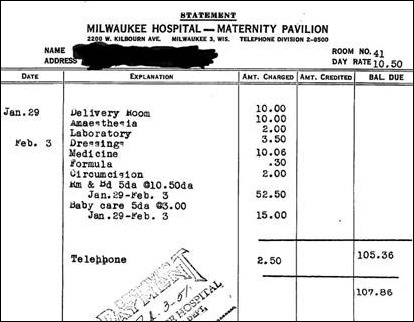
It doesn’t require somebody to sit down and start typing in stats and results and information that in all likelihood will be plagued with typographic errors, wrong and not reliable. When somebody goes into my emergency view, they see my most recent laboratory tests on Cedars-Sinai or Quest lab forms with the phone number, the physician, and the lab that ran the tests. Exactly as they would see it in their office, regardless of where it was originated.
That’s a pretty fascinating approach. Other organizations advocated that health records be exchanged as PDFs, but nobody really ever bought into that concept too much. By doing that, you eliminate the concerns about what data you can accept and the standard interchange formats and all that. You just take everything that looks like a fax or an e-mail and it’s just stored in that exact form. Is that correct?
Part of that’s correct. We also have in the site a patient history. Assuming the patient actually wants to go in and enter data, there’s a form with simple drop-downs where they can say, “I want to input my maternal grandparent’s health history.” You just hit the button that says “grandparents.” It drops down and says is it a condition, an allergy, or a surgery, and gives them some categories. You click on that, write what it is, write the doctor and any information that you want, and save it. Then you can go in and put in your mother, your father, yourself, or your children.
Basically what’s happening is you are building through data entry your personal health record, but all you’re really building is that form that you’re going to fill out in the doctor’s office anyway. When you go to the doctor, you hit a button that says “print my record.” You just bring it in and pretty much everything you’re going to need for that form is with you on the spot and can go right into the doctor’s file. If it’s a medical record or chart note or handwritten note, or in my case, my eyeglass prescription …
Each account works for 10 family members. In my case, I have my son, my father – may he rest in peace – my dog, my wife. Everybody’s in this kind of system. Depending on the emergency password that a physician or a paramedic or emergency room representative would put in there, it brings up the medical records, photo, insurance information, and prescription and labs for that individual. From any Internet-connected computer anywhere in the world, no questions asked for the quality of the form, because the person looking at it can basically reach out to the lab and confirm it’s accurate.
One of the problems of personal health record is you may get a patient that’s embarrassed about something. They may kind of redact something from data. We do not give the patient the ability to do that, because there is no data in the actual record. There is data in the health history.
I believe I understand right that it’s priced for families at somewhere around $100 per family per year.
There are multiple pricing programs. Direct online, somebody can go and pay $9.95 a month or $99.95 a year and set up and have their account. They can also pay for what we call personal touch — $80 more — and we find a nurse practitioner to go to collect forms for them. We contact all the physicians from throughout their life and we update the medical records in the account for them.
And then there’s the employer programs, where an employer with 1,000 employees can pay us less then $2 a month per employee and every employee in a company would have access to an account. And then there are associations, much larger groups, where they would pay an annual fee for every member in the association and it becomes an affinity benefit, much like a LifeLock or other similar service — whether it be lost baggage, a personal health record, insurance services — that are embedded into the benefits of that organization.
I don’t want you to tell me anything that’s proprietary, but can you give me a feel for how many active users the service has?
We define users in two different ways. We have members and we have users. For example, if you’re part of a company that has 5,000 employees, every one of those employees is a member. The actual user, depending on the type of company, can range anywhere from 5 percent to as much as 28 percent, and so we define members from users separately.
At last count, we had I think 750,000 members, although that does fluctuate up and down. We had from those members approximately 8 or 9 percent what I would call heavy, heavy users. But it doesn’t really matter, because if you work for that company, you have the ability to go in and set up your account at any time.
You might take some medications. You might have something going on in your life. But you take somebody who’s 30 years old. They get a personal health record, they don’t even think about it. They’re not as aware of it. Until one day they go to the doctor and he says, “You know, you need to have appendicitis operation or your cholesterol is too high or for some reason we’ve got a little spot that we want to deal with or some type of MRI.” All of sudden then, the person is, “Oh my gosh, I’d better start collecting my information and building my medical record.” We find that as people have their record over time, more and more people will come in and start adding things into the record.
