I'd never heard of Healwell before and took a look over their offerings. Has anyone used the products? Beyond the…
News 4/4/14
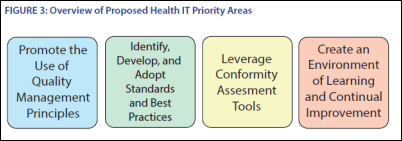
HHS releases a draft report from its FDASIA work group that includes a proposed strategy and recommendations for an HIT framework for maintaining appropriate patient protections and avoiding regulatory duplication. It reaffirms FDA’s position that its regulation is appropriate only for medical devices and not clinical software (including clinical decision support tools.) The report ponders the question of how a conformity assessment program (product testing, certification, and accreditation) might work and whether the government should play a role. It also recommends creating the Health IT Safety Center, seeking input on how it should be operated to share incidents, lessons learned, and user experience, also suggesting that third-party tests or reviews might play a role. The report describes three categories of health IT products:
- Products for admin HIT functions, such as software for billing, scheduling, and claims management that pose little patient risk. No FDA regulation is proposed.
- Clinical software for health information and data management, medication management, physician order entry, electronic access to clinical results, and most clinical decision support software. No FDA regulation is proposed.
- Products with medical device functionality, such as computer-aided detection software, software for beside monitor alarms, and radiation treatment software. FDA would continue to regulate products falling into this category.
Reader Comments
From Harry-O: “Re: NTT Data-supported Indy car. I’m pleased that we are no longer a client. While I understand that vendors need to market their products, those of us in the trenches are struggling to survive and pay their (for the most part) exorbitant support fees. Wouldn’t it be nice if they could find a way to market and reduce costs at the same time? What a waste, paid for by a hospital near you.”
![]() From Perky: “Re: ICD-10 delay. Does anyone have an inkling as to how things are going to proceed with such things as CQM reports and MU 2 demonstration/certification with the delay of the ICD-10? As I try to think this through, my head sort of explodes. If they are going to continue to require ICD-10 codes for the CQM, PCMH, and MU 2 reports, then how are the codes going to get entered if we are not using them for billing? If they decide to stick with the ICD-9 for CQM, PCMH, and MU 2 reports, what happens with the certification process? If we are not allowed to use ICD-10 until after October 1, 2015, what happens with all of the products that are already certified to use ICD-10? Are they expected to rewrite their reports using ICD-9? Do they then need to go through the certification process again?” Unfortunately Perky just hits the tip of the iceberg with his list of questions and CMS may not have enough disk storage to adequately address all the new FAQs. CMS has been been oddly silent on the whole issue all week, suggesting that no one at the agency saw the delay coming. One of the first steps towards clarity will be the issuance of a final rule for the new ICD-10 deadline. If anyone wants to stab at Perky’s questions, please share.
From Perky: “Re: ICD-10 delay. Does anyone have an inkling as to how things are going to proceed with such things as CQM reports and MU 2 demonstration/certification with the delay of the ICD-10? As I try to think this through, my head sort of explodes. If they are going to continue to require ICD-10 codes for the CQM, PCMH, and MU 2 reports, then how are the codes going to get entered if we are not using them for billing? If they decide to stick with the ICD-9 for CQM, PCMH, and MU 2 reports, what happens with the certification process? If we are not allowed to use ICD-10 until after October 1, 2015, what happens with all of the products that are already certified to use ICD-10? Are they expected to rewrite their reports using ICD-9? Do they then need to go through the certification process again?” Unfortunately Perky just hits the tip of the iceberg with his list of questions and CMS may not have enough disk storage to adequately address all the new FAQs. CMS has been been oddly silent on the whole issue all week, suggesting that no one at the agency saw the delay coming. One of the first steps towards clarity will be the issuance of a final rule for the new ICD-10 deadline. If anyone wants to stab at Perky’s questions, please share.
HIStalk Announcements and Requests

