HIStalk Interviews Nancy Ham, CEO, Medicity
Nancy Ham is CEO of Medicity, A Healthagen Business.

Tell me about yourself and the company.
I’ve been in healthcare IT for an embarrassing number of years now, about 25. But I’ve always been focused on the same problem, which is, how do we move data in a way that empowers physicians to improve financial and clinical outcomes? And trying to conquer the barriers of siloed systems, lack of standards, lack of interoperability to make that possible and to try to serve it up to physicians in a way that meets them where they are and ideally flows into and supports their operational and clinical workflow.
The most recent two years, I have been leading Healthagen Technology Solutions, which is Aetna’s population health technology services and enablement arm.
It’s a little bit confusing that the company still operates as Medicity, but is under the Healthagen group name of Aetna. How does Medicity fit into Aetna’s overall business?
Aetna acquired Medicity four years ago, recognizing that the foundation of population health is real-time clinical data and the ability to then marry that with other kinds of data – increasingly like paid claims data and biometric data — but to marry it through a robust and secure infrastructure. I often talk about the iceberg principle — what’s above the water line is the new, updated GUI and the pretty dashboards, but the first product is the data itself.
Data quality, data security, patient matching, patient consent management … that’s really hard work. Medicity — which started as a health information exchange and that was the nature of the work that they did over about 10 or 15 years – has built up this robust foundation upon which now we can attach the other population health assets and capabilities that have come to us through Healthagen or Aetna. Medicity is now the unified face to the market. All of our products, no matter where they started, are now sold and delivered through Medicity.
Some of the newer capabilities we have through Medicity are Medicity Explore, bringing to market our analytics company, formerly called HDMS. A company that’s more than 10 years old and manages more than 30 million lives through analytics.
I think that’s a really important point for your readers. As they walk into HIMSS and into the barrage of all the companies all saying, “Here’s what we do,” think about scalability and maturity capabilities. One of the first questions I always ask of an analytics company is, "How much data has processed through your engine?” Because healthcare is just this giant pile of corner cases. You have to meet them and defeat them one by one.
We have Medicity Manage, which brings in our ActiveHealth Management capabilities, which include care management analytics, risk stratification, predictive algorithms, gaps in care, registries, and also brings a really elegant provider-facing care management workflow. Because at the end of the day, the point of all this data, all these products, is to change and improve the actual care you deliver to a real person at the end of that line. You have to put all these things together.
Are providers really demanding interoperability or is everybody else just wishing they would?
[Laughs] They are increasingly demanding it because they’re getting into significant enough population health programs that the lack of interoperability, or the gaps that are created, are expressing themselves. Just as an example, if you are managing a panel of congestive heart failure patients, when you see gaps in the care record, you realize that’s a problem — when you don’t see that they had an admission at that hospital or when you don’t see that they had a test at that physician. It’s now impeding your actual ability to provide continuous care.
For me, that’s what population health is about. It’s moving from episodic, snapshot blinks of the patient to a movie. It’s like going to a movie and half the scenes are missing, so you can’t follow the plot line. That’s where the lack of interoperability is showing itself at scale now, because we are moving into true population health and people are saying, "This is not working. I need the whole movie."
Aetna has a view into all of healthcare. What does it see coming that the market might not have figured out yet?
We have a point of view, borne out by the recent Rand study, that providers buy into the fact the world is changing. They are moving from fee-for-service to something else. They are on the journey to risk. They might be at many different places on that continuum. What’s really fun is when they are at many places on that continuum simultaneously. They are in a different place for Medicare versus Medicaid versus commercial.
Technology alone is insufficient. Services alone are insufficient. Clinical alone is insufficient. You have to fuse it all together and bring risk management, i.e, I am going to be financially at risk. How do I think about that? How do I manage actuarial pricing?
Those are capabilities that health plans have that providers traditionally haven’t had to have. You have to have data and technology to move that data around appropriately to the right physician, respecting patient consent and privacy. Then you have to have clinical workflow to take advantage of everything you are doing. It needs to come together in a different kind of interoperable way.
What’s the big-picture view of interoperability and where is it moving?
I see the lines blurring. Medicity is very proud to power nine statewide HIEs, and yet when I think about the work that’s happening in those states, it is about public-private partnership. A really interesting example or theme is how payers are now becoming significant participants in these networks. One of my customers has a great phrase — she calls it ecosystems. We are evolving to healthcare ecosystems.
