News 2/13/13
Top News
Greenway announces Q2 results: revenue up 12 percent, EPS $0.00, missing both revenue and earnings estimates substantially, guiding fiscal year earnings to the low end of the range on lower revenue. Shares were down eight percent in Tuesday’s after-hours trading. From the earnings call:
- The company is moving rapidly to a recurring revenue model, with revenue recognition changes hurting short-term results
- 750 providers were added in the quarter, up 30 percent year over year
- Training and consulting revenue dropped 35 percent because large accounts pushed training out into January
- The company’s new RCM platform is in its early stages, but has over 300 customers
Reader Comments
![]() From Judy: “Re: our HIMSS promo. I thought about you. We’ve secured 25 New Orleans merchants to offer discounts to HIMSS attendees wearing our Iatric Systems branded slap bands. Merchants range from restaurants to spas to jewelry to clothing and to two stores specializing in shoes and boots. You can wine, dine, shop, tour, and spa in between all the HIMSS activities.” Judy had me at shoes and discount, but wine and spa, too? Look for the bands in the LeSack hotel drop Sunday night or at the Iatric booth.
From Judy: “Re: our HIMSS promo. I thought about you. We’ve secured 25 New Orleans merchants to offer discounts to HIMSS attendees wearing our Iatric Systems branded slap bands. Merchants range from restaurants to spas to jewelry to clothing and to two stores specializing in shoes and boots. You can wine, dine, shop, tour, and spa in between all the HIMSS activities.” Judy had me at shoes and discount, but wine and spa, too? Look for the bands in the LeSack hotel drop Sunday night or at the Iatric booth.
![]() From Alberta Gator: “Re: HIStalkapalooza. I am assuming I did not make the cut for HIStalkapalooza since I didn’t get an invite. It’s OK. I’ll still bring sexy shoes in your honor.” Don’t fear: the invites have not yet been sent even though the registration has closed! The official HIStalkapalooza invitations will be e-mailed to several hundred of our BFFs around February 18. And I can’t wait to see all the sexy shoes. If you didn’t sign up, sorry, but we’re full.
From Alberta Gator: “Re: HIStalkapalooza. I am assuming I did not make the cut for HIStalkapalooza since I didn’t get an invite. It’s OK. I’ll still bring sexy shoes in your honor.” Don’t fear: the invites have not yet been sent even though the registration has closed! The official HIStalkapalooza invitations will be e-mailed to several hundred of our BFFs around February 18. And I can’t wait to see all the sexy shoes. If you didn’t sign up, sorry, but we’re full.
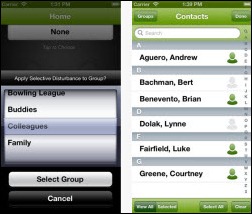
From The PACS Designer: “Re: Selective Disturbance App. Our fellow HIStalker Inga has helped a developer name a new mobile app by calling it ‘Selective Disturbance.’ It will be on TPD’s List of iPhone Apps with the next update.” I asked Inga what this was about and it turns out she helped choose the rather brilliant name attached to the app, which lets you selectively set a “Do Not Disturb” status by groups of individual contacts, so maybe you let your child get through 24×7 but block casual acquaintances during work hours.
From Ralph Samuelson: “Re: Allscripts. I am not sure how it is for everyone, but the company is allowing everyone in my group (programming for one of the legacy products) to stay on until August 1. We have until then to relocate or find another job outside the company. I probably can’t move, but I am grateful I have some time to consider my options.”
From Alert Reader: “Re: revisiting old announcements. How about Deborah Peel saying they would post Form 990 on the Patient Privacy Rights website, which was in HIStalk on January 3, 2011?” I’ve invited her to respond.
From Code Monkey: “Re: old systems vs. new. The experience haven’t changed since the early 2000s. Example: our hospital got reports that several patients weren’t seen within several hours after admission. That’s the responsibility of residents, who are entered as consulting physicians. The chief resident opened 10 tickets with no response from the application team saying that patients were disappearing from our portal lists. We had just applied a McKesson Horizon patch, so we checked the new Perl audit feature, which showed a new routine called ChopConsult, which started with: ‘Temp fix to remove [root@hcilink perl]# cat ChopConsult #Temp fix to remove consulting physicians beyond 8 from ADT.’ If you have more than eight consulting physicians, sorry, you now have zero. I use this as an example that many of these systems are hacked together and stability is an issue, without even looking into the database design. Pay no attention to what’s behind the curtain (or cloud).”
