Top News
Premier acquires financial analytics vendor Healthcare Insights for $65 million in cash.
Reader Comments

From Bean Enumerator: “Re: North Shore-LIJ’s JV with Newport Health. Newport says it has experienced and innovative health IT talent, but the only person listed as working for the company has no relevant experience whatsoever. It’s a bad sign when an investment banker starts a health IT company. How did Allscripts lose this one given their supposedly tight partnership with NS-LIJ and their population health management aspirations?” I couldn’t find much of anything on Newport Health other than it’s apparently connected to Newport Private Group with a real office in Newport Beach, CA and mail drawer addresses in New York and Texas. The site contains nothing that suggests why they would make a good partner for NS-LIJ or anyone else for that matter.
From Divine: “Re: Cerner. Have you heard anything about them pulling their Intermountain team back to Kansas City?” I have not.
From ACOver: “Re: Aledade. You didn’t mention that the company is expanding.” Farzad’s Aledade has nothing to do with health IT, which some of the HIT sites can’t quite grasp in confusing his former job with his current one. Non-HIT sites with healthcare reform and insurance followers are the place for that kind of story rather than HIT sites that just reword Aledade’s press releases without adding any value whatsoever.

From GeneInsight SchmeneInsight: “Re: Sunquest and Partners HealthCare marketing GeneInsight software. While the GeneInsight investment may be helping, I spoke with two folks (Meridian Health, NJ and Main Line, PA) each doing due diligence on enterprise systems to include ripping out Sunquest. Epic and Cerner are being vetted at both sites.” Unverified. The challenge with being a best-of-breed vendor is that your fervent, enterprise-resistant users don’t have the final word when health systems consider buying a broad, good-enough integrated product line from a company that supports it all. Those dominoes have been falling for years – lab, radiology, and pharmacy are moving (or being pushed) to Epic and Cerner from their favorite departmental systems. I haven’t seen any evidence that patient outcomes or costs have suffered as a result despite the dire predictions from the folks in those departments whose niche systems were, in their minds, integral to their unique mission.
HIStalk Announcements and Requests

Welcome to new HIStalk Platinum Sponsor YourCareUniverse. The Franklin, TN-based company offers cloud-based technology and expertise in consumer relationship management, putting consumers at the center of the health system’s strategy. Patient-facing modules include YourCareHealth (personal health records), YourCareWellness (a wellness portal), YourCareEverywhere (consumer health content), and YourCareNavigation (rules-based care and wellness plans). Provider-facing technologies include a patient education content repository for clinician prescribing, community risk stratification analytics, an HIE and HIE connector, a patient transfer application, a Salesforce-integrated consumer marketing system, and a referral management system. The company also offers strategic consulting to guide organizations through transformational change. YourCareUniverse quickly signed up 38 customers after it was launched early this year, with its first go-live last month at Mount San Raphael Hospital (CO), which is using the patient engagement capabilities to promote its brand to consumers. Thanks to YourCareUniverse for supporting HIStalk.

The YourCareUniverse folks are excited to present their two-day “Transvisional Forum: Transforming the Health of Consumers Through Engagement” conference September 16-17 at the Music City Center in Nashville. Topics of the nine educational sessions include cultivating consumer loyalty, managing the digital patient, analyzing big data, and increasing volume. Keynote speakers are Nicholas Webb (author of “The Digital Innovation Playbook”), Farzad Mostashari, MD (former National Coordinator and CEO of Aledade), Steve Blumenthal, JD (health IT attorney and all-around HIStalk pal), and Jitin Asnaani (executive director, CommonWell Health Alliance). Early bird registration is $795 through this Saturday, August 15.
This week on HIStalk Practice: Texas physicians struggle to keep their doors open and spirits up. HelloMD pivots its telemedicine services to medical marijuana. The Senate approves the Electronic Health Fairness Act, while HHS gets a black eye over breaches. Kathryn Evans offers best practices for leveraging technology to ensure reliable disposal of hazardous drugs at physician practices. HHS Secretary Sylvia Burwell announces $169 million in funding for new health centers. CSI rolls out Doctor on Demand telemedicine services. SecurityMetrics develops a HIPAA Dashboard for physician practices.
This week on HIStalk Connect: Google X Labs partners with DexCom to develop a miniaturized, disposable continuous glucose monitor. Twitter introduces an API exposing its entire 500 million tweet history to software developers. A Cambridge, MA-based genetics startup raises a $120 million Series B to advance its research into CRISPR-Cas9 gene editing therapies. A consortium of European researchers is developing a "smart mirror" that will screen users for early signs of chronic diseases.

