Top News
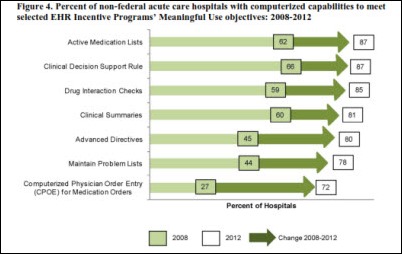
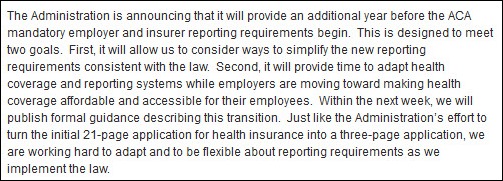
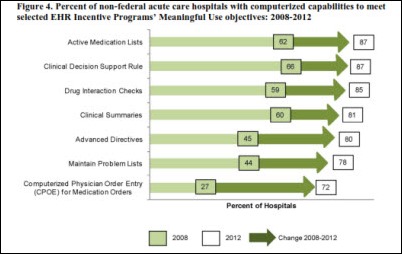
ONC releases its report to Congress on healthcare IT and HIE adoption through April 30, 2013, basically a predictably uncritical annual report of its activities. I chose this graphic randomly, then immediately noticed the common mistake of saying “Advanced Directives” instead of “Advance Directives” (you specify them in advance, but they aren’t necessarily advanced.)
Reader Comments
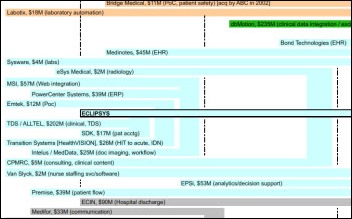
 From Chris ToeBall: “Tenet-Vanguard deal. The merger could be good news for a lot of vendors, starting with Tenet’s Conifer Health Solutions.” Tenet President and CEO Trevor Fetter says in a conference call that Conifer will provide RCM services to Vanguard’s 21 hospitals, which could provide a 28 percent boost to revenues. Less clear is the impact on athenahealth, which provides services for Vanguard’s ambulatory clinics, and McKesson, which serves Tenet’s clinics.
From Chris ToeBall: “Tenet-Vanguard deal. The merger could be good news for a lot of vendors, starting with Tenet’s Conifer Health Solutions.” Tenet President and CEO Trevor Fetter says in a conference call that Conifer will provide RCM services to Vanguard’s 21 hospitals, which could provide a 28 percent boost to revenues. Less clear is the impact on athenahealth, which provides services for Vanguard’s ambulatory clinics, and McKesson, which serves Tenet’s clinics.
HIStalk Announcements and Requests
 HIStalk Practice highlights from the last week include: Humana takes the top spot in athenahealth’s 2013 PayerView Report, while Medicaid continues to underperform. Financial management issues are the most challenging difficulties currently facing group practice executives. Consumer Reports publishes an excellent overview of the PCMH model. The AMA votes to lobby CMS for a two-year grace period to avoid complying with the ICD-10 transition – which seems like wasted energy to me, given the ONC’s promise to hold firm on the current October 2014 deadline. CMS concludes that the adoption of EHRs in community practices doesn’t necessarily impact costs. Dr. Gregg amuses with a fairy tale in the kingdom of happy healthcare. Maybe HIStalk Practice isn’t exactly summer beach reading, but there is still lots of good stuff to check out. Thanks for reading.
HIStalk Practice highlights from the last week include: Humana takes the top spot in athenahealth’s 2013 PayerView Report, while Medicaid continues to underperform. Financial management issues are the most challenging difficulties currently facing group practice executives. Consumer Reports publishes an excellent overview of the PCMH model. The AMA votes to lobby CMS for a two-year grace period to avoid complying with the ICD-10 transition – which seems like wasted energy to me, given the ONC’s promise to hold firm on the current October 2014 deadline. CMS concludes that the adoption of EHRs in community practices doesn’t necessarily impact costs. Dr. Gregg amuses with a fairy tale in the kingdom of happy healthcare. Maybe HIStalk Practice isn’t exactly summer beach reading, but there is still lots of good stuff to check out. Thanks for reading.
On the Jobs Board: Data Analyst Meaningful Use, Healthcare Software Project Manager, Resolute PB Team Lead.
Acquisitions, Funding, Business, and Stock
Craneware warns that its revenues and earnings will be below market forecasts, saying it will likely not close one of its large sales opportunities despite increased levels of sales activity.
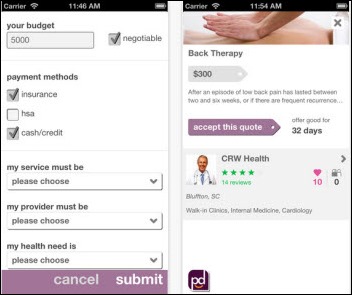
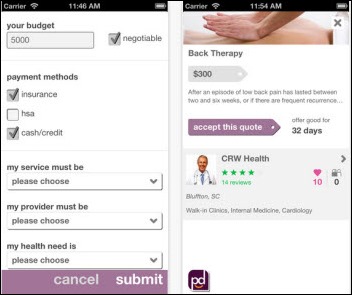
PokitDok, a startup that offers a platform for healthcare providers to advertise directly to consumers, raises $4 million in funding.
Sales
Erlanger Health System expands its relationship with MModal to include MModal Fluency Flex for creating reports and documenting patient records.