From Smarty Marty: “Re: Aetna. Will brand its Accountable Care Solutions assets (Medicity, iTriage, ActiveHealth, PracticeiQ) under the Healthagen name, possibly to separate these solutions from their core commercial insurance business. I found this when I went looking for the Medicity booth on the HIMSS website and could not find anything. Medicity’s website has brief information about it in the Events section.” Aetna quietly acquired Healthagen, which developed the iTriage consumer health app, in December 2011. Above is what is apparently the placeholder web page for the new Healthagen organization, with the four company names listed at the bottom. The Healthagen HIMSS exhibitor listing has three of the company names, omitting PracticeiQ.
HIStalk Announcements and Requests
![]() I wonder how many other people got this same e-mail from LinkedIn? I felt incredibly special for about 30 seconds until Mr. H told me he got the same notification. I knew it had to be bogus / a marketing ploy / a waste of my time when LinkedIn sent me the same notice for my personal LinkedIn account.
I wonder how many other people got this same e-mail from LinkedIn? I felt incredibly special for about 30 seconds until Mr. H told me he got the same notification. I knew it had to be bogus / a marketing ploy / a waste of my time when LinkedIn sent me the same notice for my personal LinkedIn account.
We acknowledge and appreciate the support of Deloitte, a brand new Platinum sponsor of HIStalk. The company is, of course, a premiere, worldwide professional services firm headquartered right here in the USA (New York) with a strong healthcare IT presence and a list of awards to prove it. Deloitte’s provider practice supports organizations working on tough problems: quality improvement, ICD-10, business intelligence and analytics, system implementation and optimization, disease management, and HIEs. You can keep up with big-picture developments by reading updates from Paul Keckley, PhD, executive director of the Deloitte Center for Health Solutions. A bunch of us who’ve been around awhile know Mitch Morris, MD, who leads the company’s health IT practice, and I’ll be talking to him soon about industry trends. Thanks to Deloitte for supporting HIStalk.
I always hit YouTube to see what I can find out about a new sponsor and my search for Deloitte turned up a winner: a brand new report on the 2013 health outlook.
HIMSS Conference Social Events
Going to HIMSS? We’ll post social events that are (a) interesting, and (b) open to all HIStalk readers who care to attend. Send yours to be listed.
Alego Health will host a cocktail reception on Tuesday, March 5 from 3:00 to 6:00 p.m. at their booth (#141). They’ll have hurricanes, beer, wine, an infused hydration station (what the heck is that? sounds like an IV), and some nice food that includes mini po’ boys.
Acquisitions, Funding, Business, and Stock
Enterprise HIS vendor RazorInsights announces $11 million in Series A funding from Bluff Point Associates. One of its customers was announced in the press release – Alliance HealthCare System (MS). CEO Reed Liggin mentioned the upcoming investment in my February 8 interview.
Teleheath company INRange Systems raises $1.6 million for its remote medication management device that administers single doses of meds to patients and transmits adherence data to physicians and pharmacists.
Employees of the Barcelona, Spain office of Picis (Optum / UnitedHealth Group) say they will go on strike beginning Thursday to protest the amount of severance they’ll receive as the company moves most of their jobs to India. According to the employee spokesperson who contacted us, “First, the UHG negotiators don’t have a firm plan to transition Picis development and support to India and we’ve asked them to let us help sort out how to successfully do it. Second, the compensation package is drastically lower than what we could win in court.” Spain’s legally-mandated employee benefits are extensive, but the employees say most companies that move jobs to India provide more than the minimum separation benefits. UPDATE: the response from Optum: “Picis Spain is engaged in good faith negotiations with employees at its Barcelona office, as it evolves its local workforce to better align with changing customer needs. We don’t anticipate any business disruption and hope this issue can be resolved fairly and quickly.”
Sales
Greater Baltimore Medical (MD) will implement Amcom Software’s Mobile Connect smartphone texting solution with their existing Amcom communications system.
The Michigan Department of Community Health Medical Services Administration awards Cognosante the Medicaid IT Architecture State Self-Assessment contract.
Tanner Health System (GA) selects Besler Consulting to conduct a transfer DRG underpayment recovery audit.
