News 9/19/14
Top News
Apple removes HealthKit-powered apps from the App Store on iOS 8’s launch day Wednesday, stating that an unspecified HealthKit bug will keep those apps offline for at least two weeks. Some app developers are reportedly scrambling to remove HealthKit dependencies from their products to avoid loss of momentum.
I upgraded my iPhone 5 to iOS 8 Thursday hoping to fix an ongoing “no SIM installed” error. While the Health app is present, it only supports basic data entry (body measurements, sleep, vital signs) until connected to source apps, so nobody’s going to get excited about that. It does offer a new Medical ID option so that users can enter emergency information (allergies, meds, contacts) that can be displayed on the iPhone’s emergency dialer screen when needed. Reader Is-It-The-Future-Yet says that feature could have “more impact than anything HealthKit or the silly watch is going to do to actually impact care,” although my observation is that you would still need a medical alert bracelet since first responders aren’t going to check your phone on the off chance you’ve entered something important there.
From St. Louis Cardinal: “Re: BJC. Looks like they’ve gone out to the market for EMR replacement. Order of demonstrations: Allscripts, Cerner, Epic.” Demos were completed four weeks ago. I don’t remember what they’re using, although I know they chose several Siemens Soarian apps a few years back and I think they have some Allscripts products as well.
From MD Backle: “Re: Amazing Charts. Thought you might enjoy this email ad, in which they misspell EHR three times (twice as ERH, once as HER) plus misspell ‘it’s’ as ‘its.’ They need some proofreading!” Hopefully their programmers are better keyboarders than their salespeople.
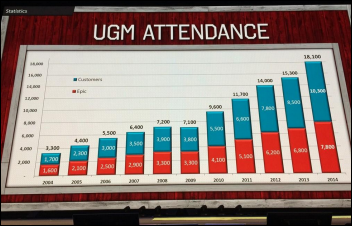
From A Reader: “Re: KLAS report on Epic consulting, released as hordes of consultants are at Epic UGM. It would be great to hear your input on the report.” I don’t have access to KLAS reports, so I generally don’t bother mentioning them since there’s not much I can say having read only the teaser press release that intentionally discloses little of the expensive report’s contents.
HIStalk Announcements and Requests
We’re already planning for HIStalkapalooza at HIMSS15 in Chicago. We’ve booked an amazing (huge) venue, hired a band, and started planning the details that will ensure that this will be the best and biggest HIStalkapalooza ever. Contact Lorre if your company wants to participate as one of five sponsors who will get great benefits like event recognition, a private hosting area, a welcome/display space on the main floor, and a bunch of invitations to share with prospects, customers, or employees. We needed to exert more control and decided to forego the “single sponsor” approach, although we might still consider it if a company agrees to our terms in making it a great experience for attendees. I like this approach (which companies have suggested for years) because the event’s sponsors can make a big impression in front of a huge audience without having to bear the full effort and expense.
This week on HIStalk Practice: One family physician sticks up for EHRs. Dr. Gregg provides perspective on Meaningful Use. Alisha Smith shares last minute prep tips for the HIPAA Omnibus deadline. Research shows Apple won’t reach critical mass for world healthcare domination any time soon. Elation EMR CEO Kyna Fong discusses the importance of physician shadowing. New Jersey Physicians ACO goes with eClinicalWorks. Brad Boyd offers strategies for onboarding financial systems. Thanks for reading.
This week on HIStalk Connect: Keas raises a $7.4 million Series C to help expand its employee wellness platform. 6Sensor Labs announces a $4 million seed round for a portable food analyzer that can detect gluten and potentially other allergens. Researchers at the European Respiratory Society’s International Congress present study findings suggesting that lung cancer patients have measurably warmer breath, a characteristic that may lead to innovative new screening tools.
Webinars
September 25 (Thursday) 1:00 ET. Using BI Maturity Models to Tap the Power of Analytics. Presented by Siemens Healthcare. Presenters: James Gaston, senior director of maturity models, HIMSS Analytics; Christopher Bocchino, principal consultant, Siemens Healthcare. Business intelligence capabilities are becoming critical for healthcare organizations as ACOs and population health management initiatives evolve in the new healthcare marketplace. The presenters will explain how BI maturity models can help optimize clinical, financial, and operational decisions and how organizations can measure and mature their analytics capabilities.
September 26 (Friday) 1:00 ET. Data Governance – Why You Can’t Put It Off. Presented by Encore, A Quintiles Company. Presenters: Steve Morgan, MD, SVP for IT and data analytics and CMIO, Carilion Clinic; Randy Thomas, associate partner, Encore, A Quintiles Company. In this second webinar in a series, “It’s All About the Data,” the presenters will review the pressing need for data governance and smart strategies for implementing it using strained resources.
Our secretive government health IT expert Dim-Sum delivered an amazing webinar Thursday on the Department of Defense’s $11 billion EHR project. We had large attendance and lots of questions in covering the EHR vendors and prime contractors that are bidding, the military health system’s structure, the opportunities for companies to do business as subcontractors, and the strengths and weaknesses of the competing teams (CSC-HP-Allscripts, IBM-CACI-Epic, Leidos-Accenture-Cerner, and PWC-GDIT-DSS.) It’s more like a conversation since we didn’t use slides, but it held my attention throughout and I highly recommend it to anyone with even a casual interest in how several billion of our taxpayer dollars will be spent or how our military members will be cared for. Thanks to the brilliant Dim-Sum for delivering a frank, funny, and highly useful presentation.
Medseek changes its name to Influence Health to reflect its mission to influence consumer choice, brand loyalty, and health behaviors before, during, and after healthcare encounters.

