Top News

Healthcare analytics vendor Inovalon Holdings (known until a 2012 name change as MedAssurant) files for a $500 million IPO. The CEO and board chair is cardiologist Keith Dunleavy, MD. The company’s technology is used by NextGen, Greenway, Allscripts, and Walgreens.
Reader Comments

From KimJongDeux: “Re: Athenahealth. Interesting that Jonathan was the much celebrated, drunk, foul-mouthed (and most un-funny) host of HIStalkapalooza for a few years and the article above seems to indicate the bloom is off the rose. Guess he’s not on the program this year? We seem to have a company run by force of personality. The quote, ‘Those naysayers don’t understand the company’s business model’ is the same cry as we hear from self-styled ‘artists’ when their works are panned and from CEOs who either get no push back from their yes-men staffs or who weeds out or banishes anyone who disagrees. The fact that their corporate meeting involves officially sanctioned heavy drinking games tells me all I need to know. And the fact that the CEO openly supports it as a good thing is troublesome. I agree that if the force of personality ever left, the company would fold like a house of cards. Being brash, loud, and verbally overpowering others can keep the airplane aloft only so long.” The company has a new logo and website, I’ve noticed, moving away from the squint-inducing yellow and green color scheme to a more serious-looking purple and green.

From PM_from_Haities: “Re: Epic’s going public. It would have very little effect. The capital structure of a company (i.e. going from private to public) impacts who owns Epic, but it’s leadership would likely be unchanged. Given Judy has plenty of cash, it would make very little sense for her to add that kind of public scrutiny unless it helped in gaining government contracts. Epic would continue to deliver on its promises and continue to grow. If anything, Epic might get BETTER by being publicly traded as they would typically have a stronger marketing department.”
HIStalk Announcements and Requests
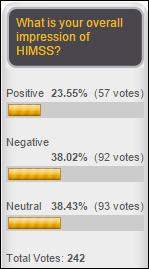
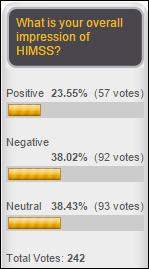
One-fourth of respondents to my poll expressed a positive impression of HIMSS, with 38 percent each having neutral or negative feelings. New poll to your right or here, triggered by last week’s Fortune article: which set of quotes best describes Athenahealth, the positive ones by CEO Jonathan Bush or the negative ones from a skeptical hedge fund manager? Vote and then click the “Comments” link in the poll box to explain yourself.
Attendees of our webinars have asked about the possibility of receiving continuing education hours. I looked into this years ago and concluded that the only way to accomplish that would be to connect with a university already set up to award CEUs to physicians, nurses, and pharmacists. I’m open to suggestions.
I registered for the HIMSS conference this weekend since the early full registration rate of $745 is good through January 27. My impressions:
- The online registration is slow because it tries to upsell you on extra-cost events, but it’s efficient otherwise.
- The registration policies document says that HIMSS doesn’t share attendee email addresses and to report any email received from an exhibitors. I assume that means that, as usual, registrants will receive a barrage of promotional snail mail (some of it invariably arriving after the conference has concluded).
- The registration policy references a “use of photographic images” clause in the same document, but the only related item involves “recording any educational session content,” so apparently the widely ignored ban against taking exhibit hall photos has been eliminated.
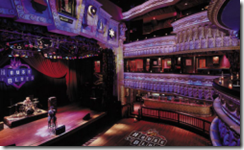
Divurgent, Elsevier, Falcon Consulting, Sunquest, and Thrasys have signed on as sponsors of HIStalkapalooza, which will be held Monday of the HIMSS conference week at the House of Blues Chicago. It’s an expensive event to put on — the facility, food, bar, and band add up to more than $175 per attendee — and the number and level of sponsors dictates the number of people I can invite (and thus the number I can’t invite) without going deep into the red. We still have a couple of weeks to add new sponsors – let me know if your company is interested in standing out among all the conference noise that week.
Last Week’s Most Interesting News
- An report looking at six ONC-funded state HIEs finds that large health systems can be either supporters or competitors, HIEs are beginning to embrace Direct despite its poor EHR integration, and the HIEs are still searching for use cases that the market wants.
- A Wall Street Journal report finds that a significant portion of Medicare fraud is perpetrated by the 45,000 newly registered providers each month that CMS says it doesn’t have the resources to review.
- CSC pays $190 million to settle an SEC fraud case that includes its UK NPfIT contracts.
- A Fortune profile contrasts Athenahealth’s high-flying public image with the skepticism of investment advisers and managers who say the company’s tiny market share and flattening performance suggests otherwise.
Webinars
January 13 (Tuesday) 1:00 ET. “The Bug Stops Here: How Our Hospital Used its EHR and RTLS Systems to Contain a Deadly New Virus.” Sponsored by Versus Technology. Presenter: John Olmstead, RN, MBA, FACHE, director of surgical and emergency services, The Community Hospital, Munster, Indiana. Community Hospital was the first US hospital to treat a patient with MERS (Middle East Respiratory Syndrome). It used clinical data from its EHR and staff contact information from a real-time locating system to provide on-site CDC staff with the information they needed to contain the virus and to study how it spreads. Employees who were identified as being exposed were quickly tested, avoiding a hospital shutdown.
People

