Top News
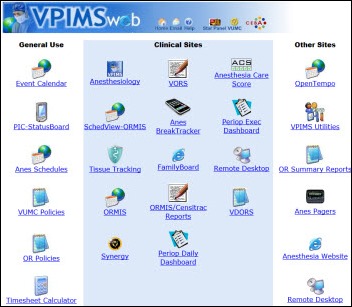
A newly unsealed Medicare fraud lawsuit against Vanderbilt University Medical Center claims that its internally developed Vanderbilt Perioperative Information Management System (VPIMS) was used to bill services for physicians who were not physically present. Documents filed with the lawsuit, which claims the fraud spanned more than 10 years, include a Vanderbilt email telling surgeons to avoid documenting which rooms they were actually covering because “it only confuses and complicates the billing and documentation process.” The lawsuit concludes, “VIPIMS’ purported improvements in billing efficiency are, in fact, largely a function of Vanderbilt’s development of mandatory default software settings that require its physicians, in all instances, to document that they meet Medicare’s conditions for payment.” VUMC says its own investigation has uncovered no billing irregularities and vows to defend itself vigorously.
Reader Comments

 From Bronwyn: “Re: Cerner Dynamic Documentation. Do you know of any hospitals currently using it who would be willing talk to a CIO about their experience?” Readers, send Inga a note if you can help.
From Bronwyn: “Re: Cerner Dynamic Documentation. Do you know of any hospitals currently using it who would be willing talk to a CIO about their experience?” Readers, send Inga a note if you can help.
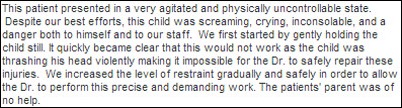
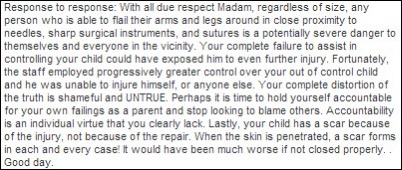
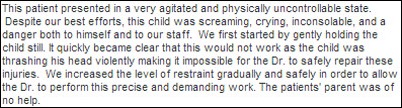
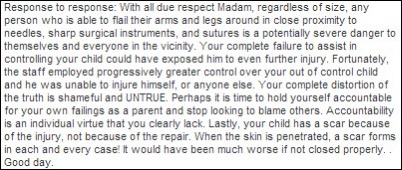
 From Reviewer: “HIPAA violation. If this isn’t the most egregious HIPAA violation ever, I don’t know what is!” A parent of a three-year-old patient posts a negative review on Yelp following a visit to a Phoenix plastic surgery clinic. The practice’s operations coordinator posts a reply that includes significant details about the patient and the office visit, as well as some harsh criticism of the mother and her parenting skills. Rebecca Fayed, associate general counsel and privacy officer at The Advisory Board Company, provided us her assessment:
From Reviewer: “HIPAA violation. If this isn’t the most egregious HIPAA violation ever, I don’t know what is!” A parent of a three-year-old patient posts a negative review on Yelp following a visit to a Phoenix plastic surgery clinic. The practice’s operations coordinator posts a reply that includes significant details about the patient and the office visit, as well as some harsh criticism of the mother and her parenting skills. Rebecca Fayed, associate general counsel and privacy officer at The Advisory Board Company, provided us her assessment:
I think that providers (or any covered entity or business associate for that matter) need to be particularly careful when posting anything online, whether it be on Yelp or other social media sites, that could be interpreted as a disclosure of protected health information. In this post, HHS-OCR could view the response by the provider as a disclosure of protected health information not permitted by the HIPAA Privacy Rule.
From Former Employee: “Re: Experian Healthcare, formerly Medical Present Value. Underwent its third round of layoffs this week, including its entire SME group and other client support staff. Sales are significantly down under Experian.” Unverified.