Arnot Ogden Medical Center (NY) will implement Merge Healthcare’s cardiology solution suite to capture, manage, and display multi-modality cardiac images, along with hemodynamics and ECG data.
Southeastern Health (NC) expands its relationship with eClinicalWorks to include the company’s Care Coordination Medical Record.
Dignity Health Medical Foundation (CA) chooses MediRevv for A/R management services.
People
Trinity Health CEO Joseph Swedish is named CEO of WellPoint, the country’s second-largest insurer, replacing former CEO Angela Braly.
Russell Branzell (Colorado Health Medical Group) is named president and CEO of CHIME.
Athenahealth COO Ed Park joins the board of directors of analytics vendor Kyruus.
Vitera Healthcare Solutions hires Kermit Randa (Surgical Information Systems) as EVP of sales and marketing.
TransforMED, the AAFP subsidiary that supports practices transitioning to PCMHs, announces the retirement of president and CEO Terry McGeeney, MD.
MedeAnalytics promotes Steve Lerch to SVP/GM of the provider business unit, Scott Paddock to SVP/GM of the payer business unit, and Sal DeTrane to CFO.
Hello Health names Barry Holleman (Cardinal Health) COO and VP.
Aspen Advisors promotes Jody Cervenak to principal.
CVS Caremark appoints Brian Tilzer (Staples) SVP/chief digital officer.
Health Care DataWorks promotes CFO Jeffrey Wilkins (left) to CEO, replacing founder Herb Smaltz (right), who will continue to serve as board chair.
Announcements and Implementations
Over 60 ACOs from 15 states form the National Association of ACOs, which will focus on helping organizations to increase the quality of care and improve health in their communities.
The Mount Sinai Medical Center (NY) reports that its Epic EMR has resulted in improved quality of care for patients, including a 56 percent reduction in Medicare readmissions and improvements in quality measures such as discharge instructions for patients and antibiotic administration prior to surgery.
The Huntzinger Management Group assists Hanover Hospital (PA) in its successful Stage 1 MU attestation.
API Healthcare introduces its Talent Management Solution to improve employee engagement while addressing the industry challenges of healthcare reform and an aging workforce.
SimplifyMD launches its simpleStart program that will allow practices to move from EHR demo to live clinical use on the same day.
Mobile platform application development provider Kony Solutions announces support for the BlackBerry Z10 and Q10 smartphones.
Stilwell Memorial Hospital (OK) goes live on Medsphere OpenVista.
Government and Politics
The government’s healthcare fraud prevention and enforcement efforts recovered $4.2 billion in FY2012, up from last year’s $4.1 billion. Over the last three years, fraud and abuse investigations recovered $7.90 for every dollar spent.
President Obama re-nominates Marilyn Tavenner as permanent administrator for CMS.
Anybody who follows the VA/DoD EHR saga knows that the story changes weekly, flip-flopping on whether they’ll write new separate systems, write one new system, buy off-the-shelf applications, or just patch together what they have. Sometimes DoD has one story and the VA another, illustrative of just how vast the gulf is that separates their philosophies. Secretary of Defense Leon Panetta spoke of the “one EHR" project in the past tense a week ago, saying definitively that the departments were giving up on that idea in favor of just getting their respective systems to talk to each other. Not so fast, says VA CIO Roger Baker, now clarifying that the integration project is a stopgap toward the original goal that will continue. All I know is that whatever they do will be horrifically expensive and behind schedule, especially on the DoD side that has paid contractors billions to develop AHLTA, and all the conflicting announcements have made me lose interest yet again. The OSEHRA community is talking if you can understand what they’re saying, meaning you’d better speak VA geek talk and appreciate decades-old VistA history, which I do on occasion. Some of those pontificating speculate that DoD will end up buying Epic, looking back to 2011 when five Wisconsin Congressmen (including eventual Republican VP nominee Paul Ryan) lobbied for the home team.
ONC’s Doug Fridsma participates in a Google + Hangout.
Federal Health Architecture releases version 4.0 of its open source Connect HIE-enabling platform. It supports higher message throughput, larger files, newly support server environments, and improved logging.
HIMSS urges HHS to stick to the October 1, 2014 implementation date of ICD-10, saying it will reduce the cost of prior authorization, enable Meaningful use, improve population health, reduce waste, and save money.
