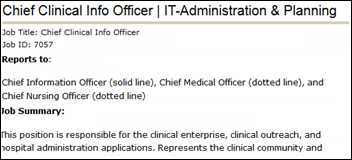
Davin Lundquist, MD is VP/CMIO of Dignity Health of San Francisco, CA.

What systems are you using on the ambulatory side and what are your priorities there?
In California, we have laws that prevent corporations from hiring physicians directly. The structure that Dignity Health primarily uses in California is a medical foundation. We have Dignity Health Medical Foundation, for which I practice at one of their sites in the Ventura market. Camarillo, California specifically. I’m a family medicine physician, a PCP.
In our medical foundation, which has about 600 physicians plus several hundred radiologists, we use Allscripts Enterprise for our ambulatory EMR. Dignity Health has nearly 40 hospitals crossing California, Arizona, and Nevada. We are moving to the Cerner platform in the hospital.
Outside of the foundation, we also have some employed medical groups in Nevada and Arizona. The large one in Arizona is using Allscripts Enterprise. Then in Nevada and a lot of our clinics that are not part of the foundation … many hospitals have community-based clinics. There’s a hodgepodge of systems that are being used there. We are in the process of looking to maybe consolidate or figure out if there’s an enterprise solution that we can roll out to all of those sites.
Are you having any challenges to tie in Allscripts ambulatory with Cerner inpatient?
In some of our markets, we’ve done a better job than in others with creating the integration. I would guess that a lot of health systems have this challenge of integrating data and having it be seamless. Integration tends to be very costly. There are issues around patient matching.
We have one of the largest private HIEs in the country. We use MobileMD, which was acquired by Siemens a few years back. We have nearly 7,000 of our physicians that have an account with that HIE. Primarily we’ve used that as a way for doctors out in the community to get information from Cerner, the hospital. Both the Cerner and the Meditech hospitals will feed data into MobileMD and then those physicians and offices in the community can access that.
Leveraging that integration platform, we’ve been able to, for our own providers that are on Allscripts, create a pretty good integration. A lot of our Allscripts providers in Sacramento will get automatically delivered to their Allscripts platform discharge summaries and radiology reports and labs and things that are done in the hospital.
Are most of the physicians attesting for Meaningful Use?
Yes. Of the providers who are on a system that is up to speed with Meaningful Use, we’ve had a nearly a 100 percent rate of Meaningful Use attestation. The clinics where we don’t run them from a foundation standpoint, then those doctors tend to work in clinics where he hospital staffs it, but the doctors are independent contractors. There’s a lot more variability there because a lot of those doctors may be specialists who have their own practice and just come in a few days a month. We believe a lot of them are attesting in their own practices.
Are you looking at any specific Meaningful Use Stage 2 challenges?
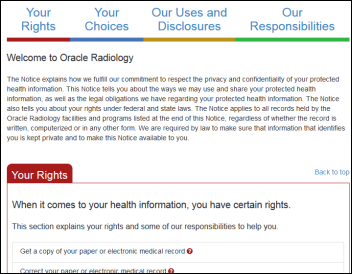
Yes. For Stage 2, the biggest challenge for us is the patient portal. We’ve been working with a company called Medseek to customize a portal for our Allscripts users. We’ve made a lot of progress, but there’s still challenges in getting patient enrollment, in getting doctors to feel comfortable sharing the amount of information that needs to be shared to achieve Meaningful Use. We’re still working through a lot of those issues, but we feel like we’re on a trajectory to make that happen by the end of the year.
Did you make that decision before Allscripts acquired Jardogs and FollowMyHealth? I’m just curious why you wouldn’t have chosen it.
We did. Without getting into the specifics, there was a very detailed RFP that went out and Jardogs was part of that. There were, I think, some specific limitations that Jardogs had, not necessarily related to function, but more around privacy and security and the way that Dignity Health approaches those things that I think made it incompatible with our setup. That was all pre-date of the acquisition by Allscripts.
Describe the pilot that you’re doing with Google Glass and Augmedix.