The other thing that we find is attrition. Since we’ve been in business — which is almost eight years now and with the product out there a little more than six — attrition is less than 2 percent. The real-world attrition, we think, is less than 1 percent. The difference is that is people who have passed away or for whatever reason aren’t getting the benefit any more. It’s not really the attrition in the account, because once somebody gets their information in the account, they don’t want to give up the account.
In the account are 16 file folders. You have complete control over what those file folders are called. Four of those file folders are actually password protected. You can call them an e-safe deposit box. You can call them a real estate file. You can call them advance directives. If somebody gets into your medical record on emergency basis, they won’t see those files, because they are password protected through the administrative side of the site.
I could be anywhere in the world and I would have passport, driver’s license, advance directives, emergency documentation, inventories of all the furniture, fixtures, and materials in my home, etc. It’s not only a personal health record, but it’s an emergency disaster preparedness medical record. You’re in a community, a tornado comes in, you’re wiped out, you need your medical records. You also need your driver’s license, your banking information, your advance directives, the articles that were in your home, your insurance policies. They are all in password-protected files that are embedded into the account.
The other reason we do the password-protected files is when a child becomes 16 years old, they are entitled to have privacy to their personal health information. This way, a family can have a MyMedicalRecords account and they can allow a one file folder to be assigned to each of the teenage members of the family so that the parents can’t have access to what’s in that account. If you have a daughter that, for example, decides they want to take birth control pills, their medical record could be separate from the family’s medical record and password protected so the parents cannot get into that account.
I want to ask you a question about patent licensing. You’ve made some statements that licensing is the future of the company’s growth and a lot of the press releases involve that. Is it fair to say that a long term plan is that the licensing fees will be the majority of the company’s income?
If I may push back a little bit, I’m not sure that I’ve said licensing is the future of the company anywhere. I don’t think that’s actually a quote that I made. What I have said is that as a result of Meaningful Use Stage 2, hospitals, healthcare professionals are obligated if they sign on the dotted line and tell the federal government that they are requesting reimbursement under Meaningful Use Stage 2, there are certain things they have to attest to. One of them is to provide a certain percentage to their audience with a personal health record. Under Stage 3, it will be more severe, because under Stage 2, they have more time. They’re talking about bringing that down to less than a day in Stage 3. Those records are required.
If somebody complies with that Stage 2 Meaningful Use, we believe that they will infringe on one of seven patents that we have issued in the US Patent Office an additional patents that we have issued in 12 additional countries around the world. What we have done is we’ve gone to the hospitals, providers, vendors, laboratories, and we’ve said, “Look, if you’re going to comply with Stage 2 Meaningful Use or you’re going to offer products and services that enable healthcare professionals to meet Stage 2 Meaningful Use, they’re probably going to infringe on one of our patents.”
We’re suggesting that they license those patents at very reasonable license fees, such that whatever they decide to do to comply with Stage 2, Stage 3 Meaningful Use, they have a license – a safe harbor — that they’re grandfathered in, where they never have to be concerned about infringement on any of our patents or other intellectual property. If those same hospitals say, “Are there any other ways to address this?” they could also use our products — our MyMedicalRecords products, our professional products — which are embedded with licenses for the technology.
What we’re essentially saying is if a hospital wants to comply with Stage 2 Meaningful Use … and I want to be very, very clear, I’m not saying they’re definitely infringing, but we believe with nearly 400 claims, that there is a high degree of likelihood that they will infringe on our patents and other intellectual property — we will, as cooperative a way possible, reach out to them to offer them licenses, the ability to utilize their product, prior to bringing any form of legal action if we believe the infringement is direct and on point.
Have you ever taken someone to court for infringement?
We currently have four matters that are of interest. Approximately two or three weeks ago, we filed a lawsuit against Walgreens. Last week, we filed a lawsuit against WebMD. We currently have identified in Australia that the Australian government actually built a $1.1 billion personal health record system that blatantly, we believe – and I would appreciate it if you would always qualify it with “we believe” – infringes on our patents almost totally. The irony of the whole thing is that the government actually appears – and I want to say “appears” – to have used our attorneys who got us the patents in Australia to review and give them an opinion on the intellectual property.
