Michael Jefferies is vice president of information systems at Longmont United Hospital of Longmont, CO.

Tell me about yourself and the hospital.
I started off as an intern way back when with McKesson. I started with their support center, answering the phones and doing support tickets. That grew into doing technical administration work. I had my roots in technical work and then grew into business leadership and started doing some outsourcing and consulting work with ACS Xerox. From there, I felt strongly that I’d like to get closer to the delivery of care.
T hat’s how I found myself at Longmont United Hospital. The hospital is a 201-bed facility. It’s a community, not-for-profit hospital Longmont, Colorado, which is in Boulder County.
As someone who previously worked for McKesson and is now a Horizon customer, how has the company handled the Horizon product and trying to get its users to migrate to Paragon?
I have a lot of respect for McKesson as an organization. I got my start there and they have some wonderful people working there. The Horizon product got its start as a startup in Boulder. It was a great product to start. It grew organically in some great ways.
As McKesson rushed to be first to market with a comprehensive, integrated solution, they used an acquisition strategy, which led to not achieving that goal of having an integrated product. While they were first to market, they came to the conclusion with their Better Health 2020 announcement that the acquisition strategy created technical, geographic, and personnel challenges. Making an integrated product through an acquisition strategy was not a feasible way to go about it. That was unfortunate because it was a product that early on had great promise.
I would agree with their decision that they’ve made in Better Health 2020. It was no longer an integrated solution. They were right to shift their strategy towards an integrated solution.
I’ve had the fortune of being a product manager and leading the implementation of the Paragon solution, It was a KLAS market leader for smaller community hospitals. They had good satisfaction. For a lot of customers, it was their first EMR.
The idea of trying to get folks that were Horizon customers with higher expectations to move to the Paragon product was premature. It was something that most of the customers did not see as a feasible solution or alternative. That’s what you’ve seen. The vast majority of Horizon customers have gone elsewhere.
The other thing working against Paragon is that the healthcare market, due to other forces, needs economy of scale. You’ve seen a huge consolidation in healthcare. That consolidation has favored EMRs that can handle a large scale, which in our market means Cerner and Epic. When a larger organization consolidates smaller hospitals and organizations, they certainly aren’t going to uptake that smaller community EMR. They’re going to continue to deploy Cerner and Epic. That has contributed to their market dominance.
Do Paragon and Meditech have significant problems that would prevent them from being successful in large academic medical centers?
Yes. Paragon right now doesn’t have an ambulatory solution, so people that are making the jump to Paragon right now are putting faith into that product developing into a comprehensive solution. Their ED product is brand new and their ambulatory product does not exist yet. That’s a major limitation for Paragon right there.
With Meditech, they’ve made some great changes in strategy recently. They’re very strong in the market. But a colleague accurately described Meditech as, “The EMR that your materials management department would choose.” It hits all the checkboxes on everything you need, but when it comes to the end user experience, there’s something wanting there. They’re a great organization, they fill a market niche that is needed, and they are moving in the right direction with listening to their customers. They have a lot of great really satisfied customers as well.
Will Athenahealth be able to compete with Cerner and Epic via its RazorInsights and BIDMC WebOMR acquisitions?
I would love to see that. Athenahealth’s approach to the private practice or ambulatory market has been that customers want to be health providers, not IT organizations. We’re not in the IT business, we’re in the healthcare business, and I think Athenahealth supports that. Their fundamental makeup gives them the chance to make a run for it. Now if they’re actually going to be successful — that’s yet to be seen. I would love to see a different competitor come in because we know that while Cerner and Epic are dominating the market, they each have their own blights as well.
What are the most important initiatives that you see happening in your hospital over the next several years?
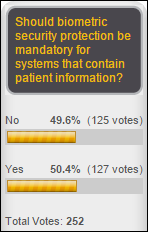
One thing that’s come to the forefront has been IT security. This is one that I’m pleased to see has gotten traction, but all of us in healthcare IT have very suddenly gotten large targets drawn on our backs and we need to move quickly. When I see the percentage of organizations out there that don’t have liability insurance for IT, that’s concerning.
It’s also concerning that a lot of the security incidents that have been reported are around theft or loss. It’s really under-reported because a lot of people don’t know that their systems have been breached. There’s an ignorance factor there as well. As we ramp up that, that’s going to be a major IT initiative — protecting our borders and raising our awareness around protecting our information. I was pleased to see that appear in the State of the Union address.
My other personal belief is that IT security — not just in healthcare, but in all industries — needs to start being addressed as a governmental issue. We have national security protecting our borders. We have a lot of protections out there. Our local municipalities have firemen and policemen. Yet hospitals essentially have to put guards at their doors and bars on their windows when it comes to IT security. We’re on our own to defend ourselves. Something that’s as critical to the US infrastructure as healthcare, financial, and other industries needs to be a larger governmental conversation.
