News 10/18/13
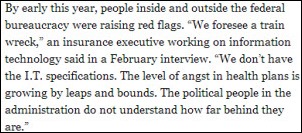
HHS Secretary Kathleen Sebelius is reported to have no intention of quitting after Republican criticism of the Healthcare.gov online insurance exchange debacle. Sebelius has acknowledged the problems, but says fixes are being put in place and those who were unable to sign up should try again. Success rates for those attempting to enroll were less than 20 percent the week of its rollout on October 1 and under 13 percent the second week, although one researcher says fewer than 1 percent of those who tried to register were successful. Another report finds that the cost for the system ballooned from the original estimate of $94 million to $292 million, with those payments going to the US federal government division of Canada-based CGI. Other estimates peg the total cost of Healthcare.gov to be more than $500 million.
Reader Comments
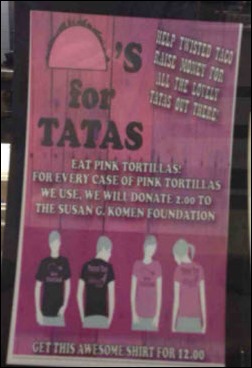
![]() From Dr. Travis: “Re: Color me pink. Breast cancer awareness month has jumped the shark this year.” Travis tells me he likes the innuendo of this poster’s message, which I believe was from the Twisted Taco restaurant in the Atlanta area. Thanks for the reminder to support breast cancer research, get screened regularly, and/or encourage your loved ones to be screened.
From Dr. Travis: “Re: Color me pink. Breast cancer awareness month has jumped the shark this year.” Travis tells me he likes the innuendo of this poster’s message, which I believe was from the Twisted Taco restaurant in the Atlanta area. Thanks for the reminder to support breast cancer research, get screened regularly, and/or encourage your loved ones to be screened.
From Reader One: “Re: from a vendor-specific forum today. ‘We inadvertently assigned 5,000 accounts to a bad debt agency. Is there a way to mass cancel?’ Now that’s what I call exciting.”
HIStalk Announcements and Requests

Welcome to new HIStalk Platinum Sponsor Boston Software Systems. The company offers an error-free workflow automation platform that allows its healthcare customers and business partners to streamline their business processes and improve productivity. Boston WorkStation lets IT departments efficiently solve problems and eliminate performance gaps in existing IT systems – integrating third-party registrations, performing eligibility checks, integrating lab results, posting payments and collections notes, performing mass updates, creating backup databases, running and distributing reports, and managing dictionaries and tables. Existing systems can be enhanced by creating new business rules and workflows and providing real-time access to external applications. IT departments love Swiss Army knife-type solutions that be used to enhance systems without vendor involvement or ongoing labor requirements, such as the hospital that’s saving 125 hours per month using Boston WorkStation to automatically create a pre-registration account at the time of scheduling or another that saves $500K by automating their materials management system to load inventory purchases and manage price updates. The company also offers Cognauto, the next-generation automation platform. The company’s products are used by over 2,500 hospital customers running many IT systems. Thanks to Boston Software Systems for supporting HIStalk and for issuing a very cool press release announcing that fact.

Thanks to Bonny and Catherine from Aventura, self-proclaimed “HIStalk minions” who volunteered to report from the American College of Emergency Physicians Scientific Assembly (ACEP13) in Seattle this week. They conducted some ED doc interviews about IT that I’ll have up later, but here are some of Bonny’s observations:
- The topic of scribes performing EMR data entry split the group, with some ED physicians expressing satisfaction in offloading tasks to what is often a pre-med student, but others feel guilty about making scribes do what some would say is their work.
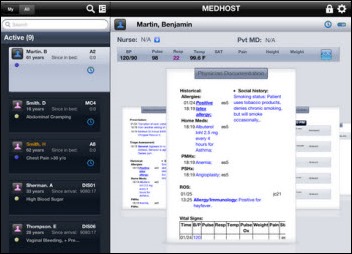
- The best-of breed EDIS vendors were there (Picis, T-System, MEDHOST) as were the big enterprise vendors with EDIS, with Epic notably being MIA.
- Education and discharge instructions vendors (Discharge 1-2-3, Elsevier ExitCare, Krames) were exhibiting.
- Bonny says MEDHOST stole the show with a patient throughput solution that pushes preemptive communication about patients from the ED or OR, such as when a patient is likely to be admitted but whose emergency care is still underway. It also offers real-time and forecasted financial operational metrics for executives.
- ACEP rented out the Space Needle, the Chihuly Museum, and the Experience Music Project for attendee events.