OB/GYN EHR vendor DigiChart promotes Rodney Hamilton, MD to president and CEO.
Announcements and Implementations
Terrebonne General Medical Center (LA) goes live in its admissions area on RightPatient facial recognition software from Atlanta-based M2SYS Technology.
Government and Politics

The New York Times profiles US CTO Megan Smith, with insiders concluding that while she has a big vision and the president’s ear, she’s also in a position that comes with unclear mandates, minimal budget, and responsibility for outdated technology platforms. The article points out that the newly created United States Digital Service reports to the Office of Management and Budget instead of her office.

A class action lawsuit filed by doctors against North Carolina’s Department of Health and Human Services over software that incorrectly paid practices Medicaid rates for services provided to Medicare patients lingers on a year later. A family practice doctor says the state owes him $100,000, adding that in his pleas to DHHS, “There was a complete lack of courtesy. Those people have no humanity.” The NCTracks system was developed by CSC at a cost of $484 million, with a significant portion copied from a similar system CSC built for New York City. The US Justice Department sued CSC and New York City in October for Medicaid fraud, claiming that the $1 billion New York system didn’t correctly bill Medicaid secondarily to private insurance. Neither system was related to CSC’s $190 million settlement with the SEC last week over accounting and fraud claims involving the company’s work on the UK’s failed NPfIT project.
Oregon’s proposed 2015-2017 budget includes $3 million for a prison system EHR, which is expected to go live in early 2016.
Privacy and Security
The US Postal Service announces that a previously reported breach of its systems that exposed the Social Security numbers of 800,000 employees also included medical information on 485,000 current and former employees as well as retirees who had filed for worker’s compensation. The most interesting aspect to me is the huge number of injury claims filed with USPS.
Technology
I mentioned last week that John Olmstead, who runs the ED and surgery departments of The Community Hospital (IN), says in an upcoming Versus webinar that he would like to see a GPS-wayfinding type technology so that hospital visitors could navigate around campus using their smartphones. Readers sent information on two companies that offer such technology:
Connexient offers a smartphone app that provides turn-by-turn navigation to visitors at Robert Wood Johnson University Hospital and will bring six more hospitals live on it in the next few months.