My love-hate affair with Windows 10 continues after one of its silent updates trashed my laptop’s Wi-Fi connectivity yesterday due to what I initially thought was device driver incompatibility. I spent a couple of hours trying to fix it before giving up and taking it to the repair shop (which I’ve never had to do since I can usually fix things myself). The shop owner left a message last night saying he had spent hours of analysis without figuring out a solution, with the only option he could suggest being to downgrade back to Windows 8.1. I returned his call this morning and he had experienced some sort of nocturnal epiphany and fixed the update-corrupted Windows networking components by matching up individual DLLs with versions and dates and then reinstalling and registering them one at a time. It’s back on my desk working fine. The $89 cost was worth it and I’m pretty happy to keep Win10, although I’m annoyed at the exasperation and expense of fixing the damage it caused and fearing the havoc the next update will wreak. The repair shop owner has added my problem to his Win10 issues folder, which is rather thick after just two weeks of its availability. He’s probably thrilled at the business uptick.
Webinars
August 25 (Tuesday) 1:00 ET. “Cerner’s Takeover of Siemens: An Update (Including the DoD Project).” Sponsored by HIStalk. Presenters: Vince Ciotti, principal, HIS Professionals; Frank Poggio, president and CEO, The Kelzon Group. Vince and Frank delivered HIStalk’s most popular webinar, "Cerner’s Takeover of Siemens, Are You Ready?" which has been viewed nearly 6,000 times. Vince and Frank return with their brutally honest (and often humorous) opinions about what has happened with Cerner since then, including its participation in the successful DoD bid and what that might mean for Cerner’s customers and competitors, based on their having seen it all in their decades of experience.
Previous webinars are on the YouTube channel. Contact Lorre for webinar services including discounts for signing up by Labor Day.
Acquisitions, Funding, Business, and Stock

Roswell, GA-based Tea Leaves Health, which sells hospital marketing software, will be acquired for $30 million by consumer health website publisher Everyday Health. Tea Leaves Founder Reuben Kennedy will make a pile of money he doesn’t really need given his LinkedIn endorsement of a car detailing company that attends to his “five Ferraris, several Porsches, and a Lamborghini.”
PokitDok, which offers 16 healthcare transaction APIs for application developers, raises $34 million.

DispatchHealth, which offers cities a mobile acute care alternative to dispatching an ambulance in response to 911 calls, raises $3.6 million. Dispatchers route non-urgent calls to the company, which sends out cars with a clinician, a mobile lab, medical equipment, medications, and Internet connectivity. The company was previously known as True North Health Navigation. It doesn’t indicate pricing, but a FAQ on its old site suggests $200 to $300 per visit with insurance accepted.

Freshly IPOed telehealth vendor Teladoc reports Q2 results: revenue up 78 percent, EPS –$7.20 vs. -$2.15. The company warns that it expects to lose $50 million in the fiscal year. Teladoc reports that 83 percent of its revenue comes from the per-member, per-month fees paid by employers, health plans, and health systems, with the remaining 17 percent coming from visit fees averaging $40. Teladoc made reference to future possibilities that include behavioral health, dermatology, second opinions, at-home testing and biometrics, post-discharge monitoring, and wellness programs.
In a strange business shift, HelloMD, which previously offered expensive, cash-only video visits with big-name medical specialists, relaunches itself as a seller of $49 video consultations for medical marijuana cards. Note that the site says “Approved in 20 mins,” which suggests that a minimal amount of clinical rigor is applied during the video visit. The lady on its home page indeed seems to have been relieved of all her medical suffering and is now in a blissful state of deep-breathing wellness, surrounded by clouds.
Sales

BayCare Health System (FL) chooses Legacy Data Access to retire its SoftMed application.
New England Healthcare Exchange Network chooses Cognizant and its TriZetto subsidiary to manage its technology infrastructure.
University Hospitals (OH) will use Sectra’s vendor-neutral archive.
Cambridge Health Alliance (MA) chooses Imprivata’s two-factor authentication for e-prescribing of controlled substances.

Athol Hospital (MA) will implement Medhost’s ED information system.
People

Cureatr appoints former Highmark CEO William Winkenwerder, Jr., MD to its board.

Bill Wallace (Kansas HIE, BCBS of Kansas) takes over as interim CEO of the Kansas Foundation for Medical Care.