- In the all-important vendor swag category, Bonny lauds Interactive Health Massage Chairs, whose booth was across from Aventura’s such that Bonny and Catherine could perform their own first-hand research as well as watch attendees shed their stress and exit happy. Check out the photo above – who wouldn’t want to have a chair massage while covered lightly with a blanket right on the show floor?
![]() Highlights from HIStalk Practice this week include: a local paper profiles two physicians with opposing views on EMRs. CMS pushes a PQRS reporting deadline back three days. A vendor speaks out against shortened exhibit hours at MGMA. Most medical practices are concerned that ACA insurance exchanges will lead to increased collection burdens and lower reimbursements. Epocrates adds a provider directory to help members identify clinicians for consults and referrals. Emdeon will pay its departing CEO $2.4 million over the next two years. Thanks for reading.
Highlights from HIStalk Practice this week include: a local paper profiles two physicians with opposing views on EMRs. CMS pushes a PQRS reporting deadline back three days. A vendor speaks out against shortened exhibit hours at MGMA. Most medical practices are concerned that ACA insurance exchanges will lead to increased collection burdens and lower reimbursements. Epocrates adds a provider directory to help members identify clinicians for consults and referrals. Emdeon will pay its departing CEO $2.4 million over the next two years. Thanks for reading.
Acquisitions, Funding, Business, and Stock
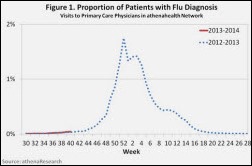
Athenahealth announces Q3 results: revenue up 43 percent, adjusted EPS $0.29 vs. $0.30, missing analyst estimates on both.
IVantage Health Analytics acquires Professional Data Services, a provider of managed care analytics and benchmarking solutions for hospitals.
StartUp Health admits 14 new companies to its three-year development program for health technology startups. Lt. Dan profiles the companies on HIStalk Connect.
Medical practice technology vendor Waiting Room Solutions changes its name to WRS Health.
Sales
Medical Services of America (SC) chooses Allscripts Homecare for its 70 home care service locations.
Elmcroft Senior Living (MO) will install Cerner CareTracker at its 85 assisted living facilities.
The 30-bed Aspire Hospital (TX) will implement clinical and financial applications from Healthcare Management Systems and physician documentation from Patient Logic.
The VA and DoD award Systems Made Simple a re-compete of the iEHR system contract for systems integration and engineering support.
Saint Luke’s Health System selects PeriGen’s PeriCALM fetal surveillance system for seven birthing hospitals in northwest Missouri and northeast Kansas.
The VA awards Harris Corporation a $60 million, four-year contract to design, install, and support the wireless infrastructure at 112 VA medical centers.
Riverside Medical Group (VA) selects athenaCollector for billing and practice management for its 300+ physicians.
The Texas Health Services Authority chooses EHNAC to develop a state accreditation program for private and public HIEs operating in Texas.
Texas Health Physicians Group selects StrataJazz from Strata Decision Technology as its integrated financial platform.
St. Luke’s Health System (ID) will implement Epic at a cost of $200 million and will offer Epic ambulatory to independent practices through an affiliate program. St. Luke’s, defending itself against antitrust claims for its purchase of Salzer Medical Group, says Epic is a superior system that will allow providers to share information with patients and with each other more easily.
People
Northwest Community Healthcare (IL) names Glen Malan (Cadence Health) VP/CIO.
OpenTempo names Jim Crook (IDX) chairman of the board, Walt Marti (GE Healthcare) chief administrative officer, and John Jordan (dbMotion) VP of sales and marketing.
Announcements and Implementations
Quantros releases IRIS 2.4, a configurable dashboard to view overall hospital performance and display trends, distribution, and variations in performance.
Government and Politics
![]() A California state appellate court rules that providers do not necessarily have liability to patients when medical records are stolen or misappropriated unless they are accessed by a third party. The ruling stems from a 2011 incident in which a UCLA Health physician’s laptop containing medical records on 16,000 patients was stolen from his home. The provider could have been liable for up to $16 million as part of the class action lawsuit, even though there was never any indication the data had been accessed. The suit was dismissed. Rebecca Fayed, associate general counsel and privacy officer at The Advisory Board Company, tells me the ruling only applies to California, which has its own statute governing the disclosure of medical information and allows affected individuals to sue for damages for certain violations. She adds:
A California state appellate court rules that providers do not necessarily have liability to patients when medical records are stolen or misappropriated unless they are accessed by a third party. The ruling stems from a 2011 incident in which a UCLA Health physician’s laptop containing medical records on 16,000 patients was stolen from his home. The provider could have been liable for up to $16 million as part of the class action lawsuit, even though there was never any indication the data had been accessed. The suit was dismissed. Rebecca Fayed, associate general counsel and privacy officer at The Advisory Board Company, tells me the ruling only applies to California, which has its own statute governing the disclosure of medical information and allows affected individuals to sue for damages for certain violations. She adds:
Although the ruling would not apply nationwide at the federal level, other states with similar state laws may look to this case for reasoning and may analogize to it even if it has no precedential value in any state other than California.