Larry Ellison will step down as CEO of Oracle. The 70-year-old company founder will be replaced by co-CEOs promoted from within, Mark Hurd and Safra Catz.
China-based Internet and e-commerce vendor Alibaba conducts the highest-yielding IPO in the history of American stock exchanges, raising $22 billion and valuing the company at $168 billion. The company made tentative moves into healthcare IT in the past few months with an investment into a Hong Kong-based pharma software vendor.
Perceptive Software, fresh off a move to a new headquarters building, announces layoffs and the closing of its offices in Beverly, MA and San Francisco.
Cerner gets Federal Trade Commission approval to acquire Siemens Health Services with early termination of the waiting period, keeping the acquisition on track for Q1 2015.
Central Clinical Labs selects Liaison EMR-Link to integrate lab results into the PointClickCare long-term care EHR.

Kaiser Permanente names SVP of Enterprise Shared Services Dick Daniels as interim CIO, replacing Phil Fasano.

Baptist Health System (AL) promotes CMIO Chris Davis, MD to CIO/CMIO. He has served as interim CIO since June.
Sunquest and Partners HealthCare establish a strategic alliance to develop a next-generation genomic information system. Sunquest will make an investment in GeneInsight, a Partners-owned company that offers software for genetic testing reporting, results delivery, and collaboration.
The Denver Office of Economic Development names Aventura as a Denver Gazelle high-growth company.

Holyoke Medical Center (MA) goes live on T-System’s EV physicians documentation system.
Dallam-Hartley Counties Hospital District (TX) implements Holon’s CollaborNet HIE.
Identity and access management solutions vendor Tools4ever will use technology from Boston Software Systems to automate its solutions.

High Point Regional Health (NC) begins its implementation of Epic, which will replace Allscripts outpatient and McKesson inpatient now that the health system has merged into UNC Health Care. According to High Point’s COO, “This is one of the main reasons we sought out and merged with UNC, that is, to be able to take advantage of centralized resources, and high on that list was Epic. For us, it’s a great opportunity because it is becoming the default, go-to system in the state.”

Congresswoman Renee Ellmers (R-NC) introduces the Flex-IT Act that would allow providers to choose any three-month quarter for 2015 Meaningful Use reporting, explaining,
Healthcare providers have faced enormous obstacles while working to meet numerous federal requirements over the past decade. Obamacare has caused many serious problems throughout this industry, yet there are other requirements hampering the industry’s ability to function while threatening their ability to provide excellent, focused care.
The Meaningful Use Program has many important provisions that seek to usher our health care providers into the digital age. But instead of working with doctors and hospitals, HHS is imposing rigid mandates that will cause unbearable financial burdens on the men and women who provide care to millions of Americans. Dealing with these inflexible mandates is causing doctors, nurses, and their staff to focus more on avoiding financial penalties and less on their patients.
The Flex-IT Act will provide the flexibility providers need while ensuring that the goal of upgrading their technologies is still being managed. I’m excited to introduce this important bill and look forward to it quickly moving on to a vote.