Other than security, we’re looking at the desktop experience for our users. Having a greater awareness and a better experience for those users, especially the clinical users, to be able to roam from PC to PC and carry their session. We were an early adopter of something called Symantec Workspace Corporate and we’re now moving to an Imprivata and VMware combination solution. We’re going to be focusing on improving that end user experience with regards to speed, with regards to single sign-on, and maintaining security while making it easy for the user to carry their session throughout the hospital and for that delivery to be seamless. That also comes into location awareness and the other technologies that can be ahead.
The other item that we’re doing is working with Hill-Rom, which also comes into location awareness with our nurses. For tracking what they’re doing, but also giving them greater communication tools and greater meaningful alerts with some of the smart beds. That’s been an important strategy for us as well.
Integration between nurse call systems and IT systems for clinical alert management, communications, bed status reporting, and patient education has been a quiet change. How will that play out as bed manufacturers move into IT and the IT side of the house has the technology they need?
It’s fascinating that the bed management people are trying to figure it out. I had the pleasure of being in a focus group at the last CHIME conference with Hill-Rom. What I understood from them is they’re trying to figure out where there’s going to be overlap and not overextend their business where they’re not going to be welcome or where they’re not going to be able to make progress.
Longmont United Hospital has been a market leader in throughput and bed management and visibility solutions. We use what I’d call a command center in our shift manager office that has a view of every unit of the hospital. At a glance, you can see the occupancy of every single one of those beds. Over the next year, that will tie into our smart beds that will be connected. You’ll be able to know whether or not the patient is in the room.
It’s also tied into our CPOE system. When new orders are placed on the units, monitors show a map of the unit and there will be an alert showing that there’s new orders on the patient. Or perhaps it would show an alert that this patient is a fall risk or some other identifier for that patient without violating their privacy.
This has been an amazing success for us. It has reached every corner of the hospital. Our environmental services team is using this system where the beds get marked as no longer occupied to quickly identify that the beds are in need of cleaning. During busy periods of time, we can then quickly get patients from the ED into beds. We’re seeing an increased throughput and increased patient satisfaction. It integrates into our EMR. That visibility system has displays on all the units that our environmental services team looks at. if someone in a room has C. Diff, there will be a flag for the environmental services team so they know to use special cleaning precautions for that room. Through that simple alert, we’ve eradicated C. Diff as a hospital-acquired condition here at LUH.
With the smart beds, when a rail drops and a patient is a fall risk, you can have an alert that’s appropriate go to the nurse. We’re seeing a lot of opportunity. We’re also seeing a lot of overlap.
It will be interesting to see where the EMR vendors end and where those bed manufacturers like Hill-Rom and Stryker end. The bed manufacturers are trying to figure that out themselves because they have a lot of great technology that can be helpful, but I think they also know that they might not be welcomed into some markets that the EMR vendors own.
Tell me about your palm vein scanning project.
We were looking at how to improve the patient check-in experience. We started exploring kiosks similar to the airline check-in. From there, it evolved into how we would identify the patients as they checked in.
We started exploring the ability to use palm vein scanning technology as a biometric to identify patients. It uses near infrared light to looks at the vein pattern within your palm, which is 100 times more unique to an individual than a fingerprint. It also doesn’t have that criminology sort of connotation that some people associate with fingerprinting, so it has a higher patient adoption rate.
That palm vein pattern is developed in the womb and it’s even unique between twins. It’s a really unique and useful biometric that has high adoption rates among patients where you might not get it because a retina scan is pretty uncomfortable and fingerprinting has the criminology connotation. With palm vein scanning, you can get better adoption.
We’ve rolled that out where the patients need to initially enroll in the program. They go through the normal registration process, provide a form of identification, and then place their palm down onto the scanner. It’s a very simple process. That biometric is saved, so from then on when they put their palm down, we know who they are.
We no longer need to ask them sensitive information. The next time they come in, they have a better experience, because by just simply placing their palm down, they can avoid having to share sensitive information that can be within the earshot of someone else. They don’t have to show their ID every time.
The other places I’ve seen this technology used has been in test-taking, like the GMAT and the SAT, so that when people leave to go the restroom and come back, that they’re not switching for someone else to take their test. It’s also used in some other countries in banking. But I think the use in healthcare has extremely great promise.
Now that we have people enrolled, we’ll be able to use that as the identifier in the kiosks. In the next few months, we’re going to be installing these kiosks so that when patients come to check in at our hospital, they can simply put down their palm on the kiosk and then immediately be identified. It will ask them for some of their information to verify that it is accurate. If there are updates, they can correct that with the registrar. It will also know if they have a payment due — they can quickly swipe their credit card and we can accept payment there, which makes that more convenient for the patient as well. The purpose here is around improving the patient experience.
The other benefit is something that plagues hospitals and health systems nationally — duplicated and overlaid medical records. We spend a lot of time merging records because of minor differences when they come in. In large metropolitan areas, it is quite common that you have people with the same name and the same birthday whose medical records might be accidentally shared. That can be extremely dangerous since you have clinicians that are making medical decisions for those patients potentially based on someone else’s medical history.








































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…