I practice in a clinic in Camarillo. We have several other primary care doctors there. We learned of the Augmedix solution. As you heard me describe some of the other technologies that we’re using at Dignity Health, you probably didn’t hear a lot of excitement in my voice. [laughs] I try not to reveal my true feelings.
Technology for physicians, while we understand and we know that it’s where we need to go, it hasn’t always been easy to adopt. If you talk to most physicians, they probably wouldn’t say that the EMR has made them more efficient. Again, I think we all understand that it’s important and having access to that data will eventually be more important.
The Google Glass technology was something that intrigued me. How is this going to impact healthcare? Where will this fall? You can imagine lots of potential use cases for it, but what we liked about the way Augmedix was deploying it, it seemed to be something that added value to physicians that would improve their ability to interact with patients, to do their job more effectively and not feel like they were getting bogged down with technology.
The way that it works is we wear the device as we’re seeing patients. The audio and video are being streamed to the Augmedix team. Through a combination of humans and technology that’s proprietary to them, the progress notes are being completed. As a practicing physician, the ability to feel like you’re getting back to that doctor-patient interaction has been a tremendous experience.
I assume they use some type of back-end speech recognition with human review and correction and that information is placed in the EMR?
I would encourage you to reach out to the Augmedix people and have them explain it to you. I want to protect their proprietary endeavors there. But I would guess that there’s probably some combination of human and technology going on there.
My experience would tell me that it has to be different than just voice recognition. You would understand this better than people that have interviewed me that when you use Dragon or even traditional dictation, you as a physician have to summarize the encounter for that voice-to-text to happen. In this case, Augmedix has partnered with us. They came and observed our workflow, observed the physicians that are using it beforehand, they met with us, they understood how we like to document, how we like to capture our physical exam and other things. They’re summarizing in real time for us. The true medical elements of that conversation are making it into the chart.
That’s not customized for each physician, right? It’s somewhat of a templated formula of how you speak to Glass to get it to understand what you’re doing at that point?
It’s not fully customized. I don’t want to imply that you can have it any way you want, but there is some customization. They do take time to learn how we like our notes to look. Also things like as I’m examining the patient, they can’t hear what I’m hearing, so I have to be able to communicate that to them in some way. Things like, if someone’s exam is normal, then in the absence of me verbalizing what I found, they may use a normal exam template that we agreed upon.
Then other times, if I miss something, one of the great and nice things about Google Glass is they can send me a little message that shows up on the Glass device and says, hey, you forgot to tell me what you saw in their ear exam. So there’s some two-way interaction that goes on.
Did Augmedix have to interface into Allscripts or did Allscripts have to participate in the setup to get your progress notes into their EMR?
Our version of Allscripts is hosted internally by Dignity Health. The Dignity Health IT team worked closely with Augmedix to sort that out. We ran everything through the privacy and security and compliance people so that the way it’s set up, everyone’s very comfortable with.
The release used the word “partnered.” There’s no financial interest either by you personally or Dignity Health with Augmedix, right?
Correct.
This is a three-physician pilot. What are the plans to roll it out further?
We’re currently looking in negotiations with Augmedix to expand to other physicians in Ventura. We’re excited about that opportunity. Then depending on how that goes, we may look to roll it other sites within Dignity.
What’s the patient reaction to using Glass in their encounters?
Overwhelmingly it’s been very positive. That’s definitely a question I had going into this — whether or not patients would accept it. I don’t wear glasses normally, so I was kind of curious what my patients would think of me wearing something like this.
One of the most surprising things is how many of my patients don’t even seem to notice. I think that probably has to do with patients coming in not feeling well or looking for help and focused on their concerns. When they come in now and see that I’m not typing, that I’m just sitting there, looking at them, waiting and listening and asking pointed questions about what’s happening — they almost don’t even notice that I have it on there.
There’s another group, obviously, that’s more tech savvy. They recognize that it’s a Google Glass and they’re interested in that because they haven’t seen one yet and they want to know what is it like. But even that, too, is a really short conversation. I explain to them what’s happening, that the information is being transmitted, and that this is helping us to document so that we can spend more time with them.