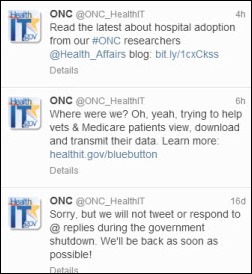
![]() The ONC Tweeters seem happy to be back at the keyboard after a 16-day furlough.
The ONC Tweeters seem happy to be back at the keyboard after a 16-day furlough.
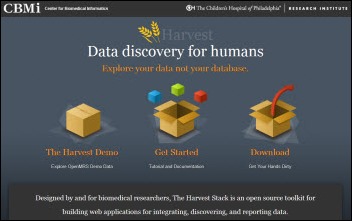
Children’s Hospital of Philadelphia (CHOP) offers Harvest, an NIH grant-funded open source software toolkit that allows biomedical researchers to explore large data sets, such as those from EHRs and genomic databases. Researchers from CHOP’s Center for Biomedical Informatics are testing Harvest against several data collections, including the Longitudinal Pediatric Data Resource that tracks data from children with conditions detected in newborn screenings.
Technology
Deloitte introduces PopulationMiner, a data analytics solution that draws clinical, financial, and operational data from Intermountain Healthcare’s warehouse to support patient-outcome analysis.
ArborMetrix integrates surgical video analysis capabilities into its reporting and analytics platform, enabling healthcare organizations to improve performance benchmarking of surgeons.
Ninety percent of surveyed nursing home physicians say their use of drug references on mobile devices prevented at least one adverse drug event the month before the survey.
Other
Virtualization software and dictation with speech recognition applications are emerging as top areas for growth potential in hospitals, according to a HIMSS Analytics report on the US hospital IT market. The demand for ambulatory EMRs and ambulatory PACS also appears to be growing.
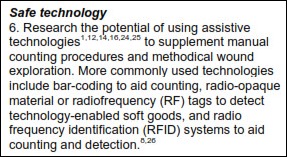
Joint Commission issues a sentinel alert warning for objects left inside surgery patients, which it says has caused 16 deaths in the past eight years. Most of the recommended actions involve processes and communication, but consideration of “assistive technology” such as RFID-tagged counting systems are also recommended.
In Canada, information on 2,000 patients of Parkwood Hospital is exposed when an unencrypted laptop is stolen from the car of a McKesson Automation employee.
Weird News Andy notes that California’s insurance exchange, Covered California, pulled down its online provider directory just eight days after go-live when the California Medical Association noted that obstetricians were labeled as ophthalmologists and doctors were incorrectly identified as speaking foreign languages. CMA also observed that some doctors were listed as exchange providers who didn’t actually sign up since insurance companies were permitted to add their in-network doctors to the list without their permission unless the doctor specifically opted out.
Staff and patients of Unit 5, the children’s cancer floor of the University of Minnesota Amplatz Children’s Hospital, create a video titled “Brave.”
Sponsor Updates
- SRSsoft hosts about 300 customers at its User Summit this week in Greenwich, CT.
- Sunquest and the Association for Pathology Informatics will offer an October 24 webinar on the topic of IT-driven virtual autopsies.
- Clinovations celebrates its five-year anniversary and highlights a few of its awards and honors.
- E-MDs integrates PatientPay’s online bill pay solutions within its PM software. The company will also integrate Phreesia’s point-of-care check-in solution into its EHR .
- St. Elizabeth Hospital’s (WA) use of e-form solutions from Access and hosted services from Inland Northwest Health Services helped the hospital meet HIMSS Stage 7 paperless requirements while eliminating the need for dedicated on-site hardware.
- Greythorn conducts a market survey for HIT professionals to analyze compensation, benefits, job satisfaction, hiring trends, and industry participation. Greythorn will donate $1 to the Boys and Girls Clubs of Bellevue and Chicago for every submission by November 20.
- Ed Bayliss, executive director for ChartMaxx, participates in a panel discussion on data exchange across the continuum of care at the eHealth Initiative 2013 Data Exchange Summit October 30-31 in Washington, DC.
- Humedica publishes a case study detailing how Mayo Clinic Health System prepared for value contracting using Humedica MinedShare.
- ZeOmega will embed Health Language technology from Wolters Kluwer Health into its Jiva care management platform.
- The Drummond Group certifies SRS EHR as a 2014 Complete EHR.