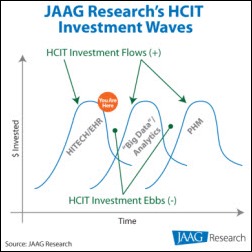
From small_data: “Re: misuse of the ‘Big Data’ buzzword. Simply storing data for archival purposes without intent of using that data for any kind of quantitative analysis is surely not ‘Big Data.’” The solution in question stores medical images. Everybody with a database now has “Big Data.” If they can export that information to Excel, they have enterprise analytics and business intelligence. If that worksheet can be emailed, they offer interoperability. If the worksheet can be stored on a Web server, it’s scalable and cloud-based. These are no longer technical terms with precise meanings; they have been hijacked by the sales and marketing people.

From Over It: “Re: Jody Albright, CIO, Overlake Hospital. Internal email says her position was eliminated and chief compliance officer will take on CIO duties. She had limited involvement with the Epic project and the go-live was a firestorm on several levels.” Unverified, but above is a purported internal email forwarded my way.
HIStalk Announcements and Requests
 The latest news from HIStalk Practice includes: use of an EMR that includes automated growth monitoring helps doctors pick up on cases of possible growth disorders among kids.The AMA offers a toolkit (perhaps a little late) to help physicians prepare for upcoming HIPAA changes. HIT expenditures in physician offices jumped 28 percent from 2008 to 2012. Will cloud-based EHR/PMs really save practices from acquisition? Patients from Advocate Medical Group file a class-action lawsuit following the theft of unencrypted computers. Rhode Island primary care practices can earn up to $10,000 to connect to the state’s HIE. Culbert Healthcare Solutions VP Brad Boyd offers some advice for defining and measuring an EHR’s ROI. Thanks for reading!
The latest news from HIStalk Practice includes: use of an EMR that includes automated growth monitoring helps doctors pick up on cases of possible growth disorders among kids.The AMA offers a toolkit (perhaps a little late) to help physicians prepare for upcoming HIPAA changes. HIT expenditures in physician offices jumped 28 percent from 2008 to 2012. Will cloud-based EHR/PMs really save practices from acquisition? Patients from Advocate Medical Group file a class-action lawsuit following the theft of unencrypted computers. Rhode Island primary care practices can earn up to $10,000 to connect to the state’s HIE. Culbert Healthcare Solutions VP Brad Boyd offers some advice for defining and measuring an EHR’s ROI. Thanks for reading!

Welcome to new HIStalk Platinum Sponsor EXTENSION. The Fort Wayne, IN company offers contextual alerting, secure messaging, and care team collaboration technologies, including specific solutions that address Joint Commission’s 2014 National Patient Safety Goal, “Improve the safety of clinical alarm systems.” First-generation systems just throw out a lot of alerts, but EXTENSION’s next-generation platform combines alarm safety software with a secure text messaging solution to optimize the workflow involved with clinical event response. The company’s HealthAlert solution solves the challenge of getting important clinical event notifications in the hands of clinicians, routing critical lab results, stat orders, staff assignment, patient monitoring, and patient nurse call requests. The system prioritizes the alerts, escalates based on defined rules, announces the event verbally to the recipient, and maintains an audit trail. It works with Android, Apple, Ascom, Cisco, Spectralink, and Vocera devices, including a mobile app that can run on a clinician’s own smartphone. Thanks to EXTENSION for supporting HIStalk.
I found this short introductory YouTube video from EXTENSION called “The Power of the EHR-Extender.”
On the Jobs Board: Manager North America Professional Services West, Implementation Engineer (East Coast), Services Operations Manager.
HIStalk Webinar