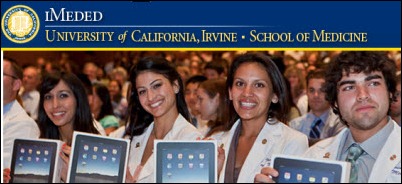
UC Irvine says medical students given free iPads with digital textbooks are scoring 23 percent higher on exams than students in previous classes, also noting that the students have formed their own technology group and developed 19 healthcare-related iPad apps in a 10-day Med App Jam. The iMedEd program was named a 2012-2013 Apple Distinguished Program this week.
Other
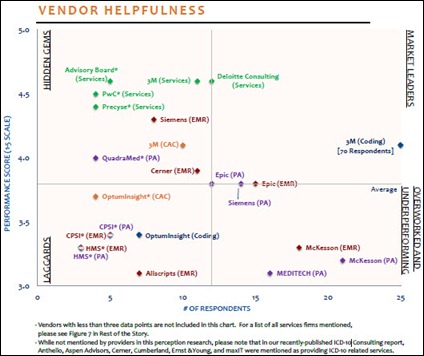
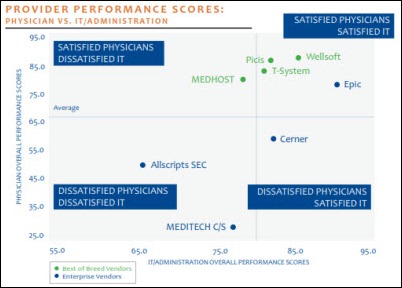
Cerner, Epic, and Siemens earn the highest ratings in ICD-10 preparedness according to KLAS, while Allscripts and Meditech score lowest. Among firms providing ICD-10 consulting, The Advisory Board earns top marks for high-quality roadmaps and best-practice sharing among firms providing ICD-10 consulting, while Deloitte has the most engagements. The majority of the market is looking to 3M and computer-assisted coding technology to aid in the transition.
Here’s the latest cartoon from Imprivata.
A local medical center in Rhode Island pitches a move to the Amazing Charts EMR to earn Meaningful Use money, adding that health services board members with medical backgrounds could help with the conversion. Several audience members objected, saying they don’t want board members seeing their medical information. The board deferred the EMR decision until its next meeting.
New Jersey Economic Development Authority approves creation of a life sciences and healthcare IT accelerator that will offer the usual seed money, boot camp, mentorship, and pitch showcase.
In Canada, Saskatchewan’s privacy commissioner is investigating three cases in which health authority employees inappropriately accessed the electronic medical records of their co-workers, including one where an employee found that her name had been replaced with a vulgarity and “RIP” at the end.
A Houston medical student files suit against his school, claiming it illegally viewed his hospital medical records and expelled him based on a physician’s speculation that he had tried to commit suicide.
Weird News Andy speculates that perhaps not all things go better with Coke. Like cardiac arrhythmia, for example, in a 30-year-old mother of eight in New Zealand whose death was ruled by the coroner as being partially caused by her 2.2 gallon per day Coca-Cola habit. The sugar water liver had damaged her liver, caused all her teeth to rot out, and addicted her to the point that she experienced withdrawal symptoms when her supply ran out. Her family says they thought Coke was OK because the bottle carries no warnings, while the company complains that the coroner himself wasn’t really sure that Coke killed her.
Sponsor Updates
- Emdat posts its spring trade show and conference schedule.
- Hayes Management Consulting posts case studies of some of its projects.
- HealthCare Anytime and ICA partner to leverage ICA’s interoperability technology with HealthCare Anytime’s patient portal.
- Informatica’s Chief Product Officer Girish Pancha participates in this week’s Pacific Crest Emerging Technology Summit in San Francisco.
- Truven Health Analytics adds enhanced reporting functionality and flexibility to the latest versions of its pharmacy intervention and infection prevention products.
- Unity Health System (NY) executives will share details of how they leveraged public and private HIEs to enable a community diabetes collaborative during a March 21 Webinar hosted by dbMotion.
- Capario realizes double-digit revenue growth from its provider base in 2012 and increased adoption of its portal application.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.













































































































Move your quotes to where they should be and it's no longer politics-in-the-blog, but instead a fact that's true at…