Top News

Nevada fires health insurance exchange contractor Xerox and announces plans to shut down its site, saying it will instead rely on Healthcare.gov for at least a year and then decide whether to spend many more millions to build a new exchange. The state has paid Xerox $12 million of the $72 million contract value and says the site’s many problems can’t be fixed by the next enrollment period that starts in November despite a personal promise from the CEO of Xerox. According to a board member, “We’ve seen so many broken promises from Xerox on how they’re going to fix it that at some point it just becomes not credible.”
Reader Comments

From Skeptic: “Re: Patrick Dempsey investing in CrowdMed. He made a big splash in Seattle about a year ago, coming in to ‘save’ Tully’s, a local coffee company. After incredible news coverage, he pulled out as an investor.” Dempsey ended up suing his investment partner, claiming that the owner borrowed money against the coffee company’s assets at an exorbitant rate without telling him. I think I would be cautious about bringing in a celebrity investor with deep pockets and high visibility, but also an ego accustomed to constant care and feeding.
From Jackie: “Re: HIStalk emails. Just wanted to say I love the new format with a snapshot of the article and the time it will take to read it. Great idea!” Thanks. I’m not doing it for news posts since those are broken out by category and therefore reading time isn’t as relevant since not everybody reads them all.
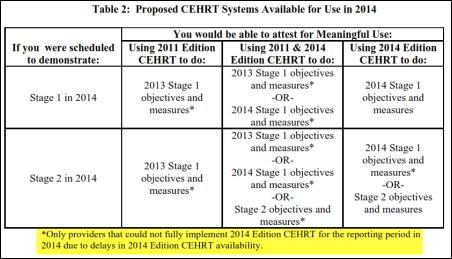
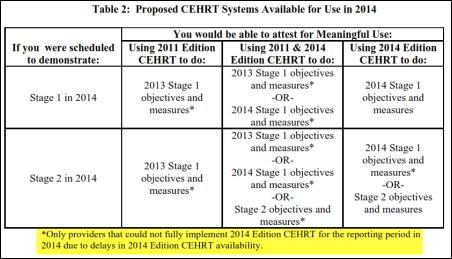
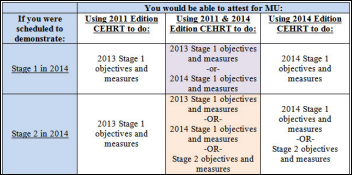
From MoreCowBells: “Re: new CMS rule. The press release includes the matrix you published, but not the asterisk and footnote. For Stage 2 sites, it makes a hug difference in what they will and won’t be able to do to attest.” Above is the footnoted version from the NPRM (highlighting mine), which seems to suggest that 2011 Edition CEHRT can be used in 2014 only if the provider’s EHR vendor hasn’t released a 2014 certified product. Lots of people are complaining about the proposed change for one reason or another, but the bottom line is that as long as providers plan to keep cashing HITECH checks, Uncle Sam gets to attach the strings. It also provides a lesson learned: if more than 20 percent of providers are moaning that they won’t be ready by a given federal deadline, don’t bother getting ready yourself because the date will be moved back.
HIStalk Announcements and Requests