Informatica will present “Best Practices for Delivering Better Quality Care and Reducing Preventable Patient Readmissions” on Thursday, September 26 from 1:00 – 1:45 p.m. Eastern. Speakers are George Brenckle, PhD, SVP/CIO of UMass Memorial Health Care and Richard Cramer, chief healthcare strategist of Informatica (I interviewed him awhile back). Register here.
I recorded the HIPAA Omnibus webinar given by Rebecca Fayed and Eric Banks of The Advisory Board Company earlier this week and posted it to YouTube. The slides are here. Thanks to Rebecca and Eric, who stepped up when I asked for volunteers to run through the changes with HIStalk readers. We had a nice turnout, and in typical Advisory Board fashion, not a second was wasted due to inadequate preparation or lack of focus.
Acquisitions, Funding, Business, and Stock
Covisint will raise at least $64 million in its IPO by offering 6.4 million shares at an expected price of $9 to $11. The company generated $94 million in revenue for the 12 months that ended June 30.
Three partners of Morgenthaler Ventures create a new management company and the $175 million Canvas Venture Fund that will focus on early stage investments of $5 to $15 million in mobile, health IT, financial technology, and enterprise technology. The parent VC company invested in physician social network Doximity and free EMR vendor Practice Fusion.
The CSI Companies acquires Atlanta-based IT staffing firm Anteo Group.

Lincor Solutions moves its headquarters from Ireland to Nashville.
Sales

Estes Park Medical Center (CO) will implement HealthCare Anytime’s patient portal technology at its hospital and outpatient clinic.
The Valley Hospital (NJ) selects Merge Healthcare’s CTMS for Investigators to manage its clinical research operations.
UHS-Pruitt Corporation, a provider of post-acute care services, will implement healthcare analytics and population health solutions from Caradigm.
The 110-provider Prima CARE (MA/RI) selects Ingenious Med’s mobile revenue capture technology.
Washington Orthopaedics & Sports Medicine (DC/MD) selects SRS EHR for its 11 providers and three locations.
People

Wellcentive names Tom Zajac (Elsevier) CEO.

Health Catalyst appoints David K. Crockett, PhD (ARUP Laboratories) senior director of research and predictive analytics.

Robert Porr (Accenture) joins Sandlot Solutions as EVP of sales and marketing.

Nancy Killefer (Department of the Treasury, IRS Oversight Board, McKinsey & Company) joins the board of The Advisory Board Company.

University of Missouri-Kansas City hires Mark Hoffman, PhD (Cerner) as director of bioinformatics core and associate professor to establish its Center for Health Insights informatics program.


Stanford Hospitals & Clinics (CA) promotes Pravene Nath, MD to CIO and Christopher Sharp, MD to CMIO.
MGMA-ACMPE names Garth Jordan (EDUCAUSE) COO.
Prime Healthcare Services (CA) will implement Infor financials, supply chain and human capital management, clinical bridge, and analytics.
Announcements and Implementations
Quest Diagnostics joins LabCorp and almost all of Colorado’s large hospital laboratories in connecting to the Colorado RHIO.
The HIEs Michigan Health Connect and Michiana HIN will share health records between Michigan and Indiana providers.
The Patient-Centered Outcomes Research Institute board of governors issues 71 awards totaling more than $114 million to fund comparative clinical effectiveness research, including studies to improve the applicability of data collected through EHRs and social media sites and methods for engaging minority patients and caregivers in patient-centered health research.

Ivo Nelson’s Next Wave Health forms Smart Social Media, Inc., a software company that will develop a healthcare social media platform. Next Wave Health acquired the OneXPage social media platform from Digiapolis, Inc., founded by Minneapolis entrepreneur Eric Lopez, who will be CEO of Smart Social Media.
Gastroenterology EHR vendor gMed will use behavior-based prescription management messaging from LDM Group to improve medication adherence and highlight therapy options.
Government and Politics
ONC launches a patient matching initiative to seek common denominators and best practices being used by private healthcare systems and federal agencies.
Innovation and Research
The use of an electronic decision support tool linked to patients’ EMRs helped reduce deaths from pneumonia in EDs by up to 25 percent according to researchers from Intermountain Healthcare and the University of Utah.
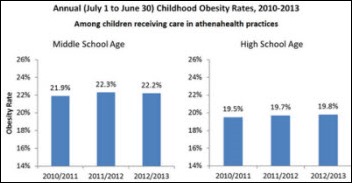
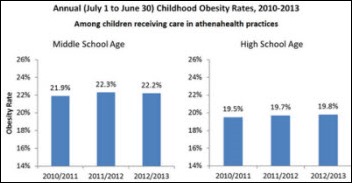
 An athenahealth analysis of EHR data from its user network reveals no signs of a national decline in childhood obesity over the last three years. Athenahealth obviously has a wealth of clinical data at its disposal and this type of analysis is interesting and arguably beneficial. However, are practices and patients aware of how athenahealth and other EMR companies may be using personal health information? More importantly, should they? To the latter question I say yes, and mechanisms should be in place to allow practices and patients to opt in or out.
An athenahealth analysis of EHR data from its user network reveals no signs of a national decline in childhood obesity over the last three years. Athenahealth obviously has a wealth of clinical data at its disposal and this type of analysis is interesting and arguably beneficial. However, are practices and patients aware of how athenahealth and other EMR companies may be using personal health information? More importantly, should they? To the latter question I say yes, and mechanisms should be in place to allow practices and patients to opt in or out.
Technology
AirStrip will develop and optimize its AirStrip ONE solution for Samsung tablets running Android and Windows 8.1 operating systems, as well as Samsung convertible and all-in-one desktop and laptop PCs with touch screens.