Slidell Memorial Hospital (LA) will implement Medhost’s EDIS and ED PASS for self-service patient check-in.
Piedmont Orthopaedic Associates (SC) selects SRS EHR.

South Georgia Medical Center will implement RelayHealth’s HIE platform.
ProMedica’s Lenawee Physician Hospital Organization (MI) selects Wellcentive’s population health management and data analytics solutions.

North Shore-LIJ Health System chooses InterSystems HealthShare for connectivity of all its systems in a $25 million deal. Competitor Allscripts dbMotion, now owned by NS-LIJ’s incumbent EHR vendor, wasn’t mentioned.

The Miami VA chooses GetWellNetwork for in-room entertainment, Internet access, and patient education under a $2.4 million contract.
People
CareTech Solutions appoints Brian Connolly (Oakwood Healthcare) chairman of the board, replacing Peter Karmanos.

Chris Bauleke (RelayHealth) joins Healthland as CEO. Former CEO Angie Franks (above) continues as president.

PatientPoint hires John McAuley (Allscripts) as COO and Eldon Richards (UnitedHealth Group) as VP of engineering and technology services.

Nordic Consulting promotes Vivek Swaminathan to chief consulting officer.

Jacobus Consulting names Noel Allender (Beacon Partners) managing director of its Epic practice.

RemitDATA names Michael Kallish (MPV – above) SVP of business development and Jim Harter (e-Rewards) CTO.

Imprivata President and CEO Omar Hussain is named as an Ernst & Young Entrepreneur of the Year in New England.
Huron Consulting hires Tracey Mayberry (CSC) and Kevin Smith (MedeAnalytics) as managing directors in its Huron Healthcare practice.
Announcements and Implementations
Cerner achieves HDI Support Center Certification.
Quest Diagnostics makes its Care360 Solution Suite available through AT&T Healthcare Community Online.
The local TV station profiles Cedar Rapids, IA-based healthcare website developer Geonetric, pointing out that none of its 70 employees have managers, food is available and free, and flex time and sabbaticals are standard. According to the HR director, “We want you to enjoy life and experience life, and do great work for us. And it’s awesome.” It says the company will hire another 130 people and move into a new building. Its website declares it to be the “coolest healthcare Web company. In the history of ever.” According to its site, employees get free ice cream when a new client is signed, dress is casual, Grillin’ Friday is BYOM (bring your own meat), and there’s a knitting circle.