Welcome to new HIStalk Platinum Sponsor Logicworks. The New York City-based company, founded in 1993, helps providers meet MU Stage 2 requirements to automate security risk analysis, address encryption and security of data at rest, and implement security updates. It offers an application-specific solution for NIST 800-certified cloud-based offsite disaster recovery for EHRs, with unplanned system failover with less than two hours of downtime. Its medical image archive and vendor-neutral archive for PACS breaks the never-ending cycle of adding storage capacity as imaging data grows. The company can help with application decommissioning as well, retaining legacy data in a cost-effective, HIPAA-compliant cloud. Logicworks also offers cloud solutions (public, private, and hybrid) and managed Amazon Web Services cloud hosting. As the company says, customers don’t come to it looking for a cloud, they’re looking for solutions for particular problems, and that’s what they offer. Thanks to Logicworks for supporting HIStalk.
I cruised YouTube to see what’s available for Logicworks and found this overview.
This week on HIStalk Practice: HHS representatives weigh the pros and cons of using Medicare data to alert public health officials to the potential needs of vulnerable patients during a disaster. Accountable Care Options and its physician network earn a $4.2 million bonus from CMS as part of its participation in the Medicare Shared Savings program. Oncologists list the pros and cons of moving from independent practice to hospital employment. A solo physician line items his reasons for closing up shop, citing meaningful use of an EHR as the final straw. Health systems and public health departments enter the new world of urgent care and retail clinics. The VA’s troubles show no signs of being swept under the rug. CMS and ONC publish a proposed rule that would slow down the MU program by extending Stage 2 through 2016. The government considers a national “biosurveillance” system that will give it near real-time access to the private medical information of citizens in the name of national security. Not all physicians stick their heads in the sand when it comes to online reviews. Thanks for reading.
This week on HIStalk Connect: As Apple’s WWDC nears, Dr. Travis speculates on how its anticipated new mHealth app Healthbook will work. Rock Health introduces its sixth class of startups that focus on ICU analytics tools, primary care telehealth, population health, and a private health insurance exchange. High school Junior Jack Andraka wins the Siemens We Can Change The World Challenge with a water purification text that is nearly 200,000 times cheaper than currently available tests, also having in 2012 won the Intel International Science and Engineering Fair with a new pancreas cancer screening test that is 168 times faster and 400 times more accurate than currently available tests. Mango Health raises a massive $5.25 million Series A round for its medication adherence app.
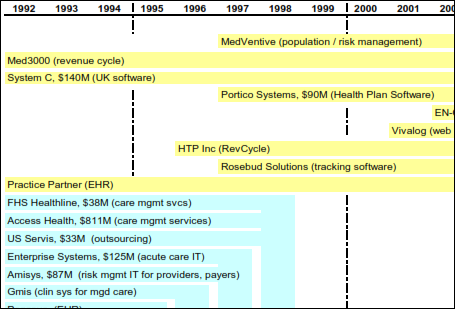
Acquisitions, Funding, Business, and Stock

Healthcare consumer marketing vendor Clariture gets $1 million in seed funding from Nashville VC The Martin Companies.

ZirMed acquires population health management platform vendor Intelligent Healthcare.
Sales

Marshfield Clinic chooses Strata Decision Technology’s StrataJazz as its integrated financial platform.
Community Care of North Carolina will implement CitiusTech’s BI-Clinical platform.

St. Joseph Health (CA) selects InterSystems HealthShare for its data sharing initiative.
People

AMC Health names Walter D. Hosp (HMS Holdings) to the newly created position of CFO.