Mikey Dickerson, the former Google engineer brought on as administrator of the White House’s US Digital Service, says Healthcare.gov was a mess when he was called in to fix it as part of the “tech surge.” There was no system status dashboard, so “there was no place to find out whether the site was up or down except for watching CNN,” none of the project’s 55 contractors were tasked with maintaining uptime, and nobody seemed surprised or anxious that the site was down since government projects fail regularly. He explains his job change: “We have thousands of engineers working on picture-sharing apps when we already have dozens of picture-sharing apps. These are all big problems that need the attention of people like you. These problems are important, and fixable, but you have to choose to take them on. This is real life. This is your country.” I noticed that his LinkedIn profile lists his previous government-related service as “No Fancy Title, Thanks.”
The Portland, OR business paper profiles startup ReelIDX, which offers platform for creating, managing, and sharing medical video content. It emphasizes recording the patient encounter for patient education and clinician review.
Three North Carolina health systems – WakeMed, Wake Forest Baptist Medical Center, and Vidant Health – create a shared services company to reduce costs, with WakeMed’s CEO saying the systems hope to reduce their individual Epic operating costs and training efforts.
The Helsinki, Finland newspaper writes up “Apotti – a patient data system that costs more than a children’s hospital.” The government chose CGI and Epic as vendor finalists to develop the new system and expects to name the winner in early 2015. Total costs are estimated at $555 million.
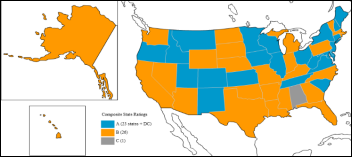
Does that graph help? "@CraigJoseph: Epic makes case that they should be recognized for interoperability. #EpicUGM pic.twitter.com/USYNDqhc9c"
— Farzad Mostashari (@Farzad_MD) September 16, 2014
This tweet from Epic’s UGM seemed to polarize the Twitterverse – do the disproportionate Epic-to-Epic numbers support or dispute Epic’s interoperability claims?
AMIA joins the Commission on Accreditation for Health Informatics and Information Management Education to develop accredit master’s programs in health informatics.

Faculty of the School of Biomedical Informatics at Texas Medical Center don hats to celebrate National Health IT Week.
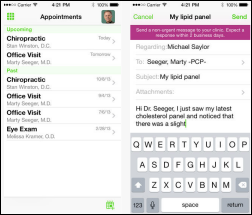
A clickbait Venture Beat article titled “EHR giant Epic explains how it will bring Apple HealthKit data to doctors” takes 16 paragraphs to state the obvious: user information from iOS’s HealthKit can be grabbed by Epic’s MyChart (with the patient’s permission) and then populate Epic. It misses the real challenge as to what happens on the Epic side, not only in the form of alerts or actions, but what clinicians are supposed to do as a result. The challenges aren’t technical:
- The data that an iPhone can collect is basic and not all that useful diagnostically except perhaps trended over time (such as a gradually increasing weight).
- Most app developers won’t get FDA approval to add logic that would find the one piece of potentially useful information out of thousands of data points, so that means tons of useless and unreviewed junk will get dumped into Epic.
- Providers aren’t paid to watch consumer-captured information. Even now patients could email their doctor with logs of weights, blood pressure, and blood glucose, but doctors aren’t paid to read them. It’s also not clear who should be watching the information – PCP, specialist, nurse, or someone else?
- Healthcare is designed around encounters, not monitoring. App developers don’t understand that medicine isn’t as digitally right or wrong as their world – most of us as patients want to be treated as individuals, not worksheets of measures limited by the convenient availability of sensors.
- Hospitals and practices may decline to allow patients to send them information since that accepts responsibility for doing something with it. Nobody wants to get sued for malpractice for missing one abnormal measure.