We have found the same thing in Singapore, where the health department in Singapore and other companies — including a very, very large company out of China — are infringing on our patents there.
We have begun the process of pursuing Australia. We would hope to settle it very, very quickly, because they have a billion-dollar system that is basically given away to everybody who lives in Australia, which completely, completely destroys the ability for us to sell our product. We would hope that they will be objective in entering to some type of licensing agreement with us. Our patents go far back before they ever actually looked at the system that they built subsequent to the issuance of the patents, which we believe they were aware of.
I forgot to ask that earlier. What years were your patents granted?
The patents have been granted throughout the last seven years. I mean, originally they were filed … I think originally the first filings were in 2005. The US patents mostly were issued at the very, very end of 2011 and throughout 2012. We continue to have numerous applications on file, both pending applications and continuation applications on existing patents.
Your patents were filed in 2011. What was new in 2011 in your patents that hadn’t already been marketed by someone prior to that?
It has to do with what we originally invented in 2005. The patent is like three legs of a stool. You plant the first leg and the stool is going to be a bit wobbly. Then you plant the second leg and the stool is going to be solid. Then you plant the third leg and the fourth leg and you build on intellectual property. The original inventions were true inventions at the time they were filed in the patent office. They’re all based on the original art. Then over time, you amend those applications to bring in different features and functionality that rely upon the original prior art.
But the original prior art when we file these patents or the amendments to these patents or additional patents or continuation patents on, the Patent Office is very, very thorough. I mean, very, very thorough. It took us close to seven years to issue the first patent. It took us, I think, five or six years to issue the first patent internationally. It took almost eight years to issue patents in Mexico. It’s not a simple process. They look at everything. It costs this company millions of dollars in fees, expenses, and attorneys on a global basis in order to prosecute this portfolio.
Most patents are written to be as broad as the patent office will accept. Can you just describe in general what the patents cover? Maybe the top one or two that are in question now with other people infringing.
There is a valuation that was done which I can send you the link to. It was actually covered in a news release by the company when it came out about a month, a month and half ago. That valuation identifies every one of the patents around the world by its name, description, and number. I don’t want to answer a question that really has the potential of narrowing the scope just by the fact that I can’t properly answer it in an article like this. What I would do is I would refer people to that valuation summary and they would be able to go to the patent office and look up everything.
There’s claims that deal with how the patients get personal health records. There’s claims that deal with telemedicine. There’s a broad spectrum of claims. Like I said close, to 400 in stage, with more patents and additional claims pending and a lot of claims around the world. It wouldn’t be fair to you, me, or the reader to just say, “The basics of it is this.”
They are a method and system for providing personal health records, electronic health records, and other forms of electronic documents. They run the gamut of e-safe deposit box, which could mean personal information like we discussed with advance directives and maybe a copy of your passport all the way to your medical records.
Some of the recipients of the potential infringement letters have been hospitals, most of which are non-profit. I don’t want to ask you a proprietary question, but when you say the fees are reasonable, what kind of terms would you offer them to license?
Every one of the agreements and licenses that we’ve entered into is confidential. If you look at me or you Google me, I spent the last 13-14 years of my life dedicating it to giving away money to charity. Prior to that, I probably have raised more money for organizations using what was called cause-related marketing, where a portion of a dollar that a company like Procter & Gamble would get would go to Special Olympics or the Heart Association or D.A.R.E. America. So when it comes to non-profit charity and giving, it’s in my DNA.
When I say reasonable, I mean in a way that protects the hospital, gives them a benefit so that they can provide a broader service to their patients. It’s not the kind of dollars that you’re looking at from all these lawsuits with Samsung and BlackBerry and Apple. It’s not that kind of a thing.
We look for a win-win situation with the hospital. The best way I can explain it is our primary business is personal health records. A lot of people have tried to paint the letters we’ve sent to the hospital as if we’re patent trolling. A troll is somebody who has rights to a patent, but basically goes around suing people and demanding royalties. A troll is not the original inventor of the patents, of which I am on every patent that’s been filed anywhere in the world.