Intelligent InSites names Shane Waslaski (Varistar) as president and CEO.
MEA|NEA appoints Mary Dooley (Xerox) as director of sales, partners, and channels.
Announcements and Implementations
Henry Schein Medical will offer athenahealth’s services to its customers as part of its ConnectHealth offering that includes Dell, Midmark, Siemens, and Welch Allyn.
Ping Identity announces Ping One, a mobile app for single sign-on for iPhone, iPad, and Android devices.
Government and Politics
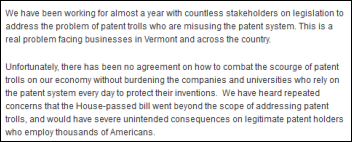
The Senate shelves the Innovation Act, a patent reform bill overwhelmingly approved by the House that would have made it harder for patent trolls to sue companies (most of them in the technology sector) using dubious patent claims. Senator Patrick Leahy (D-VT) removed the bill from the Senate Judiciary Committee, stating in his announcement that patent trolls are a real problem, but that the proposed bill would have imposed unintended consequences on legitimate patent holders.
Innovation and Research
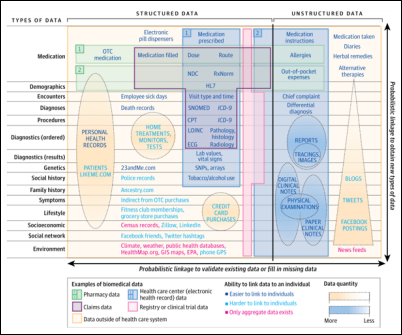
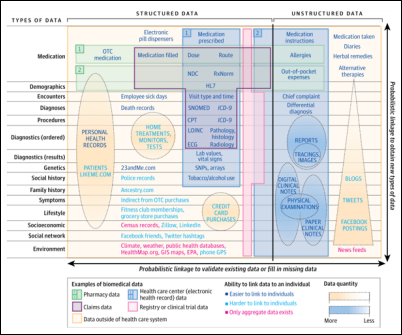
A JAMA opinion article on big biomedical data says that deep EHR information can be connected to broad data sources such as claims data, social media, and credit card purchase history to create a big-picture view of individual patients and their health risks. The problems are lack of a national patient identifier and privacy and security concerns. The authors are Harvard docs Griffin Weber, MD, PhD; Kenneth Mandl, MD, MPH; and Isaac Kohane, MD, PhD. I would think that a patient survey would find considerable discomfort with this possibility.
Other
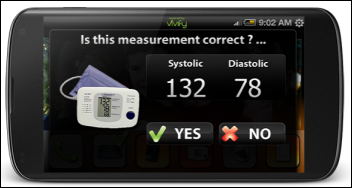
The Houston paper profiles Memorial Hermann Hospital’s Virtual Care Check program, in which discharged patients at high risk for readmission receive home visits and are monitored remotely via a scale, blood pressure cuff, pulse oximeter, daily questionnaires, and a tablet running software from the hospital’s partner Vivify Health. The hospital says the program’s patients are readmitted as low as 5 percent of the time vs. the national average of 12-15 percent. Memorial Hermann also announces the rollout of a free 24-hour RN-staffed Nurse Triage Call Center that anyone in greater Houston can call to ask questions or determine where to seek care, created after a study found that about half of Harris County ED patients could have been managed in a primary care setting.

Valley View Medical Center (AZ) loses its external phone connectivity and computer network for 11 hours after a Frontier Communications outage caused by a damaged cable.
Surescripts says that more than half of all eligible prescriptions in 2013 were transmitted electronically, with nearly three-fourths of office-based physicians using e-prescribing.
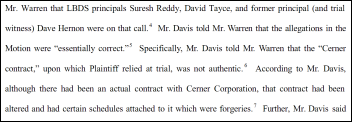
A law firm that had just won a $25 million verdict against a Korea-based medical imaging company withdraws from the case when its client, Texas-based cardiac MRI vendor LDBS, admits that a Cerner contract it introduced into evidence was falsified by using a fictitious email address. The CEO of LDBS had claimed he attended RSNA 2010 and saw the Korean company’s engineers demonstrating LDBS’s technology in a competitor’s booth.