Assuming this isn’t your first time reading HIStalk, you contributed to the 8 million visit milestone. Thanks.
![]() A few highlights from HIStalk Practice this week include: AMA remains tight-lipped about the ICD-10 delay. Physicians in academic settings report higher compensation when more time is spent seeing patients versus performing research. Specialists who are late in adopting EHRs may struggle to meet Stage 2 patient portal requirements. European Union GPs report that interoperability issues, a lack of regulatory framework, and inadequate resources are the biggest barriers to adopting ehealth tools. The GAO recommends CMS expand its benchmarks for assessing Medicare physicians. Dr. Gregg contends that HIT’s next big role is to motivate change in consumers that will drive transformation in providers. Thanks for reading.
A few highlights from HIStalk Practice this week include: AMA remains tight-lipped about the ICD-10 delay. Physicians in academic settings report higher compensation when more time is spent seeing patients versus performing research. Specialists who are late in adopting EHRs may struggle to meet Stage 2 patient portal requirements. European Union GPs report that interoperability issues, a lack of regulatory framework, and inadequate resources are the biggest barriers to adopting ehealth tools. The GAO recommends CMS expand its benchmarks for assessing Medicare physicians. Dr. Gregg contends that HIT’s next big role is to motivate change in consumers that will drive transformation in providers. Thanks for reading.
This week on HIStalk Connect: IBM partners with the New York Genome Center to research genetics-driven brain cancer treatments with Watson. Rock Health’s digital health funding report recaps a record-breaking $700 million in funding in Q1, its strongest investment quarter to date. Airstrip acquires San Diego, CA-based Sense4Baby, a startup from the West Health Institute that markets wireless fetal monitors.
Upcoming Webinars
April 9 (Wednesday) 1:00 p.m. ET. Think Beyond EDW: Using Your Data to Transform, Part 1 – Avoiding Analysis Paralysis. Sponsored by Premier. Presenters: Kristy Drollinger, senior director of population health analytics, Fairview Health Services; J.D. Whitlock, corporate director of clinical and business intelligence, Catholic Health Partners; Sean Cassidy, general manager of information technology services emerging business unit, Premier, Inc. Are you ready to invest in an integrated data platform? Do you have a strategy to make the information accessible and actionable? How will enterprise data warehousing transform care delivery? There’s more to data analytics than simply deploying an EDW. Learn what goes into becoming an information-driven enterprise in the first webinar in this series.
April 16 (Wednesday) 11:00 a.m. ET. Panel Discussion: Documents, EMRs, and Healthcare Processes. Sponsored by Levi, Ray & Shoup. Presenters: Charles Harris, senior technical lead, Duke University Health System; Ron Peel, technical advisor, LRS; and John Howerter, SVP of enterprise output management, LRS. IT department in hospitals implementing EMRs often overlook the role of document-driven workflows. Prescriptions, specimen labels, and discharge orders, and other critical documents must be reliably delivered with minimal impact on IT and clinical staff. This panel discussion will discuss the evolving use of documents in the “paperless/less-paper” environment.
Acquisitions, Funding, Business, and Stock
GE Healthcare will acquire CHCA Computer Systems, the Canada-based developer of the Opera software application for OR management and analytics, of which GEHC Is a distributor.

MModal reaches an agreement with the majority of its bankruptcy creditors to cut its debt by over 55 percent, which is about $350 million. Investor’s Chair sitter Ben Rooks provides some financial perspective about the company in answering a reader’s question in his “Health IT from the Investor’s Chair”.
IMS Health Holdings, which sells de-identified patient prescription information, goes public in an IPO that values the company at over $6 billion.
Practice software vendor edgeMED acquires revenue cycle management company Physician’s Billing Alternative.
ZirMed acquires the payment processing, patient eligibility, and patient estimation business owned by TransEngen.
Pharmacy automation vendor Aesynt, which operated as McKesson Automation until its November acquisition by Francisco Partners, acquires Italy-based pharmacy IV technology vendor Health Robotics.

