HIStalk Interviews Matt Zubiller, VP of Strategy and Business Development, McKesson
Matt Zubiller is vice president of strategy and business development for McKesson.

Give me some background about what you do at McKesson.
I’ve been with McKesson for about 10 years. I’ve held a variety of roles, both on the strategy side and the general management side. Most recently I was the general manager for decision support, InterQual, and the Clear Coverage business. Now I am responsible for the strategy for the McKesson Health Solutions business, which connects payers and providers.
What is the Better Health tour?
McKesson put on the Better Health tour with a variety of its customers and stakeholders. McKesson touches a lot of different people and customers. We brought pharmacists, payers, providers, diagnostics manufacturers, and technology companies together to talk about healthcare and what type of change is needed to move it forward.
We’ve done that across several regions–Portland, Boston, and also in Minnesota now. We are looking to bring together each of these different types of constituents to help them move healthcare forward and help be the change we want to see.
What kind of innovation are they talking about on the tour?
It starts with looking at the change. We as McKesson operate on an international basis, but healthcare happens very locally. Depending on the region you’re in, there are different problems that are being addressed.
They were macro issues, like the changing of reimbursement from volume to value. But also issues about how you help to move technology along, along with physician adoption. How do you help payers or a health systems collaborate more effectively with each other to help drive the inefficiency out of healthcare?
Can you describe what you’re seeing that’s interesting or what attendees are talking about?
They talked about a few models — particularly in Boston — that were interesting to us. There are technology innovators that we invited. We call them Edisons. They are the folks who are pushing both technology and different healthcare business models forward.
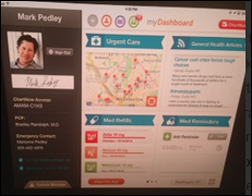
One example was a company called Iora Health. They contract with payers, providers, and primary care to provide primary care services on a fixed fee per-patient basis. That business model innovation is super interesting. When you use technology to support it, it becomes a lot more efficient and effective so you can track the performance of those patients.
Another example is some work that the Tufts health system has been doing. Tufts is a big health system, the oldest in the country, I believe. They had been looking across their region within the Boston area. They had contracted with and also connected to community hospitals so they could serve a much broader region of patients. You don’t have to have patients come in all the way into the Tufts health center to be able to be served. The community physicians themselves and the community systems can help support their patients.
There are several different ways we’re using technology to help break boundaries, but also to be able to shift business models.
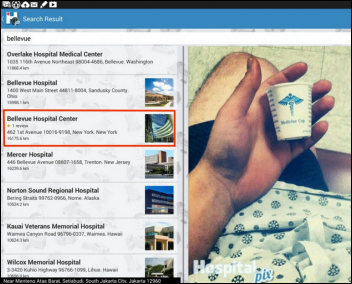
Jonathan Bush had an interesting thought in his book that part of the limitations of healthcare are geographic as well as driven by state-by-state licensure. In addition to telemedicine, he says hospitals should physically transport patients from long distances into their hospitals that perform high volumes of specific procedures, the focused factory model. What’s the potential of telling a patient in Boston that the best treatment for them at the best price might be in Ohio or Minnesota?
I think that is another factor as well. The walls are both regulatory and just the way we think about healthcare today.
Clayton Christensen was presenting at our innovation conference as part of the tour. He was talking about different types of innovation, both incremental and disruptive innovation. One of the things he has espoused is the fact that you need to provide the best care in the lowest-cost setting. I think that equally applies to your point, around the fact that care can be provided in one region or another depending on how efficient and how effective that really is.
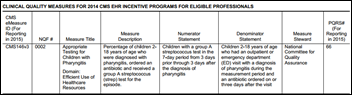
Part of the problem in healthcare — and this is something that also came up – is how do you effectively measure that? When you move from a volume-based model to a value-based model, where everybody’s talking about being paid based on value, how can you truly get to agreement around what value is? That’s a particularly difficult concept that the government’s trying to push forward with the ACA program, to begin to define different types of metrics.