Madison, WI startup Solomo Technology is using similar technology to help conference attendees locate session rooms. It offers APIs so that developers can integrate its location and content services into their own apps.
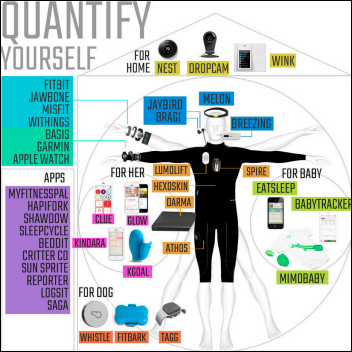
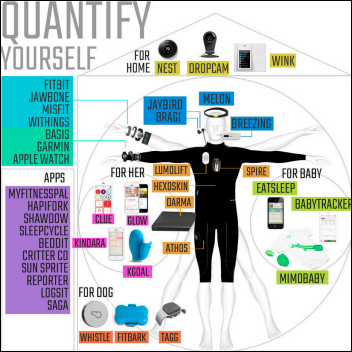
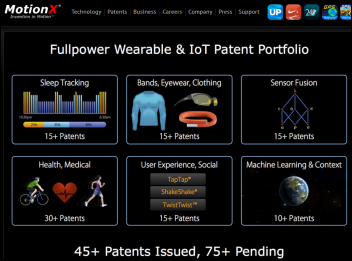
An excellent analysis of the fitness tracker market makes great points:
- Courts are beginning to accept fitness tracker data in cases ranging from vehicular accidents to worker’s compensation, with resulting privacy concerns.
- Wearable device manufactures use glossy marketing to position themselves as health and wellness brands instead of step counters. “You will never find a review for Jawbone or Fitbit that says ‘works as advertised’ because no one knows what they’re advertising.”
- Trackers have penetrated only 3 percent of the market and the washout rate is high.
- The Scanadu medical tricorder-type device holds great promise, as does senior monitoring app Lively.
- Companies that have bought a single brand of fitness tracker for employees haven’t seen broadly successful results because people are motivated differently.
- Users don’t want more data, they want to have devices tell them what to do and to simplify their technology interactions rather than to add new ones.
Other

This headline from the Rome, GA newspaper succinctly describes a lot of what’s wrong with the US economy. Taxpayer-funded organizations that don’t pay taxes themselves shouldn’t be the only hope of employment growth. At least government hiring didn’t top the list.

The Madison newspaper profiles Nordic Consulting co-founder Mark Bakken’s transition from entrepreneur to venture capitalist. He’s putting together a $10-$20 million venture fund that will invest $300,000 to $500,000 in Madison-area companies whose technologies work with Epic. He has raised $4 million so far (including $1 million of his own money) and says several Epic-using health systems have expressed interest in investing. The article mentions that he has personally invested in eight startups (Catalyze, Forward Health Group, Wellbe, Moxe Health, 100health, Quietyme, Healthfinch, and HealthMyne) and four of those have hit $1 million in annual revenue. Bakken, who stepped down from the CEO role at Nordic last month but remains board chair, says he “won the lottery with Nordic,” which had $81 million in revenue in 2013.

A fundraising project for the children of The Johns Hopkins Hospital senior software engineer and bike shop owner Tom Palermo that included a 1,000-participant New Year’s Day ride has raised $60,000 so far, well beyond its original goal of $10,000. Palermo, 41, was killed last weekend when he was run over while bicycling by an Episcopalian bishop with a previous drunk driving arrest who fled the scene. She has been placed on administrative leave pending possible criminal charges following her admission that she hit Palermo, who leaves behind his wife, six-year-old daughter, and four-year-old son. The bishop had previously received probation for her 2010 DUI arrest (before she was hired by the diocese) in which she was driving a car with a tire shredded to the rim, told police she had drunk alcohol and smoked marijuana, and recorded a 0.27 on a blood alcohol breath test.
Five Michigan health systems receive $25 million in value-based payouts from Blue Cross Blue Shield of Michigan, which says the hospitals and physicians are communicating better because of EHRs and HIEs. The systems will also receive $500,000 each over three years to improve their IT systems and care coordination. The chief medical officer of Henry Ford Physician Network says he gets immediate notification if his patient is is seen by any provider in the network or at an area hospital that uses Epic, but otherwise he won’t know about it until he sees the patient next, so he’s looking forward to using the money to improve HIE connectivity and to improve data capture from physician practices.