In a healthy ecosystem, everyone contributes as well as receives. What we are seeing now is new stakeholders come to these ecosystems and say, "I’m a payer. First of all, I have data to contribute to the ecosystem. I have claims data. I have medication history data. I have care management data. Let me contribute my data to that ecosystem. Then whether you are an individual physician or hospital participating in that ecosystem, you can now benefit. Let me receive information from that ecosystem, such as real-time clinical data, alerts that a member has just been admitted to the hospital, so I can activate my own care management programs."
We think it is a fading distinction between public, private, and regional. What we see are these localized healthcare ecosystems in which increasingly we are seeing everybody in. Which is exciting because that’s been the vision all along — creating clinically-connected communities. Wherever you go as a patient, wherever your family member goes, your data is accessible, contextual, and available.
Who should pay the cost of interoperability? How do we make sure that we aren’t building individual proprietary silos?
First of all, I hope no one out there is thinking that their main business model is selling data or monetizing data. Data is just an input into an improved healthcare system. We are all trying to lower the cost for data to flow into these ecosystems so they benefit the actual care and cost for what is going on.
I see that increasingly, people understand this mutuality. If I want to get data, I need to provide data. By the way, it is the patient’s data. We are all trying to contribute to create that clinically complete view of the patient, so that as they navigate the healthcare system, they are getting the best possible care. What I would like to see is simply a continued investment by us as an industry in standards in interoperability so that we reduce the cost and the friction of data moving.
The monetization should be by whoever’s at risk. If you are the payer, if you are the employer, if you are the state government, if you are the federal government, if you are the provider … Whoever’s at risk financially and clinically for that patient is who is benefiting from having access to a more complete clinical and financial record — they are the ones who should underwrite the cost of having created that.
How would you set up an economic incentive to align the interests of those who benefit from the data with those who contribute it for someone else’s benefit?
I would love to at some point have a longer conversation about some really successful statewide networks. Colorado, Ohio, Delaware, and Vermont have achieved, or are close to achieving, 100 percent connectivity — hospitals, physicians, DME, SNF, long-term post-acute, payers, the VA, Social Security, the prison system. They have developed models where all the constituents in their community are now participating in the system and have a shared goal of improving the health of their citizens.
There are statewide models that are working very effectively now on a multi-stakeholder basis. The revenue models are all a little different, but a lot of them were started up by hospitals wanting to replace phone, fax, and courier with more modern means of delivering clinical information electronically to physicians.
Now what you are seeing is the next wave of stakeholders coming in, contributing both data and funding. Any network has a semi-fixed cost, and spreading it across now a broader community, which is exciting to see. As new people arrive, they have to connect to the network and subscribe and help underwrite its cost as well as contributing their own data.
What is the next level beyond where we are now with population health management technology?
In some ways, I think we are still at the first level, which is trying to create data completeness. We talk about building complete, ubiquitous, and indispensable networks. Those words have a lot of meaning for us.
Complete means data completeness. No network is ever data complete because there’s always the new frontier. We conquered a lot of real-time clinical data. Now we are all trying to get ambulatory data, CCDs, consolidated CDAs out of ambulatory practices. Payers are arriving at scale to contribute the data they have. Biometric is a new frontier. We are doing a really interesting pilot with Cleveland Clinic and Medtronic. There’s always going to be more data. We will never be data done.
Ubiquity is around Moore’s Law — the more connection points on a network, the more powerful it is. If you think of networks as being geographically-oriented, clinically-connected communities, you are always going horizontally and vertically to create more data and connectivity density.
The new wave of population health is the third word, which is indispensable. Which is about, does any of this matter? Are we creating a difference in the Triple Aim? Are we improving health, improving care, improving cost? The new wave is actual measurement in ROI.
We are going to have to embrace and learn as an industry that a lot of things we are doing right now, while interesting, aren’t transformative. Trying to figure out where we can hone in. A lot of that honing is going to maybe be the fourth new frontier, which is direct patient engagement. Engaged in their own care, with their own data, with their own protocols.
Do you have any final thoughts?
I’m both excited and worried about the state of the state for population health. I’m excited about the pace of innovation, the number of new entrants, the amount of invention that’s happening. But I worry that it’s a little untethered from the jobs of cost and quality. That it’s untethered from risk management and care management. I want to be sure as an industry that we are being purposeful in effecting change, not just in creating new software tools.







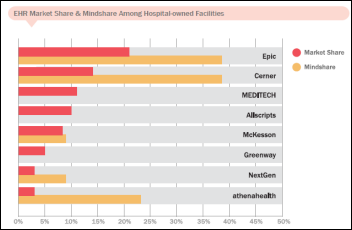








































"A valid concern..." Oh please. Everyone picks the software they like and the origin of that software is an afterthought.…