But in the end, part of the wall you need to break down is not just understanding what good quality clinical care is, but what the financial decisions are that come along with it so you can begin to represent value.
I’ve worked in hospitals almost all of my career and we never told patients that another facility might be better at doing certain things. You worked in an area of McKesson that managed that data, so you could see it. Is it hard to convince patients that their local, shiny hospital that’s a source of community pride isn’t always the best place for them to seek care?
It’s an incredibly difficult sell, but I think it’s also generational. If you look at the generations who are a bit older, their fundamental healthcare relationship is based on that trust between them and their physician. If you look at some of the new generations, they’re beginning to not only question that, but they’re looking for the tools, as consumers in healthcare, to find the best healthcare at the best cost.
I think it’s incredibly difficult to bend that, but generationally we will probably end up getting there, even if it’s going to be 20 years from now. I prefer to believe we can use technology to accelerate that.
The big thing two or three years ago was medical tourism, with foreign hospitals marketing their Joint Commission accreditation, English-speaking employees, and luxurious accommodations. What happened to that?
I think medical tourism still has its place. I think that is still progressing forward. Telemedicine will help progress that forward.
What seems to be a big catalyst that’s going to be needed is this push towards value. It’s super hard to compare and contrast where can I truly get the best care at the best cost. It feels like medical tourism is still a bit of a novelty.
But when you begin breaking down these walls, if you can very clearly communicate to the patient, the consumer making that decision, what quality procedure they can receive with turnaround times and outcomes associated with it as well as cost, I think you’ll begin to see consumers demanding more of that information from the rest of the healthcare system.
Health IT startups usually claim they are innovative, but they are also often naive about the entrenched players and the difficulty in targeting an audience to make a sale or even get a pilot. What advice do you have for those companies?
Before I was in McKesson, I was both an entrepreneur and worked with a lot of entrepreneurs. One of the blessings you have as an entrepreneur is that you have wide-angle views, but also you don’t believe the obstacles in front of you are as big as they really are. I guess that’s the definition of an entrepreneur.
Healthcare moves slowly, more slowly than anybody else, because of all the constituents, stakeholders, and agendas that are involved.
Most folks who know of McKesson don’t immediately think that we are this incredible source of innovation. But it’s interesting in that I see a lot of pockets across McKesson in the various different constituents we have that we are innovating. But I think that we can do it faster. I think we can do it smarter.
That one of the reasons we put the tour together, to connect to those Edisons out there, those entrepreneurs who are thinking about new business models, who are thinking about overcoming the challenges that they see in front of them, and help us maybe get past, or in some cases, out of our own way. The partnership between the notion of the Davids and the Goliaths.
I guess you could argue that McKesson can very much seem like a Goliath in many ways. But if we can partner with those Davids out there who are going to eventually disrupt the businesses that we work in in a way that helps support the innovation, I think we can get what consumers need in the long run, which is more clarity around value, as well as being able to progress and change and adapt our business models before they get adapted for us.
What’s a good way for McKesson to work with those little companies?
We’re still figuring that out ourselves. We’ve tried the acquisition route before in the past. We’ve also tried the investment route before in the past, and we’re going to continue to evolve that over the course of the next 18-24 months as well with a couple of things that are coming out that we’re happy to talk with you about.
But one thing I’d throw out there is that we know that both on the outside and the inside that McKesson’s really good at scaling up, being able to take existing business models that have shown good promise and be able to provide both the technological support and the infrastructure and the scale to be able to blow it out to all the different stakeholders that are involved. And be able to do that while managing all the various conflicts.
For an entrepreneur, that’s really hard work. Not only that, it’s some of the most difficult work for them to try to pass through, because most of the time, entrepreneurs are starting new things and trying to grow companies, while the scale that McKesson brings is super important.
I think that there’s a nice pairing there, where people who are looking to start new businesses and be innovative can look at things in different ways, show how that works, and then McKesson can bring its scale and its process excellence, customer relationships, and network to help it grow quickly.