TreeHouse Health makes a six-figure cash investment in LogicStream, a provider of clinical decision support tools.
Sales
A healthcare quality collaborative headed by San Jose Clinic (TX) selects CompuGroup Medical’s CGM Enterprise suite for community health practice management.
Memorial Health Care System (TN) and St. Vincent Health System (AR) select MedAptus Professional Charge Capture for automated coding and billing.
Visiting Nurse Service of New York chooses Crescendo from Delta Health Technologies for homecare business management.
VNA of Albany and Visiting Nurses Home Care (NY) choose Homecare Homebase.

Oconee Medical Center (SC) adopts PeraHealth’s PeraTrend platform as its real-time clinical decision support tool.
The Center for Diagnostic Imaging (NJ) will implement Healthec’s HIE platform.
Craneware signs multi-year contracts with two unnamed hospitals in the Eastern US for about $6.9 million.
People

PatientSafe Solutions names Cheryl D. Parker chief nursing informatics officer.

Nextech appoints Ron Kozlin (Pilgrim Software) CFO.

CareCloud names Lee Horner (Eliza Corporation) chief sales officer.

Baylor Scott & White Health appoints 11 new members to its senior leadership team, including Matthew Chambers (Scott & White Healthcare) as CIO.

Aaron Karjala, CIO of the troubled Cover Oregon online marketplace, becomes the fourth top manager to resign his post.
Announcements and Implementations
Cherokee Regional Medical Center (IA) goes live on its $2 million Epic system.

Qatar’s Al Khor Hospital and Al Daayan Health Centre go live on Cerner.

Hudson Valley Hospital Center launches its MyHVHC patient portal.
Emory Healthcare and Grady Health System join the Georgia HIN.
The Spanish Catholic Center (DC) implements Forward Health Group’s PopulationManager and The Guideline Advantage.
Government and Politics
CMS issues a Daily Digest Bulletin that summarizes the newly passed Protecting Access to Medicare Act of 2014, Noticeably absent is any mention of the ICD-10 delay. The Bulletin notes that “more information about other provisions will be forthcoming.”
Innovation and Research
The New York eHealth Collaborative and the Partnership Fund for NYC call for applications for the second class of the New York Digital Health Accelerator, a program that will give up to 10 early- and growth-stage companies $100,000 each to advance their digital health technology efforts.
Children’s Memorial Hermann Hospital (TX) offers patients a chance to virtually visit the Houston Zoo, located across the street from the hospital, from their hospital beds using Google Glass.
Other
![]() I suppose this constitutes a bad day at the office, at least if you are the tree trimmer who is recovering after the chainsaw he was operating kicked back into his neck.
I suppose this constitutes a bad day at the office, at least if you are the tree trimmer who is recovering after the chainsaw he was operating kicked back into his neck.
The local paper covers the plight of a 25-bed critical access hospital in Arkansas, whose February computer fees of $63,000 contributed to a loss of $142,000. Administrators expect a $1.2 million EHR incentive check in May, but those funds will be used to pay off EHR vendor Healthland, which did not require the hospital to pay until it received its MU check.
Mercy Technology Services, the information backbone of the Mercy healthcare system, will market its services to other Epic users as the first provider accredited in the Epic Connect program.