Lt. Dan covers the iPhone 5S announcement in his excellent HIStalk Connect analysis, “Apple Comes Up Big On The iPhone 5S Unveil: What it Means for Healthcare.”
Other
The Tax Increment Financing Commission of Kansas City approves a $1.635 billion incentive for Cerner’s proposed plan to develop a 4.5 million square foot mixed-used campus.
VA psychiatrists and researchers are using natural language processing and query searches of doctors’ free-text notes to flag patients who present a clear risk of suicide.

Crittenton Hospital (MI) will provide free electronic copies of medical records to the families of patients treated by Farid Fata, MD. Fata is the Michigan Hematology Oncology physician accused of deliberately misdiagnosing patients and improperly administering chemotherapy as part of a $35 million Medicare billing fraud scheme. The hospital provides records free only to medical doctors, but reversed its policy after the doctor’s patients staged a protest.
The New England Journal of Medicine gets banned from posting pictures on Facebook after running a medical image of a patient with scrotal calcinosis, which Facebook found pornographic. Facebook changed its mind shortly after.
Sponsor Updates
- Aventura publishes an informative and entertaining HIT Survival Handbook.
- Allscripts will add Inovalon’s quality improvement and risk score accuracy analytics to its EHR platform.
- Health leaders in Leeds, UK will evaluate whether outcomes can be improved by using Alere’s healthcare platform.
- Medseek Empower 5.0 earns CCHIT certification as an EHR Module and is compliant with the ONC 2014 Edition criteria.
- Campbell Clinic (TN) reports that its use of Emdat’s medical documentation solutions has improved documentation completion, workflow, and transcriptionist productivity.
- Billian’s HealthDATA interviews Collin Searle, social media manager for Intermountain Healthcare (UT), about the health system’s social media strategy.
- Clinovations CEO Trenor Williams discusses the need for pharma companies to use technology and think more strategically about communications with health providers and patients.
- Innovative Healthcare Solutions offers a white paper series that includes tips for a successful project outcome.
- Hot jobs on the site of Henry Elliott & Company, which specializes in Caché and M/MUMPS technology positions, include Senior M/Caché P/A, Caché M/Mumps Web Developer, VistA Analyst, and .NET/Caché Developer.
- Cleveland Clinic’s use of BI dashboards from Harris Healthcare has driven significant ROI and performance improvement, including a $10 million increase in net income.
- Intelligent InSites announces details of InSites Build 2013, an RTLS learning event October 28-30 in Fargo, ND.
- Sunquest Information Systems and the Association for Pathology Informatics will host a September 26 educational webinar on pathology informatics featuring Walter Henricks, MD of Cleveland Clinic.
- Florida Hospital Celebration Health realizes increases in key HCAHPS categories since implementing GetWellNetwork’s Interactive Patient Care and Clinical Practice Design solutions.
- UnitedHealth reports its use of InstaMed online payment option has resulted in over $3 million in payments since its late July rollout.
- Trinitas Regional Medical Center (NJ) enhances staff safety with Versus Visibility Staff Assist RTLS technology.
- Hayes Management Technology adds its go-live support and legacy support services to its website.
- Divurgent and Medix will host a Retro Arcade Event during Epic UGM. Readers may RSVP here.
EPtalk by Dr. Jayne
Mr. H mentioned that PatientSafe Solutions has joined us as a Platinum Sponsor, but I wanted to offer my own shout out for its PatientTouch system. I first saw it at HIMSS13, and as Inga can attest, was really geeked out about it. I’d love to see it installed at my institution, so maybe I’ll “accidentally” leave their information on my boss’s printer.
I spent the earlier part of this week at the AMIA Clinical Informatics Board Review Course in Chicago. There were enough sassy young female physicians in attendance, so I feel fairly safe in admitting it while being able to still remain anonymous. I even saw some sassy shoes, so I felt like I was in good company.