We invented those patents so that we would have the opportunity to go into the market and compete and create a barrier to entry for our competition. By ignoring our rights under those patents, we are essentially being denied the ability to compete in that marketplace, because other people will just go in and sell their product at the expense of infringing on our patents.
What’s fair and reasonable in our mind is something analogous to the amount of money that we would have made had we were providing those products and services. But if somebody is going to say we’re going to preclude you from providing those products and services, then they should pay us something reasonable for infringing on our intellectual property.
In our case, we don’t care if somebody licenses or somebody buys. They win and we win either way. The objective here is to not do something that makes it impossible to make a deal, but also do something that is fair to our shareholders in the sense that we’re not denied access to the marketplace just because somebody said, “The heck with them. We don’t care about their patents,” which is what is happening in Australia. I mean the Australian government in a macro example — macro being huge, but one country — they basically said, “We’re going to make a personal health record. We’re going to give it away to 20 million people free and we’re going to infringe on IP and we don’t care.”
I had a meeting with a group of Congressmen last week in Washington, DC. Ironically, we focused on stimulus, and some of the things were covered in the Page 1 article in The New York Times. These Congressional representatives who are on the oversight committees have said that intellectual property –the right to own property, the right to own a home, the right to own what you create, eat what you sow — is a fundamental right of every American, and it’s probably a fundamental right of everybody wherever they are anywhere in the world.
These are rights that we built products for, we created things for. When somebody takes away your right to compete in the open marketplace, they pay a royalty or a license fee. In those rare cases where you unfortunately have to go to litigation, maybe they’ll pay more. But the objective here is to create reasonable relationships with hospitals.
I have said to our shareholders, there’s 5,000 hospitals out there. It doesn’t take a lot to figure if every hospital gave you some reasonable amount of money for every 250 beds, the hospital would win based on the quality of our product and we would win for our shareholders.
There was a rumor that there was some interest by the National Coordinator or some part of HHS about what was going on with the patents and the letters that were being received by hospitals, and possibly by somebody in California, maybe the Attorney General, as well. Has there been any official interest or discussion about what you’re doing from any government or oversight-type body?
When we originally sent out the letters, some of the hospitals apparently forwarded them to the California Hospital Association and the AMA. I received a copy of a letter that was sent by the California Hospital Association legal counsel Jana Du Bois to every hospital general counsel saying, “If you get a letter from a company called MyMedicalRecords, we think they’re some kind of patent troll. Let us know.”
When I got a copy of that, we contacted her, and we explained to her that, “Hey, it’s our primary business. We invented it. We did not buy these patents. We are not trolling with these patents, and by the way, we are very, very anxious to enter into reasonable business relationships with the hospitals to license the patents or utilize our products and services.”
She turned around and basically sent out what I would – I’m not going to say it was an apology letter — but she definitely sent a letter out to everybody to set the record straight. To the point that I just found out last week in one state on the East Coast, meeting with their association, actually discussing the possibility of saying, any hospitals in the state, we will negotiate through the association one license agreement so that the hospitals can get the benefit of the lowest possible rate, and as long as the hospital is a member of that association, they would get the license agreement.
In addition to that, we — meaning MMR — would take 30 percent of those license fees, put them into a non-profit managed by that association to provide healthcare and philanthropic services to underprivileged in their communities through their hospital network. So in essence, we would say, State XYZ is kind of like a safe harbor for, I think it’s 10 months. We would negotiate a license agreement with that association. The license agreement would be based on the beds in the hospital. They would offer it to everybody in that state.
If they accepted it, they got that rate. We would take 30 percent of the money, give it back to the community to provide healthcare and other services to the community through those hospitals. If the hospital did not sign on, then we would see what happens after that period of time. That is as recently as last week. It was very well received. We are already in the process of signing agreements to facilitate those conversations.
The associations are very aware. The associations hopefully will understand that we’re trying to be reasonable about the whole thing. As for the AMA, I know they’re aware of it. We’ve not communicated with them.