AMIA’s review course for the clinical informatics subspecialty certification that starts in October is scheduled for July 15 availability. Live courses started in April.
Caristix introduces Caristix 2.0, the latest version of its HL7 interface lifecycle management platform.
Allscripts announces that Sunrise Acute Care 6.1 and Sunrise Ambulatory Care 6.1 have been certified as Complete EHRs under ONC 2014 Edition criteria.
Penn State Hershey Children’s Hospital uses Amcom Messenger for calling Code Blue.
Cerner announces its support for Blue Button +.
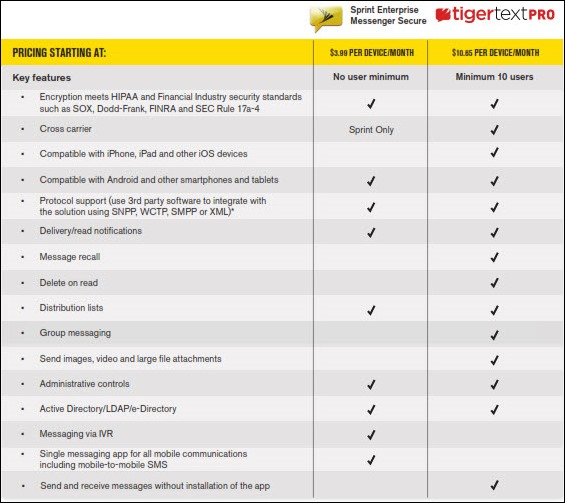
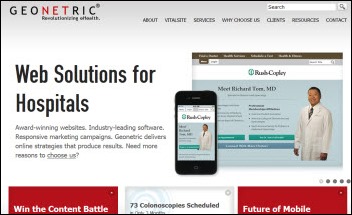
Sprint announces the availability of the TigerText HIPAA-compliant secure messaging solution and a less-expensive offering powered by TeleMessage branded as Sprint Enterprise Messenger – Secure.
Government and Politics
Industry officials testifying before the Senate Committee on Finance offer opinions on how to improve healthcare quality. Concerns raised include:
- CMS should consider reducing the 1,000+ quality measures currently used for reporting and payment programs and develop measures that are more outcome- and patient-oriented.
- Many traditional EHRs, especially those used by small physician practices, are not well designed, which limits a provider’s ability to produce meaningful data for quality reporting.
- Provider payments need to be better aligned with outcomes and quality reporting.
- The government should go beyond the EHR incentive program and work towards the development of a framework for care coordination and long-term care outcome measurements.
CMS redesigns its Physician Compare Website to include details on physician or practice specialties, EHR use, board certification, and hospital affiliation.
Practice Fusion launches a medical imaging API that will allow its practice users to connect to imaging centers, allowing physicians to receive results electronically for Meaningful Use and giving imaging centers potential new business. Use is free for the practice, but not for the imaging center.
Technology