Why a board review, and why now? This fall marks the first opportunity for physicians to actually seek board certification in the subspecialty of Clinical Informatics through the American Board of Preventive Medicine. There’s also a pathway through the American Board of Pathology – based on the number of pathologists in the class I don’t want to neglect to mention that because I know if they’re reading they’ll correct me – but the majority of informatics physicians I know are not pathologists.
As a new specialty, they’re offering a “practice pathway” for those of us who are not fellowship-trained to seek certification, through 2017. Candidates in this pathway have to demonstrate at least 25 percent practice in clinical informatics during three of the five years preceding application. In 2018 and later, candidates will have to have completed a minimum of 24 months in an ACGME-accredited Clinical Informatics fellowship program.
Many of us are not fellowship trained. Instead we’re homegrown informaticists who have been at this quite a while. We may have done some coursework in informatics or had intensive mentoring in order to reach our level of performance. In my case, the thought of trying to go back and do a formal training program on top of working the number of hours I do currently made my skin crawl, as did the idea of spending $40,000 or more on a degree that wouldn’t raise my income or the level of respect from my peers.
After a little cajoling from a colleague, I decided to aim for certification in the first round through the practice pathway. It’s a bit daunting because it’s a brand new exam. None of us really knows what to expect, and although the Board has published an “examination content outline,” it’s pretty daunting since the level of detail they could be expecting could be all over the map. The application process was also daunting, as I had to track down former bosses who could best attest to the time I’ve spent in the field. I’ve had five bosses at three jobs in the last five years and only one is still working at the hospital where we were colleagues.
I’ve never taken a board review course before, so this seemed like a good time to try it given the breadth of the material. The class was a nice mix including average working CMIOs and high-powered names from major academic institutions. The VA and military were well represented, as were ambulatory organizations, payers, and vendors. I’m happy to report a Bowtie Index of 3.67 bpd (bowties per day) with one attendee having particularly fetching choices.
The group was pretty social and there were some key themes heard during the cocktail hour and various breaks. One is that there are quite a few institutions out there that still don’t value the contribution that a CMIO brings to the table. Many CMIOs are forced to try to do the job without the title or the appropriate level of authority. If you’re at one of those facilities who still question whether you need a CMIO, check that exam content outline to learn more about what we do and what we can bring to the table.
Another key theme is that there is never enough money to do the work that needs to be done. That goes right along with the theme that there are always more projects to be done than can be humanly accomplished. I also learned that many physician informaticists are very driven and devoted to the field – so much so that one physician sitting near me said his colleague’s inhuman level of work product clearly means that she’s a cyborg.
I’m unfortunately having to play catch up for the days out of the office, so you’ll have to wait until Monday’s Curbside Consult to hear about the rest of the course and some fun things I learned including some informatics jokes. I’ll leave you with this one in the interim:
A programmer is asked by his spouse to get some groceries. She asks, “Can you pick up a loaf of bread, and if they have eggs, get a dozen.” He returns home with 13 loaves of bread. She asks, “What happened?” His response: “They had eggs.”
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.












































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…