University of Iowa Health Care names Maia Hightower, MD, MBA, MPH (Stanford Health Care) as CMIO. She replaces Douglas Van Daele, MD, who will serve as executive director of University of Iowa Physicians.
Announcements and Implementations
InterSystems will use technology from Validic to integrate user-generated and wearables data into its HealthShare interoperability suite.

HIMSS brags on its Cleveland conference center and its role in helping its vendor members market their products as it trolls for “collaborators” (i.e., paying tenants). The upcoming events list isn’t very compelling with mostly small HIMSS meetings and vendor presentations for attendees yearning for a junket to Cleveland. I’m starting to think that from my experience with health systems and member organizations that the concept of non-profit (meaning “non-taxpaying”) organizations should be eliminated.
Government and Politics
A GAO analysis finds that the VA and DoD are working on interoperability between their systems, but are missing dates and won’t be finished until 2018.
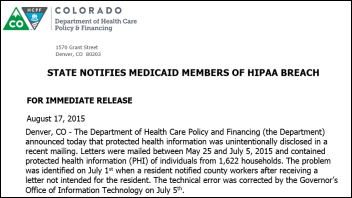
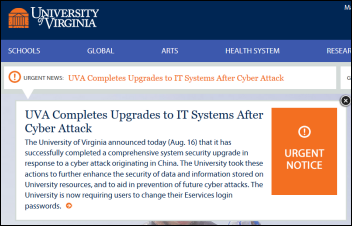
Privacy and Security
The Economist ponders whether databases can remain useful after being anonymized, or if in fact real anonymization is even possible given the relative ease of matching one database to another to re-identify the information. Possible solutions include releasing data only to researchers rather than to the general public, making data recipients sign use contracts, making re-identification illegal, encrypting data queries as a package so that researchers can’t see the underlying data rows, and dividing the database among multiple hosts.

The Greater New York Hospital Association bans filming in the city’s hospitals without the the prior written consent of patients, embarrassed by a 2012 episode of “NY Med” that captured the ED death of a patient whose family recognized him on TV despite his digitally obscured face.
Innovation and Research
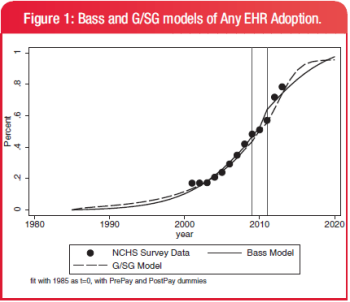
I can’t see the full article since I don’t subscribe to JAMIA, but I would question the methodology of this study, which concludes that HITECH didn’t change the EHR adoption trajectory – it was just practices without EHRs imitating those that had them.
Other

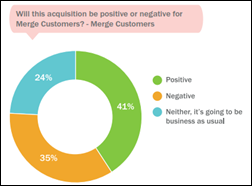
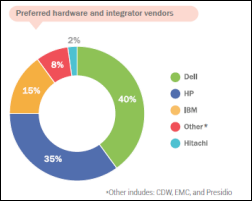
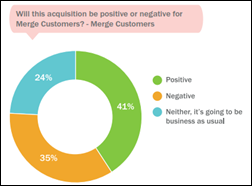
Peer60 publishes a “Rapid Reaction Report” on IBM’s planned acquisition of Merge Healthcare, collecting thoughts from 130 healthcare leaders in the two days following the announcement. One-third of the Merge customer contacts said the acquisition will be negative, but 20 percent said they will expand their use of Merge’s solutions under IBM’s ownership. Radiology and non-CIO IT folks felt pretty good about the announcement, but 60 percent of CIOs see it as negative. The main concern seems to be whether IBM is too big and too light on PACS knowledge to keep Merge customers happy while they try to sex up Watson with Merge-supplied “eyes.”