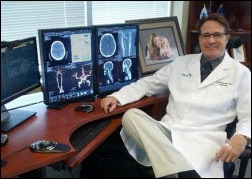
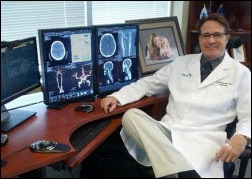
Arizona-based surgeon Gil Ortega, MD performs the world’s first orthopedic trauma surgery while wearing Google Glass, which he says will be useful for teaching students who will have a clear view of the sterile field, recording the surgery, and requesting information via the device.
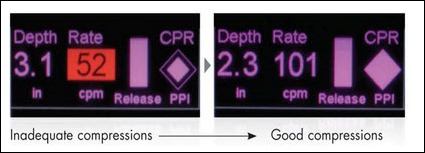
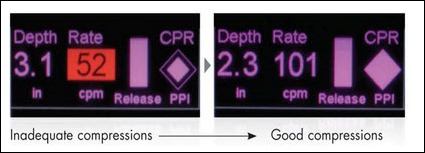
A study finds that the survival rate for non-hospital heart attack patients doubled when paramedics performing CPR were coached using Real CPR Help software that is standard on ZOLL Medical’s defibrillators.
Other
A study published in JAMA finds that treating the costliest Medicare patients in doctors’ offices instead of ERs may not save as much money as previously hoped, only about 10 percent.
Porter Research looks at ICD-10 readiness among physician practices and finds that most are concerned with disruptions in cash flows when the new code set goes into effect. Of practices that have not yet started preparing for the transition, more than a third believe they have adequate time to prepare. The rest either don’t know where to begin or lack time, staff, or training resources.
Healthcare attorney David Harlow, who writes HealthBlawg, launches a crowdfunding project called Hacking HIPAA. It will a create a new Common Notice of Privacy Practices that will give patients an explanation of potentially beneficial electronic transfer of their data (e-mail, cloud, video, text messaging) and obtain their consent for its use before the new Omnibus HIPAA Rule “will make cloud hosting of healthcare projects untenable very soon.” He’s hoping to raise $10,000. That’s Fred Trotter in the video.
Who proofed this announcement? It’s apparently how they role.
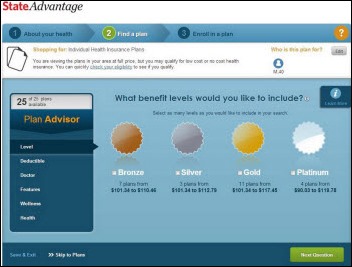
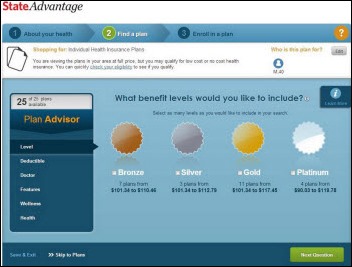
Kaiser Health News test drives the health insurance exchange enrollment software that will be rolled out in Minnesota, Maryland, and DC for the scheduled October 1 launch.
Weird News Andy hopes the patient remembers his native language. A 69-year-old man being treated for stroke at Robert Wood Johnson University Hospital is sent unconscious on a charter flight back to his native Poland when he’s found to be uninsured and living in the US illegally.
Sponsor Updates
- Visage Imaging releases a case study about the use of the Visage 7 Enterprise Imaging Platform by teleradiology provider Rays.
- UltraLinq Healthcare will incorporate cardiology decision support tools from DiACardio into its cloud-based image management and reporting system.
- Karen Marhefka, MHA, RHIA of Encore Health Resources will present a primer on value-driven healthcare at the Texas AHIMA convention today (Friday, June 27) at 1:30 p.m. Central time.
- Quantros announces the patent pending status of its Smart Classification technology for classifying incident reports in real-time.
- The Center for Economic Growth recognizes etransmedia Technology with a technology innovation award.
- Cornerstone Advisors announces its #1 KLAS mid-term ranking in the Planning and Assessment category and its projected 100 percent growth this year.
- Nuance Communications names 11 hospitals as 2013 winners of the Million Dollar Club, having saved at least $1 million by using Dragon for medical transcription and clinical documentation.
- Xerox VP Ed Gala asks JetBlue co-founder Ann Rhoades and hospital IT executives what airlines and hospitals have in common.
- Greenway Medical will integrate the inpatient EHR of Health Management Systems its PrimeSUITE solution.
- Nuesoft Technologies celebrates its 20th anniversary.
- Kareo integrates its PM application with Demandforce, an Intuit company, to help practices build their online reputations and proactively engage with patients for preventive or recurring care.
- Sandlot Solutions CEO Joe Casper discusses improving care with HIE and data analytics.
- Verisk Health recaps its recent Webinar featuring Granite Healthcare Network’s (NH) use of data analytics to provide cost-effective care.
- Versus offers a replay of the AHA-hosted Webinar on improving safety measures with RTLS featuring Western Maryland Health Systems. Versus also offers a case study that details how the organization reduced elopements and improved response times with RTLS technology.
- AT&T partners with Project HOPE to improve women and children’s healthcare in Asia and Africa.
- Northern Ireland’s health minister writes about the transformation of the country’s healthcare system using technology from Orion Health.
EPtalk by Dr. Jayne
The National Uniform Claim Committee announces that CMS has finally approved the new 1500 claim form. It allows identification of whether ICD-9 or ICD-10 is being used and expands the number of diagnosis codes which can be reported. The deadline for transition to the new form seems to be fluid. Providers should contact their clearinghouses to determine when they will begin accepting the form and should work with their vendors to ensure practice management systems can generate the new form.
HIMSS calls for proposals for pre-conference symposia. New this year, they’re looking for abstracts for full-day preconference programs. The deadline is July 22 and those selected will be notified in August.

Medical Economics identifies “10 regulatory irritants fueling physician dissatisfaction” according to a Physicians Foundation study. The list includes:
- Meaningless work
- Box checking
- Data is replacing information
- Quality
- Site of Service
- Fraud
- Sustainable growth rate (SGR)
- PCORI and IPAB
- Costs
- The government is coming between me and my patients
Bloomberg discusses the top US states where physicians have gone digital. I was surprised to see Washington, DC at the bottom along with Louisiana, New Jersey, and Connecticut. Wisconsin is at the top, followed by Minnesota, North Dakota, and Massachusetts.
Note to marketing folks: always test your mail merge skills before sending out blast e-mails (and especially snail mail). This week I’ve been on the receiving end of two charity letters asking me to send my pledge (which wasn’t a pledge but an outright donation) and now an e-mail addressed to “Dennis.” First impressions are everything, folks.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.












































































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en