If you took the start-ups that have a paying customer or two, you would eliminate probably 90 percent of them. Assuming they’ve cracked the code and gotten that far into healthcare, what are the biggest potholes in the road that could cause them to fail?
One is time. Most of the time as an entrepreneur, you’re naturally also very aggressive around time. But in healthcare, the clock moves so much more slowly.
The ability to not only get customers on board, but to demonstrate results to show that you can actually improve costs or improve outcomes, is critical. Once you do that, you can scale. You have to address time. You have to be able to demonstrate outcomes and cost savings.
Once you’re able to do that, one of the biggest challenges that the entrepreneur has is figuring out how to break into the markets. Being able to get in front of payers, for example. Payers are obviously very busy and they’ve got a lot of things on their plate already. They tend to be somewhat siloed organizations. If you’re trying to get into a payer organization, you have to figure out how to leverage relationships to go do that.
That’s one thing McKesson can do, and it’s something I’ve seen myself. On the provider side, we obviously have relationships with thousands of health systems and tens of thousands of providers. That same issue — how do you break into the mindset of the physician when not only you but every other entrepreneur out there is trying to figure out how to get a hold of their attention to have them use your product or to be able to buy your solution?
It takes almost as much effort for an insurance companies other deep-pockets investors to do a little deal as a big one, so it may not be attractive to take a minority position or to invest in a small company. Is there a middle ground where they should look to someone other than a McKesson to help them get to the next level without giving away all of their equity?
I’ve seen a lot of experimentation out there. You see joint ventures that are happening because they’re a little bit less intensive in terms of taking equity away from the entrepreneur. There’s a shared upside on both sides, which is nice. There are a couple of organizations that are out there that are using that very well to their advantage.
There are venture funds that are being started by different organizations to support investments in those start-ups, which I think is also a good avenue depending on the level of engagement that the executives at that company have with those funds. That’s the real value the entrepreneur gets out.
If you serve a unique or specific niche or segment need, you can start with a simple partnership to demonstrate value and have the organization help you demonstrate that value. That can go a long way to the next step, be it a joint venture, a venture investment, or a potential acquisition down the road.
What do you see as the most likely area in which there could be true disruption versus incremental innovation, focusing on the technology side?
I look at technology as a great enabler of a disruption, but I don’t look at it as the source of the disruption.
As we move and shift our reimbursement system, it’s going to be a tremendous impact on our organizations. ACA, for whatever it’s worth, did many things. One of the things it did was expand access. It hasn’t done a lot around controlling costs.
I think you’ll see the next big change is going to be how to get our costs under control. Health systems have tremendous operating margin pressure. Health plans themselves are limited in terms of where they can reduce medical costs.
In the end, I think the shift in reimbursement model from a volume-based, fee-based model to a value-based model is where you’re going to see significant disruption. You’re going to see providers beginning to think about pushing volume out to lower cost settings. You’re going to see payers incentivizing providers and doing it in a way that’s clear.
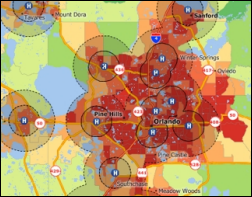
They’re going to need technology to do all of this, from population management — which is one of the thing McKesson is focused on — through risk management, through telemedicine, through connectivity. CommonWell is a good example — to be able to share data across different systems. Work we’re doing around decision support to both know clinically and financially what’s most appropriate at the point of care. Those are technological innovations that are going to stem from that business model disruption.
Do you have any final thoughts?
The tour is an exciting thing for us, but it’s just one part of the many things that McKesson is looking to do to drive and partner with innovators. Recognizing that we are a big organization that’s been around for a really long time, by working with those companies who have great ideas and those people who want to change healthcare for the better, the tour is just one good example of us trying to make that happen.






















































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…