A Reuters investigative report says that a grand Black Sea estate allegedly built for Russian President Vladimir Putin was paid for by skimming money from $200 million in inflated medical equipment contracts. The report names two people it claims bought medical equipment from Siemens and then sold it at inflated prices to the Russian government as part of a $1 billion healthcare modernization project, with $56 million of the money finding its way to Swiss bank accounts and then to the builder of the estate.
An AHRQ hospital survey on patient safety culture finds that while organizations are encouraging teamwork and organizational learning, more than half of respondents fear mistakes they make will be held against them, nearly half say patient care information isn’t communicated well when patients are transferred or during shift changes, and nearly half think employees are too overworked to provide the highest quality care.
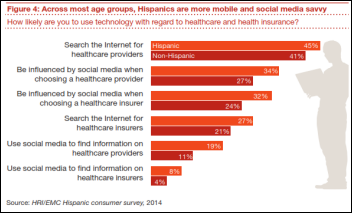
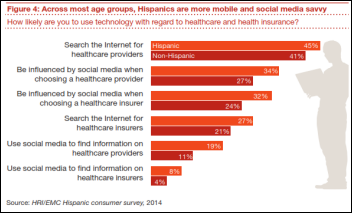
An PwC report says Hispanics will drive the US healthcare economy because: (a) more than 10 million of them will gain insurance through the Affordable Care Act; (b) they are cost-conscious; (c) they are heavy mobile users; (d) they don’t like sharing medical information; (e) less than half have a regular doctor and they don’t necessarily believe that the doctor knows best; (e) they will use retail clinics, community health clinics, and pharmacists to manage non-urgent problems; (f) they distrust the government and insurance companies and would rather see information in English since the translations are often poorly done.
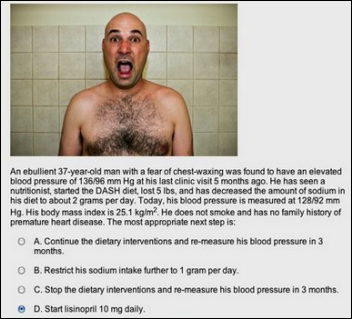
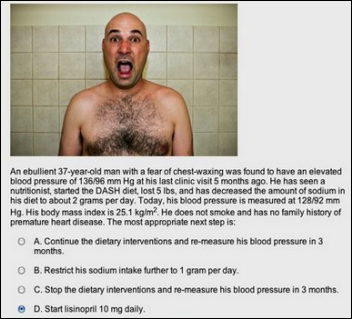
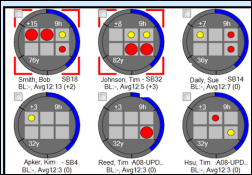
NPR profiles Qstream, a Harvard-created company that sends sequential emailed quiz questions to doctors and nurses to keep their education current. Eight Boston hospitals are testing a series of blood pressure questions that use bizarre stock photos and memorably silly cases to entertain and inform the recipients, who often compete against other using assumed names. Hospitals are posting leaderboards of the aliased participants, and as always happens with anonymized physician performance metrics, the always-competitive doctors have figured out who is who and where they stand among their peers.
Sponsor Updates
- HealthMEDX is rated as the #1 EMR vendor in the new KLAS report, “Long-Term Care 2014: Which Vendors Deliver on the Fundamentals?” with 100 percent of customers saying they would buy its product again.
- Forward Health Group CEO Michael Barbouche will speak at Connecting Michigan for Health June 4-6 in Lansing. He presented last week at the CEhp’s Alliance Industry Summit in New Brunswick, NJ.
- Nordic releases a case study on Baylor Scott & White’s use of its remote solutions offering for go-live support.
- DataMotion discusses current and future email regulations.
- Premier Inc’s safety expert Gina Pugliese joins The Physician-Patient Alliance for Health & Safety board of advisors.
- Kareo is selected as a 2014 Red Herring Top 100 North American award winner.
- GetWellNetwork clients experience a 76 percent improvement in pain well controlled as well as improvements in environment of care, medication teaching, heart failure readmissions, and falls.
- MedAssets announces that its 2014 Technology and Innovation Expo, to be held October 28 in Dallas, TX, is accepting applications for exhibitors.
- NTT Data commits three years of support for the North Texas Food Bank’s Food 4 Kids – Plano Program.
- OTTR Chronic Care Solutions will integrate XynManagement’s XynSiteTM suite of data analysis tool with its longitudinal patient tracking solutions and services.
- Nuance will add voice capabilities to Oracle mobile apps.
EPtalk by Dr. Jayne
As you would expect, the hot news in the administrative halls of our medical group this week was the play by CMS to again change the game for Meaningful Use. On the first pass, it looks like a benefit for providers, but I’m always skeptical until I look at the complexity of the details. Honestly, I tried to read the entire document (which at only 28 pages is nothing compared to the other Proposed Rules that emanate from CMS) but just couldn’t make it through.
I’m a TV junkie, so I was reminded of an episode of “Grey’s Anatomy.” One of the characters has a photographic memory. Some of the senior residents need information from paper charts to prep for their oral board exams, but they can’t take the charts to study them. They convince Lexie to try to memorize the charts and she starts, but partway through, she just snaps and her brain quits working. Another character makes a comment along the lines of, “You broke her.”