Lenox Hill Hospital (NY), embarrassed by international press coverage of a British couple unfortunate enough to have their premature baby delivered in the US at a cost of $200,000 instead of free in England, hints that it will simply write off the bill, sticking less-publicized patients with the burden of its profitability. It really annoys me that when media outlets publicize a ridiculous hospital bill involving a feel-good patient, the hospital nobly agrees to cancel the bill as though it doesn’t really need the money. The rest of us who get equally absurd hospital bills are turned over to collections for every dime. Somehow the public never sees through this PR scam to realize that we’re all paying for it. The same hospital annoyed patients and families three years ago by restricting visitor access so that Beyonce and Jay-Z could have their baby in the manner to which they have become accustomed, with the star couple adding their own private security force to guard the VIP suite (the hospital denies rumors that the couple spent $1.3 million to upgrade their room). The CEO of North Shore-LIJ Health System, which owns the hospital, was paid $4.3 million in 2013.

The Sioux City paper describes the interoperability situation between UnityPoint Health – St. Luke’s and Mercy Medical Center, running Epic and Cerner, respectively, and still faxing scanned chart images back and forth. The hospitals are bringing up Iowa Health Information Network with hopes of electronically exchanging at least summary records.
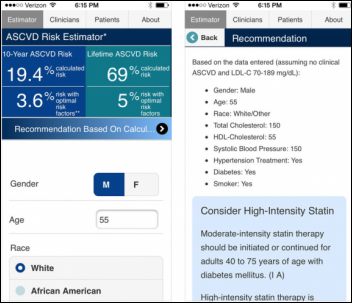
Tennessee doctors are diagnosing and treating people with flu by telephone or telemedicine, telling them not to come to the office for fear they’ll spread the virus to other waiting patients.

A ProPublica investigative article exposes the billing practices of the for-profit debt collection agency run by non-profit health system Mosaic Life Care (MO), which has filed 11,000 lawsuits in five years to collect money from uninsured hospital patients and to garnish their usually low wages. The part of the story that always drives me crazy: uninsured patients are sued for the full (phony) list prices hospitals make up in order to give 90 percent discounts to insurance companies, so people are losing their homes to pay for $12 Tylenols and the ever-accruing interest charges and attorney fees. It seems reasonable that hospitals be required to charge cash-paying patients their lowest prevailing contracted prices.
A JAMA opinion piece written by informatics people from Christus Health points out the rising numbers of medical scribes, the number of companies (22) offering their services, and the creation of a scribe aptitude test and a vendor-led member association. It says that overuse of scribes to make up for EHR inefficiency can lead to compliance and clinical issues, concluding:
The answer to today’s inadequate EHRs is not scribe support. Instead, physicians should demand improved products, should educate vendors to ensure that they understand how physicians think clinically, and should clarify what is needed for an intuitive, quick, and navigable user interface. If such usual market forces are vibrant, and physicians engaged robustly, EHRs will evolve rapidly. Yet even after a decade of use, some EHRs and CPOE may not compete with the speed of a paper checklist, and may never.
The New York Times notes that a doctor whose office was raided by federal agents for writing oxycodone prescriptions for $200 in cash was caught only because neighbors complained about the traffic outside his unmarked office that was guarded by an armed bouncer. The doctor made $2.6 million in cash over two years writing narcotics prescriptions to patients who then turned the drugs over to “crew chiefs” to sell on the street. The practice created false medical records that included MRI reports and urinalysis results.

Dr. Oz makes a lot of headlines, most of them negative. His ABC TV show, “NY Med,” takes heat when a female viewer watches her husband die in an episode filmed at New York-Presbyterian Hospital without the family’s permission. Producers blurred the man’s face in the video, but the woman recognized him and heard his last words as the cameras rolled. Her son has filed complaints with the hospital, the state’s Department of Health, and HHS’s Office for Civil Rights. The hospital and ABC claim the patient isn’t identifiable, ABC says news is protected by the First Amendment, and the hospital says the man’s privacy rights ended when he died and blames the family instead for calling attention to his identity by complaining.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.











































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…