EPtalk by Dr. Jayne
You can tell that fall has arrived when every coffee vendor (including the one in the hospital lobby) is pushing pumpkin spice latte. Unfortunately, it is also the time I start sweating the fact that I need to come up with an extremely creative Halloween costume and come up with it stat. One of my favorite former bosses throws a massive party and the price of admission is a great costume. I enjoy Halloween immensely and have a closet full of costume options, but this party is peopled with brilliant individuals from academia, healthcare, and health IT so throwing on the Princess Leia braids simply will not do.
Maybe I’ll print a bunch of completely random attributes (some of which relate to me and some that do not) and go as my LinkedIn profile. I always laugh when people endorse me for knowledge of vendors I have never even heard of. I know several of the attendees are faithful HIStalk readers. Maybe I can convince my date to adopt a couples costume and we can go as Inga and Mr. H. Of course I could always go as Dr. Jayne, but that might be a little obvious. I guarantee at least one attendee will be wearing a bowtie and a Farzad-worthy grin.
The lobby of our medical school has a wall with pictures of our staff who have won various Nobel prizes. I could always dress as one of them and see if anyone picks up on it. Getting someone to identify that choice might be a little dependent on how far after the start of the cocktail hour I arrive, though, so not entirely a safe bet. I’m leaning towards possibly a World War I nurse just to have an excuse to purchase an awesome vintage cape. In medicine (and nursing) we used to dress more formally and I miss that. I understand that the current culture of scrubs is all about comfort and practicality, but I can’t help but think that if we dressed more seriously our patients (and administrators) might take us more seriously.
I took a course recently that covered communication and corporate culture. We did several exercises looking at how appearance plays a role in group dynamics. Watching several videos, we scored the characters based on believability, authority, seniority, and a host of other factors. Regardless of the scenario, those characters who dressed in traditional business attire scored higher than those who dressed casually. Besides dress, there are a lot of other factors at play with power dynamics, including the position of the participants (same height vs. seated/standing), tone, demeanor, etc.
I had the opportunity to rotate through a hospital in the UK during the late 1990s and was struck by the formality of the nursing staff. They still wore traditional dress whites (with caps) and nursing trainees wore blue. Physicians wore the long white coat and neckties. There were very few female physicians who I interacted with during my rotation, so I can’t particularly remember what they wore.
I trained at an academic medical center with an extremely traditional surgery department. Surgeons were never to wear scrubs outside the operating room. Trainees were not allowed to consume food or drink in the hallways – not even a sip of coffee – and white coats were to be fully buttoned at all times. Conversely, the OB/GYN house staff wore scrubs and sneakers 24×7, which created more than a few resentments. I wonder though if the patients or other hospital staff really perceived the departments differently? Was it a factor of dress code or of other factors that the dress code exemplified, such as discipline, order, and precision?
Scrubs and casual dress have become a way of life for most hospitals and medical offices. My hospital requires care teams to wear certain colors of scrubs depending on employee roles. Nurses wear navy, respiratory therapy wears light blue, patient care technicians wear khaki, etc. This seems to better help patients understand who is caring for them and what to expect. Unfortunately, physicians run the gamut between coat and tie and whatever scrubs they put on at the last hospital they rounded at. Some are so casual it’s hard to take them seriously. In response to a number of male physicians going sockless in loafers, one local facility created a rule requiring that “hosiery be worn at all times.” I’d like to have been a fly on the wall at the medical staff meeting where that was discussed: readmission rates, surgical site infections, ventilator-associated pneumonia, and bare ankles.
In the ambulatory care setting, the proliferation of scrub styles is mind boggling. We see a lot of “hip” medical assistants and patient care techs in low rider scrubs with flare bottoms that drag the ground to the point where they fray. I hope they never have to run to a code or crouch down to provide CPR, and if they do, that they have their waistband firmly in hand. One pediatrician I know has hand painted lab coats for every holiday and season. She’s the only physician on staff who wears a blue coat, so it really stands out. I smile every time I see her in the elevator, but I’m not sure what some of the patients and visitors think.
Generally I think the offices where staff dresses in a more uniform manner appear more organized and professional, but again maybe the dress code is a side product of management rather than a causative factor. Many of our offices provide staff with practice-logo polo shirts to be worn with khaki pants. This can be useful to reinforce an office brand as well as to help patients identify staff members, especially in busy offices with many ancillary services. That might be a great costume idea – maybe I’ll borrow a polo and masquerade as a staffer for a competitor practice.
I didn’t set out to write a fashion review, but perhaps Inga has been a greater influence on my writing than I previously thought. I could write an entire column on sassy patent leather hospital clogs, but we’ll save that for another night. I’m off to the internet for costume ideas. Got a great one? Email me.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.



















































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en