A KLAS report on ICD-10 consulting services (with the unfortunately timed subtitle “Who Can Help in the Eleventh Hour”) ranks The Advisory Board highest for overall ICD-10 consulting performance, followed by Aspen Advisors. Optum and 3M earned the highest scores for on-site training.
The majority of health organizations participating in a HIMSS Analytics survey report having a formalized EHR governance structure in place with a structure that involves a cross-functional, multi-disciplinary advisory board or committee. The biggest EHR governance challenges are physician engagement and adoption.
Sponsor Updates
- 3M completes its acquisition of Treo Solutions, a provider of data analytics and business intelligence to providers and payers.
- Analyst firm IDC names Covisint a “major player” in worldwide federated identity management and single sign-on.
- Medworxx Solutions and Leidos Health will offer providers help with patient flow performance and analytics.
- Allscripts recognizes its customer Citrus Valley Health Partners (CA) for being one of the first organizations in the country to meet the 2014 MU Stage 2 requirement for electronic transitions of care, which it accomplished using Allscripts dbMotion.
- Wellcentive will demonstrate is population health management platform at this week’s AMGA meeting in Grapevine, TX.
- Biztech profiles ICSA Labs and its work certifying security products.
- The Health Catalyst team explains how population health management solutions lead to overall better health care.
- MedAssets president and CEO John Bardis headlines the SEMDA 2014 Conference as the Gala speaker May 7-8 in Atlanta.
- A local paper interviews Summit Healthcare founder and CEO Ted Rossi, who shares details of the company’s history and growth.
- A KLAS report on HIEs finds that 100 percent of InterSystems HealthShare customers have made HealthShare part of their long-term plans and say they would purchase HealthShare again.
- Craneware conducts its annual Executive Industry Leadership Survey to measure revenue integrity priorities.
- ADP AdvancedMD, Intelligent Medical Objects , The SSI Group and NextGen issue statements following the passage of the ICD-10 delay legislation.
- Kit Check adds Medi-span integration to its Trusted Pharmacist Medication Checks software.
EPtalk by Dr. Jayne