Steven Stack, MD, president-elect of the AMA, says EHRs are immature, expensive, and poorly designed. He adds that poor EHR usability is a significant driver of physician dissatisfaction. He doesn’t explain why AMA’s members greedily and voluntarily bought those systems despite their faults hoping to pocket a few dozen thousand dollars in free MU money. The market is where it should be, at the intersection of supply and demand, and perhaps the AMA should be convincing its members who are providing the demand as customers instead of scolding the companies that meet it. It’s like complaining that you hate Taco Bell while waiting in line to get your daily bean burrito. Stack has done committee work for ONC, was involved with the PCAST Report (that mostly touted Microsoft as the answer to all healthcare IT problems), and is on the board of eHealth Initiative (which includes quite a few vendor members). He’s always been a usability critic.
At least 15 children die in Syria after receiving UN-provided measles vaccine, with a preliminary WHO report speculating that medics accidentally gave the muscle relaxant atracurium instead of the vaccine since the drugs are packaged in similar vials and were stored in the same refrigerator.
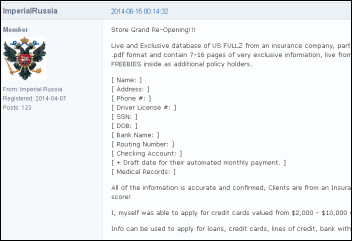
A security publication finds medical records on sale in bulk on a black market Internet site, apparently stolen from a Texas life insurance company’s applicant database. The writer bought records and verified their accuracy, with prices as low as $6 for each “fullz,” slang for a complete set of records that the buyer can use to open fraudulent credit card accounts, access bank accounts, or take over someone’s identity.
UCSF surgeon Wen T. Shen says he’s embarrassed for patients to see his lack of typing skills, but doesn’t like the alternatives:
Wait until after the patient leaves to start charting (impractical given our clinic workflow); hire a medical scribe to do my documentation for me, as detailed in a recent New York Times article (not happening with recent budget cuts); use the nifty speech-to-text dictation device provided to all clinicians (feels extremely weird and off-putting to do this in front of patients); actually learn to type (old dog/new tricks, dwindling brain plasticity).
Weird News Andy says, “I <3 this password,” although he adds that it might be tough to get into your phone to dial 911 during a heart attack. Researchers develop an authentication method that uses wristband-detected ECG patterns as “the perfect password,” although people with fibrillation might not be ideal users.
- Nordic announces that it has earned the top ranking among Epic implementation support and staffing consulting firms in a new KLAS report. Also named in the report is Orchestrate Healthcare, the highest ranked vendor-agnostic consulting firm in the implementation support and staffing category.
- ADP AdvancedMD’s EHR earns ONC-ACB certification as a Complete EHR.
- Huntzinger Management Group recognizes its clients and IT professionals for National Health IT Week.
- Access provides Normal Regional Hospital (OK) with giveaways to help celebrate National Health IT Week.
- EClinicalWorks names several ACO clients that are generating savings after deploying its CCMR.
- ESD’s Phil Sierra discusses the value of healthcare IT in a recent blog.
- Etransmedia shares a video about its success and growth.
- SRSsoft is participating in the American Society for Surgery of the Hand conference in Boston this weekend.
- Truven Health Analytics and National Business Group on Health partner to facilitate an improved Employer Measures of Productivity, Absence and Quality program.
- AirWatch by VMware offers instant support for devices running on iOS 8.
- An Imprivata survey finds that 65 percent of hospitals will use Virtual Desktop Infrastructure within two years and 84 percent of those will add single sign-on.
EPtalk by Dr. Jayne
The physician lounge was buzzing this morning with the news of HR-5481, the “Flexibility in Health IT Reporting Act.” If passed and signed into law, it would allow providers to report 90 days rather than a full year in 2015.
I have to say my pulse quickened when I saw it. Congress set precedent with their ICD-10 push. This one might have less of a chance, however, since it’s not being tacked onto another high-profile bill. Maybe we can hook it to a bill everyone can get behind, such as the “We Love Mom, Apple Pie, and America Act.” If this passes, it just might defibrillate Meaningful Use, moving it from “mostly dead” to “slightly alive.”
In other bandwagon-jumping news, the American Medical Association releases a paper on setting “Priorities to Improve Electronic Health Record Usability.” I’m not a big fan of the “blame the EHR” game since there are so many more factors that influence usability, user behaviors, and generally how the health system runs. Rather than putting all of our eggs in the proverbial basket and assuming that if we just “fix” the EHR everything will be awesome, let’s look at the other issues that cause slowness and waste in health care.
My laundry list includes E&M Coding, obnoxious precertification requirements placed on physicians without good reason, The Joint Commission requirements, RAC audits, payer audits, Meaningful Use, other certification body requirements, and numerous non-value-added steps throughout the day. I could go on, but it would be aggravating. Although some of these have been shown to improve outcomes, many are just nuisances. Let’s take a multi-pronged approach and stamp out ALL poor usability, not just that of the software variety.
Back to the AMA, they again sent Medicare reimbursement codes for end-of-life care discussions to CMS for consideration. I’m in favor of efforts that would actually help physicians be paid for non-procedural work. We don’t die well in the United States. TV and media paint a picture of heroic lifesaving measures where everyone recovers fully, but don’t ever show patients with poor outcomes. The last time this came up, the scare tactics around “death panels” crushed any hope of approval.
As a primary care physician, one of the best things I can do as part of our partnership is talk to you about end-of-life care, getting your wishes out in the open and ensuring you have a support system that can carry them out when the time comes. Unfortunately, this isn’t for just Medicare patients. We need a national dialogue (heck, our EHRs all have prompts for it anyway) for patients of all ages. Young women die in childbirth, people are in horrific accidents, and overall stuff just happens.
I had some nurses make fun of me when I rolled into an outpatient surgical procedure with my healthcare power of attorney and living will at the tender age of 31. As a physician, I don’t want “everything” done and am firmly convinced there are things worse than passing on. Unfortunately, there’s no way commercial payers will cover this service until Medicare takes the lead or until patients pay out of pocket.
Until then it’s just one more thing we have to do without compensation, like keeping your diagnosis list maintained in both SNOMED and ICD-9 and explaining ethnicity to elderly people who have no idea why we would need to gather that type of information. I’m expected to share all data, but patients can pick and choose what I see, potentially placing them at risk. Proponents of MU argue that the potential of up to $44K worth of incentive payments effectively compensates us for all the extra work, but it doesn’t even scratch the surface.
I’m interested to hear what else we should ask Congress to fix for us while they’re at it. Got an idea? Email me.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.


















































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…