Top News

Healtheway announces its nine founding organizations. The public-private partnership will provide operational support for the eHealth Exchange, formerly known as the Nationwide Health Information Network Exchange.
Reader Comments
From Site Watcher: “Re: HIStalk. Happy 10th anniversary!” Thanks! It has gone by quickly.
From Doug: “Re: Meaningful Use security risk analysis. I would be interested in which of your sponsors offers consulting engagements, especially those appropriate for a 100-bed community hospital.” Thanks for showing preference to HIStalk’s sponsors, any of which that can help Doug can contact me and I’ll forward your information.
From Vascular Surgeon: “Re: health data. A Wired graphic from April finds that Kaiser Permanente’s data set is 31 petabytes, six times the size of the digital collection of the Library of Congress.”
HIStalk Announcements and Requests
 Highlights from HIStalk Practice this week include: the top ambulatory EHR, PM, and clearinghouse products according to the KLAS Mid-Term Report (and don’t miss the readers’ comments about the rankings.) A computer outage in the Canadian province of Alberta causes 202 practices to lose access to patients’ charts for over five hours. Almost half of practicing physicians are dissatisfied with their jobs. CMS publishes updated 2014 clinical quality measures for EPs. Technology could improve treatment outcomes for children with chronic illnesses. I whine and wonder about waiting at my doctor’s office. I love new readers almost as much as I love ambulatory HIT news, so sign up for the e-mail updates when you are perusing the news. Thanks for reading.
Highlights from HIStalk Practice this week include: the top ambulatory EHR, PM, and clearinghouse products according to the KLAS Mid-Term Report (and don’t miss the readers’ comments about the rankings.) A computer outage in the Canadian province of Alberta causes 202 practices to lose access to patients’ charts for over five hours. Almost half of practicing physicians are dissatisfied with their jobs. CMS publishes updated 2014 clinical quality measures for EPs. Technology could improve treatment outcomes for children with chronic illnesses. I whine and wonder about waiting at my doctor’s office. I love new readers almost as much as I love ambulatory HIT news, so sign up for the e-mail updates when you are perusing the news. Thanks for reading.
Some of the interesting recent posts on HIStalk Connect are (International) White Collar Healthcare, Mobile Health App Platform Choices, Apple Markets Its Role in Global mHealth, and Start Me Up HIT Event. Get e-mail notification of new HIStalk Connect posts by signing up.
I’ll be surveying the HIStalk Advisory Panel of primarily CIOs again this week. Let me know if you have a question you’d like me to ask them.
Welcome to new HIStalk Platinum Sponsor Logicare. The Eau Claire, WI company offers patient instructions for hospitals, clinics, and EDs that integrate with all major EHRs including the VA’s VistA. Clinicians enjoy the ability to create a patient-specific teaching document in just a few clicks, while patients can actually understand that document since the content is written at a sixth-grade reading level. Patient instructions are offered for 6,300 topics and the system has earned numerous ONC certifications, making it easy to meet the Meaningful Use requirement to provide electronic discharge instructions (flash drive, secure e-mail) at the time of discharge for patients who request them. Thanks to Logicare for supporting HIStalk.
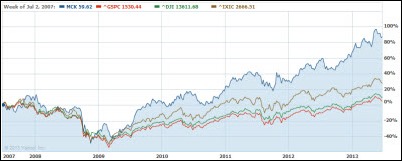
Acquisitions, Funding, Business, and Stock

Clinical Outcomes Management Systems, a provider of disease management technology for the long-term care industry, secures a minority investment of $21 million from Summit Partners.
Agilum Healthcare Intelligence raises $1.82 million of a $2.32 million equity offering.
Sales
Polyclinic Surgery Group (WA) selects ProVation medical software from Wolters Kluwer Health.
The Georgia Department of Community Health selects Truven Health Analytics to build and implement the Georgia Health Information Network.

Chinese Hospital (CA) will deploy NextGen Inpatient Clinicals.

KishHealth System (IL) selects PerfectServe clinician-to-clinician communications platform for two of its hospitals.
WellStar Health System (GA) will deploy Capsule’s DataCaptor software across its five hospitals.
People

Eastern Maine Healthcare Systems announces that VP/CIO Catherine J. Bruno will retire in December.

Ernst & Young names Encore Health Resources CEO Dana Sellers its 2013 Entrepreneur of the Year for Healthcare in the Gulf Coast Area.
Jerry Dennany (Allscripts) joins RazorInsights as CTO.
UltraLinq Healthcare Solutions appoints Ross Hoffman, MD (MedSolutions) CMO.
Announcements and Implementations
Caradigm announces the availability of Provisioning v4.0, which manages clinician access to applications while supporting data privacy regulations.