I seem to be rounding up lots of federal issues this week. Monday opened with an extremely heated discussion involving a hospital laboratory director, our medical group operations VP, and me. To make a long story short, one of our hospitals is refusing to play nicely in bringing a bidirectional interface live for our employed physicians. Although many of our physicians use a large national reference laboratory (mostly due to payer requirements) we have a handful of physicians who are being held captive because they are located in the hospital medical office building. The terms of their lease prohibit external vendors from picking up samples at the office after hours, which basically locks them out of the market. Since the practice specializes in OB/GYN and has a high volume of office-collected specimens, they’re stuck using the hospital’s lab and pathology services.
Although the hospital initially agreed to a bidirectional interface so the practice could meet its requirements for both structured data and CPOE, it is now balking under the excuse that a bi-directional interface isn’t “required” for Meaningful Use. They want the practice to figure out some way to create magic with electronic ordering that prints to paper requisitions and an unsolicited results interface. The orders can’t match up automatically, which makes a mess of all the numerators and denominators unless staff manually matches the results. I explained to the lab director in my best primary care voice that a bi-directional interface isn’t entirely about MU, but rather actually has a great deal to do with patient safety.
He didn’t seem to care that it would help close the loop on orders, making sure results were received and catching misses through electronic reporting. He actually suggested providers should use an accordion file and duplicate copies of the requisition. What century is this person living in? I understand competing priorities and limited budgets, but these are our employed physicians that we placed in the hospital building in good faith.
I thought at one point I was going to have to perform a stroke assessment on the operations VP. He made some threats about calling the hospital CEO to discuss breaking the lease and the lab guy still didn’t flinch. It was brinksmanship like I haven’t seen in a long time. I know the hospital CEO well and would love to be a fly on the wall when he calls the lab director and tells him to get it in gear. The bigger picture includes hundreds of newborn deliveries and even more GYN surgeries. Given the practice’s revenue boost to the hospital, I would bet money that the lab director will be singing a different tune by next week.
I’ve also been wrangling entirely too many consultants and administrators regarding the now-approved ICD-10 delay. We’re breathing a sigh of relief on the inpatient side because our hospital vendor still hasn’t delivered decent software. On the ambulatory side, I’m just aggravated, though. Our vendor worked extremely hard to deliver solid product and we’re upgrading very soon. I think of all the “real” enhancements they could have done to the software with the development dollars that they pumped into getting ICD-10 ready and out to the client base with ample time for everyone to upgrade.
Speaking of the legislation, did anyone read the whole thing? I did read the “Protecting Access to Medicare Act of 2014” and there were a couple of other gems that snuck in under the cover of the SGR patch. I love the fact that the Government Printing Office uses an old-school type face for the header on legislation. Check out Section 111, which gives hospitals some relief from the so-called “two-midnight rule” through March 2015. Of course “evidence of systematic gaming, fraud, abuse, or delays in the provision of care by a provider” can trigger an audit regardless.
Sections 205 and 206 include abstinence education and funding for the PREP personal responsibility education program. I know there are some sassy seniors out there, but I fail to see how throwing this in with the “Protecting Access to Medicare Act” makes logical sense. They should have called it the “Protecting Medicare, Serving Special Interests, and Tidying Up Odds and Ends Act.”
Fifteen million dollars for pediatric quality measures is in section 210. One of my favorite add-ons is section 216, “Improving Medicare policies for clinical diagnostic laboratory tests.” It requires laboratories to report their private payer contractual rates and test volumes to assist in establishing Medicare rates. So much for a free market (although we knew that was long gone with Medicare already.)
Another favorite (which I almost missed because of the mind-numbing and sleep-inducing effects of federal legislation) is section 218, which promotes evidence-based care by requiring physicians to use clinical decision support before they order certain radiology imaging studies. CDS modules can be part of certified EHR technology or independent. Eventually outlier physicians will require prior authorization before they can order studies. Just when you thought it was safe to go back into the water after MU2, there are more sharks circling. I hope the EHR vendors can code fast enough to keep them at bay.
The ICD-10 delay is in section 212, if anyone is interested. I gave up after page 31. A reader gave me my laugh of the day about the delay:
Dear Dr. Jayne,
I have three young boys and one of them is always winding up in the ER. This year alone we’ve already had boy vs. coffee table, boy vs. Evel Knievel bicycle jump, and boy vs. monkey bars. Every time our insurance pends the claim and sends me a letter asking for verification that the injury was not work-related or due to a motor vehicle accident. I wish they could figure out that if the boys are 4, 7, and 10 they’re probably not on the job. A quick skim of the ER note would give them the rest of the information. I was looking forward to ICD-10 because maybe the more specific codes would give the insurance company what it wanted in the first place. I guess I’ll have to wait another year to find out. Hopefully we’ll be less accident prone by then.
Those descriptions remind me of Struck by Orca and I’m thinking maybe a companion volume is in order. What’s your reaction to the ICD-10 delay? Email me.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre.
More news: HIStalk Practice, HIStalk Connect.






Dr. Jayne – all this talk of federal legislation and overly complicated bureaucracy brings to mind a great Washington Post article on yet another example of our government’s penchant for technological ineptitude, and ultimate love of all things paper: “The Sinkhole of Bureaucracy” http://ow.ly/vqBP5
@fdasia report
The patients are the losers. The vendors are the winners. The doctor and nurse users are the sufferers.
At what site does one leave comments on the FDASIA rules?
In March, HISTALK covered the FDA recall of McKesson Anesthesia EHR for misidentification of data, that could result in death, a Class 1 recall.
Is that not inconsistent with the statement that the health management IT is of low risk and need not be regulated, as stated in the FDA new release?
Just wondering what you and your readers think.
RE: From Harry-O: “Re: NTT Data-supported Indy car. I’m pleased that we are no longer a client. While I understand that vendors need to market their products, those of us in the trenches are struggling to survive and pay their (for the most part) exorbitant support fees. Wouldn’t it be nice if they could find a way to market and reduce costs at the same time? What a waste, paid for by a hospital near you.” This Indy Car sponsorship is actually done by NTT DATA corporate and it not related to the Healthcare Technologies Division. It is not used in any Marketing for Healthcare. So, it was not paid for by a hospital at all.