As to the National Coordinator, my days with the National Coordinator go back to Dr. Brailer, when Mike Leavitt was Secretary of Health. Mike Leavitt knew about MyMedicalRecords and our intellectual property in the early, early days. Dr. Brailer knew about MMR and our IP in the early, early days. The Small Business Administration acknowledged what we were doing after Katrina, because we had the ability to not only provision personal health records, but emergency safe deposit boxes for victims of natural disasters – they presented us an award. Subsequently, I meet with Dr. Blumenthal and William Yu, when he was in the office, went through the products, service, patents, the intellectual property. There could be no surprises to anybody about what we have been doing.
I think I read that you’re sending – maybe it’s not the right figure — 250 letters a week. I’m just curious how much response you’re getting from those letters or what hospitals are doing when they receive those letters?
We’ve sent out somewhere between 600 and 750 letters. Many of them respond. Some of them don’t respond. When they don’t respond, we reach out and try to communicate with them.
There are maybe additional letters, but at this particular point in time, we’ve had a lot of success with everything from the association I described to numerous hospitals in California that have opened the door for meaningful negotiations. If somebody opens the door for meaningful negotiations, we’re basically going to take the time that’s necessary to make them comfortable that they’re making the right decision.
Meaningful Use Stage 2 really starts in February 2014, I think. And so, if the hospital wants to understand this, vet the product, vet the service to understand the IP, we’re anxious to work with them in a businesslike manner.
Any final thoughts?
We’re looking forward to HIMSS. There are a lot of people that have gotten letters from us. We’re looking forward to more patents being issued. There are a lot of people that have contacted us and arranged to meet with us at HIMSS to discuss a variety of business opportunities from strategic partners, licensing. We’re going to be previewing wellness applications connected to our personal health records. We’re going to be focused on integrating our personal health record with the output from all the apps that are coming in on iPhones and Android phones.
We’re looking forward to meeting people in the booth who may have the wrong perception of the company. If the perception they have is it’s some guy sending out letters trying to get royalties who is not entitled to them, we’re not those people. There may be some of those people out there. We’re not those people.
We have a real product that we invented that we would prefer to sell people. But if people are not going to buy it and they’re just going to work around it or they’re going to ignore us … the most reasonable thing to do is to license, because that way everybody wins. Should they decide that, you know, it’s really not such a dumb idea to attach a 10-digit telephone number to every one of our patients’ personal health records so that they can go anywhere in the world, and if they’re on vacation in Israel – where, by the way, we own the patents — they can literally get a lab test, have it put in their account, and seen by their physician at New York Pres in three minutes.
I’m a big believer in supporting hospitals so that if, God forbid, I go into the emergency room and I need something, the little green light goes on and says, “He’s a good guy." But hundreds and millions of dollars have recently been spent in this community by Cedars-Sinai Medical Center and UCLA. They both have Epic systems. They can’t talk to each other. Here I’ve got a health savings plan. I’m in the emergency room at Cedars-Sinai, but next time because I’m closer to UCLA or the Cedars emergency room is full, all the tests that I had at Cedars now have to be redone at UCLA. Why?
Kaiser is a classic example. The rumor is more than $6 billion has been spent on EMR and PHR. Right now, I’m not a Kaiser member. If I get sick anywhere and I need my medical records, yeah, I have some kind of a patient view. But that emergency physician in Sheboygan, Wisconsin or in Deer Valley, Utah, where I just came off at a ski slope with a pain in my arm or my chest or broken bone — they can’t get that data. They’ve got to completely rework me up before I go into surgery. If I’m unconscious, these people don’t know today that I’m a thyroid patient. I don’t have a thyroid. I have to take certain medications. If I’m unconscious, I can’t tell them that.
If you start asking around about how much money has been spent on a state-by-state basis trying to create a regional health information system — I’m going to be kind — It’s probably $20 to $50 million a year, and I don’t think you can find a working model. If you do find a working model, I don’t think you can find a handful of hospitals that talk to it, because they’ve all got their own EMRs. There’s no interoperability, despite the fact that this whole effort from Bush was designed to empower the patient and create interoperability. So basically we’re at $11 billion and counting — maybe 12 now, I don’t even know, it goes so fast — and the original selling proposition of why we needed this has not been met.

























































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…