Across the board it’s been very well received. They even get a little excited about the fact that their doctor is using a new technology. It gives them confidence that we’re looking to whatever it takes to provide better care for them.
Are there still things in an encounter that you have to use a keyboard or a tablet for, or are there things that you would like to see added to what Augmedix can do to make it complete so that you don’t have to use any other device?
In this first phase, we still have to do our orders. We didn’t feel comfortable yet turning over the keys to that CPOE engine given that there’s a lot more important things going on there, like we should get the right medicine ordered, right labs ordered, those kinds of things.
Usually that happens at the end of a nice interaction with the patient, though, where we say, “OK, this is what I’m going to do for you.” That’s when I can turn and enter in some orders. But I think that’s a much more accepted thing for patients because they feel like they’ve had their time and now you’re actually doing something for them. When you do have to turn to your computer to do that, I think that’s an appropriate thing.
We are looking and hoping that as the technology matures, both the EMR and the Augmedix technology, that maybe at some what point we can verbalize those orders and that our voice can be recognized and authenticated. Who knows what that will turn out to be? But I am optimistic that we can push the limits of that.
Is it storing video or audio or both from the encounter?
At this point, no. I think our compliance people and everybody wasn’t comfortable with that yet, is my understanding. It’s an interesting thought, though. I think I saw an article recently where someone else was looking to maybe record video and audio right into a medical record, which I thought was an interesting concept. But we’re not doing that.
People always say technologies don’t preserve the patient’s story or the full richness of the encounter, so it would be pretty cool to say, “I want to see this whole visit over. I want to hear what I said, what the patient said.” That would be interesting documentation, although certainly there’s privacy and litigation concerns on both sides.
Absolutely. Once people feel comfortable that there’s technology out there that would really keep that safe, then I think we’ll move in that direction.
Dignity recently formed an accountable care organization. What lessons are you learning about the need for data and analytics tools?
ACO is kind of a broad term. There are several ACO-type contracts throughout Dignity Health in both California and Arizona. Some of them are more along the shared savings route and others are maybe more along just some metrics and other things. Clearly we understand the need for having access to data across the continuum of care. We need to be able to see longitudinal view of a given patient in order for us to really understand what it’s going to take to care for that patient and partner with them in helping them achieve their health goals.
What other projects are taking the most of your time and energy?
I’m working on projects with population health. We are looking to create what we call our population health management technology stack. You described the need for data — we’re looking at getting the data gathered for the first phase, then getting into the analytics layer, care management, what we do with that data, the clinical and patient portal-type interactions.
Related to pop health, we’re looking at collaboration tools, secure messaging tools, video visits … the list goes on and on. I think there’s probably a common list that you would hear from any big health system that is trying to anticipate what might be needed as we turn the corner on healthcare reform.
You’ll be buying and implementing quite a lot of systems over the next several years.
Yes. We are in the process of looking for vendors who, in some cases, have the maturity for us to buy them and purchase. But in most cases, especially in the population health space, we’re looking to either build or partner to co-develop solutions. I think it would be naive of us to invest too much money in a "solution" when nobody really knows what’s exactly going to be needed. We’re going to be very busy for a few years on that front.
Do you have any final thoughts?
I just want to say that I’m excited to be a part of Dignity Health. I’ve only been here for a couple of years. I came on at a really good time. I arrived right about the time that they were changing their name from Catholic Healthcare West to Dignity Health. I’ve seen a trajectory in this company that seems to really understand where things are headed, but not losing sight of the mission and value, this campaign around human kindness.
This particular Google Glass pilot and project has demonstrated that Dignity Health is willing to put their support and invest in projects that go in line with that. I’ve done a lot of technology stuff over the years, but this is one of the first that seems to excite every physician that comes around it, which is different from a lot of technology. I think the reason is because it really does get us back to why we got into medicine, which is that patient interaction, making a difference and feeling like you’re using something that’s more transparent and that is helping you as opposed to getting in your way.











































Traditionally Professional Courtesy is something that physicians gave each other - but we had to be careful with it when…