After today, I know how that feels. My boss expects me to be an expert on everything CMS within moments of its release. There is just no way to do so. CMS often conflicts itself (look at the FAQ evolution if you think I’m kidding) and delegates authority to a maze of regional contractors who each make their own de facto rules.
As a provider, I’ve had it up to here with CMS and Congress meddling in health care. If I was an independent physician, this would be the final straw that would convince me to opt out of Medicare and take my chances.
I’m a good reader, logical thinker, and smart enough to make it through medical school, yet I cannot begin to understand all of the regulations, especially when they start conflicting with each other. Our health system now employs a team of people to try to keep up with them and we can barely keep our heads above water. By extension, I can see no way (other than paying a fleet of consultants or going crazy) an independent provider can hope to play the game.
And that’s what it is — a game. Meaningful Use is just another fiery hoop for everyone to jump through. Since it’s all or none, you can work yourself to the bone, have everything right, but be thwarted by arcane rounding rules (don’t get me started) that will defeat you in the end. You can be defeated by patients who refuse to comply with your advice and have no interest in accessing their records. (I was visiting a practice today where nearly 80 percent of the patients refused their clinical summary documents or left them in the exam room.)
You can be defeated by the inability to get all the reports to run at the end of your attestation quarter if you’re trying to hit July / August / September. There’s no grace period – attestation has to be done by October 1 – so prepare for an all-nighter. If you have a power outage, you’re doomed. Hope there aren’t any hurricanes that weekend for our east coast readers trying to squeeze it in.
Anyway, we’ve all been through the angst of this for months and months, and now they’re going to probably change the dates again. We don’t know whether we can trust CMS. We don’t know how hard to work in the mean time – there is a 60-day window for commentary on the rule and no guarantees that it will be put into place unchanged – so essentially many of us are still on the hamster wheel whether we want to be or not. It’s discouraging, disheartening, and disrespectful to the many people who have worked so hard over the last year, only to have the end game change again.
I understand how we came to be here. I understand population health and the need to have big data. I understand the need to see vast numbers of patients to make sure everyone is served. I understand the need to coordinate care. But on the other hand, I understand the need to be able to spend my time just being a doctor – listening to patients, understanding their needs, and helping them get better. It seems that has been completely lost in all the noise and churn of regulations, guidelines, and rulemaking.
I’m not old enough to have practiced in the “olden days” of medicine when you could get away with writing a note that said “Sick – Penicillin” and charge $5 and be done with it. I certainly see the appeal however. I wonder if I could deliver primary care much cheaper if I went to the old-school approach? Without insurance or all the referral-chasing, I could probably slash my overhead by 80 percent. Without all the overhead, I could lower my prices. With lower prices and fewer distractions, I could help more patients. This is the heart of the direct primary care model, which is gaining traction in many communities. It’s an appealing proposition for more and more physicians.
A lot of providers who are learning to use electronic health records complain of being turned into data entry clerks or having to take on the duties that used to belong to the unit secretary. I initially went into IT and administration to help patients (and my peers) at a higher level. Unfortunately, I’m spending more time chasing federal rules, reading legislation, and trying to understand arcane documents than I ever thought possible.
Maybe I should have gone to law school after all. Maybe it’s just CMIO burnout. Maybe my brain is broken. Maybe I just need to get over it. But on the other hand, maybe we just need all these other entities to get out of our patient -physician relationships.
What do you think about the proposed changes to MU? Email me.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.













































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…