EHealth Technologies breaks ground on its new company headquarters in Rochester, NY.
Cerner launches a pilot of the Primary Health Network, a health model that uses retail locations as access points for wellness screenings.
Government and Politics
The HHS Office of Inspector General audits four Texas RECs and concludes that each has met the scope of services in their cooperative agreements with the ONC. The audits are the first of their kind by the OIG and focused on outreach activities, vendor selection and implementation assistance, and workflow analysis.
The VA announces the availability of eBenefits, an online portal that will allow veterans to file disability compensation claims electronically.
Today’s best use of a “This Is Spinal Tap” reference in a tweet comes from, interestingly enough, the federal government.
Other

Unionized nurses with Affinity Medical Center (OH) call on hospital officials to delay this weekend’s implementation of Cerner EMR, saying patients will be at risk because the nurses have not received sufficient training and will be short staffed during the first days of the live. The nurses detailed their concerns in a letter to hospital officials, but claim that hospitals officials refused to meet with them and would not accept the letter.
Here’s athenahealth’s Jonathan Bush speaking at TEDMED 2013 on healthcare profits, pointing out that non-profit hospitals often make bigger margins than Exxon. “In the mid-1990s, healthcare was annoyingly affordable – annoying if you’re one of the hospitals.” He names names.

Cone Health (NC), facing a $30 million annual budget shortfall, will lay off 150 employees. Both Cone and nearby Wake Forest University Baptist Medical Center say their Epic implementation costs hurt their bottom line at least temporarily.
Sponsor Updates
- HealthEdge, a provider of IT solutions for healthcare payors, partners with NTT DATA to transition Independent Health and Riverside Health to the HealthRules product suite.
- Divurgent posts a video of its DIVOLYMPICS employee spring games event.
- Two members of Wellcentive’s implementation team earn NCQA certification as content experts for patient-centered medical homes.
- Access partners with The Last Well to bring clean water to all of Liberia.
- A Deloitte Center for Health Solutions report explores how CIOs are navigating day-to-day management challenges.
- Visage Imaging publishes “Three topics you may have missed from #SIIM13” as a follow-up to the recent Society for Imaging Informatics in Medicine 2013 meeting.
- ISirona President Peter Witonsky lists key criteria for evaluating a medical device data system.
- GetWellNetwork announces the Transformative Health Series, a series of short films that recount the personal journeys of patients, families, caregivers, and healthcare professionals who are shaping the patient engagement movement.
- API Healthcare opens its annual conference with a keynote address featuring Paul Spiegelman, author of Patients Come Second: Leading Change by Changing the Way you Lead.
- Verisk Health announces the agenda and speakers for its 2013 national conference September 18-20 in Orlando.
- The Association for Healthcare Documentation selects Emdat as a nominee for the Innovation Through Technology Award.
- A local publication features Canton-Potsdam Hospital (NY) and its online bill-pay service operated by Instamed.
- Strata Rx announces the schedule for its O’Reilly Strata Rx Conference September 25-27 in Boston.
- Aspen Advisor consultant Claudia Blackburn will discuss how to empower population health during a June 25 Webinar.
- Wellsoft’s EDIS earns the top rating for EDIS and Imprivata takes the top spot for Single Sign-On in the KLAS 2013 Mid-Year Performance Software & Services report.
- Former CMS Administrator Donald Berwick, MD discussed the future of healthcare at this month’s 22nd Annual Midas User Symposium.
EPtalk by Dr. Jayne

The American Medical Association’s House of Delegates met in Chicago this week. One of their resolutions addresses sitting in the workplace. Employers are encouraged to make alternatives available including standing desks, treadmill desks, and isometric balls. I’d love to have a treadmill desk, although I spend half my day on conference calls which would render it almost useless. Several schools in my area are experimenting with standing desks in the classroom, citing famous users Thomas Jefferson, Winston Churchill, Charles Dickens, and Ernest Hemingway.
I loved this piece on batch workflow for the medical office that turned up on KevinMD this week. It should be required reading for EHR users. Author Dike Drummond, MD compares physicians that respond to popups and messages in the EHR to a dog with a tennis ball that can’t choose to not chase it once thrown. Watching my colleagues become totally distracted with Instant Messenger, Twitter, Facebook, and e-mail all day long, I can’t help but agree.
Dr. Gregg tweeted earlier in the week about the fundraising effort for Scanadu Scout, being billed as the first real medical tricorder. I e-mailed myself to look at it later and am happy to see that they have raised over a million dollars. I also learned that the Scout is built on the same platform as the Curiosity Rover, which is pretty cool if you’re a science geek like me. Scanadu hopes to use backers to gather data to help refine its algorithms as well as to prepare for FDA approval as a medical device.
Speaking of Twitter, Bill Gates @BillGates noted this week that he is “Excited to join the 200M+ strong @LinkedIn community.” I wonder if his connections will start endorsing him for skill sets that he doesn’t actually have, which is what my connections recently started doing? It’s definitely been amusing.
I’m excited about the new HIStalk webinar series, but unfortunately my day job keeps interfering with my potential attendance. Next week’s webinar addresses “Using Clinical Language Understanding & Infrastructure Planning as Key Strategies to Ensure Clinical Revenue Integrity with ICD-10” and you can register here. I’ll likely register anyway with the hopes that my conflicting meeting will cancel – hope to see you there!

We’ve all heard horror stories about organizations dumping medical records rather than shredding them or unintentionally misplacing paper charts. Now that patients are receiving copies of their visit summaries and other documents at every visit, there’s an increased chance that we’re going to see more than grocery receipts and shopping lists blowing in the wind. Kudos to my friends at DISC Corporation who made sure the full-color copies of a patient’s colonoscopy report made it to the shredder. Not every patient-facing document has a patient or practice address, so that was probably the most ethical course of action.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.





































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en