A British newspaper profiles EMIS Health Managing Director and former Misys Healthcare executive Duane Lawrence, noting that he was the #1 territory sales manager for Coca-Cola at 22 years of age before deciding, “I wanted to do something that was going to make a difference.” I can’t think of any positive healthcare difference Misys ever made other than getting out of it, but perhaps he has finally found his calling.
The shrill shrieking for Internet attention has unfortunately encouraged the proliferation of witless, intellect-insulting puns in headlines, I’ve noticed. The reporter’s credentials suggest he should know better, although maybe I’m expecting too much since he also contributes to “Painting and Wallcovering Contractor.”
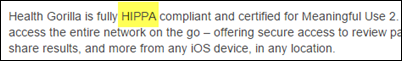
Nice job spell-checking, Health Gorilla (or is that Health Gorrila?)
The former network manager of Yukon Kuskokwim Health Corporation (AK) is indicted for collecting and distributing child pornography over the hospital’s network after investigators find 29 terabytes of images and videos.
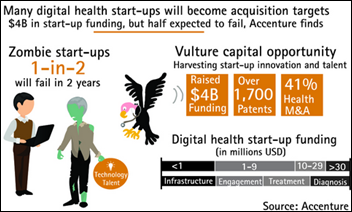
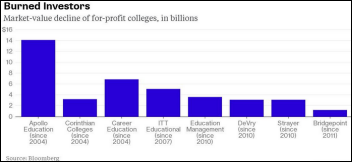
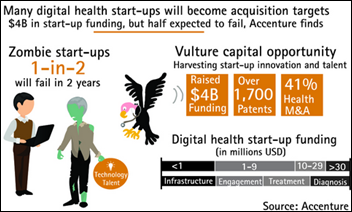
An Accenture analysis of 900 digital health IT startups labels half of them as “zombies” that are likely to fail in their first two years, creating a “vulture capital’ market in which better companies pick at their carcasses for people and technologies. The report identified the zombie startups as those “dead but unaware of it” companies that raised up to $50 million from 2008 through 2013 but haven’t had new financing in the past 20 months. I’m not as optimistic as Accenture that those struggling newcomers have people or intellectual property worth poaching, but we’ll see. They left out the most interesting part – the list of those companies they targeted as zombies. It would be fun to run a death pool contest.
In Australia, a state review of the new Queensland children’s hospital finds that patients were endangered in the rush to open the facility quickly before medical equipment, computer systems, and even hand sanitizers were in place. Employees didn’t meet each other for the first time until the day of opening. Everyone agrees now that the hospital needed another two months before opening its doors.

I winced when I saw the “register for HIMSS16” subject line in my inbox. The pushed-back Chicago version was like Daylight Saving Time – it was great having the extra weeks before last year’s conference, but now we’ll all pay as the clocks are set forward for Las Vegas and the dreaded week comes all too quickly (you’re likely an HIT newbie or anything-to-miss-work conference junkie if you actually look forward to it). Early bird member registration runs $765. Las Vegas always requires messing up the familiar schedule to accommodate the busloads of gamblers that the hotels and casinos won’t displace over the weekend, meaning the HIMSS conference runs Monday through Friday instead of Sunday through Thursday. The opening keynote will be at 5:00 p.m. Monday and the exhibit hall won’t open until Tuesday morning. HIStalkapalooza will be Monday night as usual, so hopefully the opening keynote will be as unappealing as in the past several years so people can bail out to arrive at my event on time. The closing keynote will be delivered by noted healthcare IT expert Peyton Manning, who will face a Friday afternoon audience smaller than at a Denver Broncos closed practice scrimmage. Hotel rates are, as always, jacked up for expense account attendees, with the same Treasure Island room running triple what it would cost to go next week in the miserably hot Las Vegas summer. In case you forgot, HIMSS announced earlier this year that the conference will alternate between Las Vegas and Orlando, having outgrown all the more interesting places.
Sponsor Updates
- E-MDs offers a free ICD-10 Survival Kit.
- Extension Healthcare offers “Market Trends: Counting Down to Alarm Safety Readiness.”
- Galen Healthcare offers “Healthcare Interoperability Musings: Incentives, Barriers, Blocking.”
- Access demonstrated its electronic forms and signatures solutions at Meditech South Africa’s event in Johannesburg.
- Greenway Health posts “Electronic Prescribing of Controlled Substances: a Convenient Tool to Improve Patient Care and Safety.”
- Hayes Management Consulting offers “Secure Messaging – Why It Makes Your Job Easier & Your Patients Happier.”
- ZeOmega earns NCQA’s disease management certification.
- The HCI Group publishes “4 Steps for Success: ICD-10 Training for Physicians and Non-Clinicians.”
- HDS offers “FDA Warns of Medical Device Hacking.”
- Cumberland Consulting Group is named to the Inc. 5000.
- Healthfinch says “Document, Document, Document!”
- HealthMedx offers “Proposed CMS rules set new destinations for SNFs … but where’s the path?”
- Healthwise offers “Engaging Moms on Medicaid.”
- Iatric Systems posts “EHR Optimization: Go-LIVE Marks the Beginning.”
- VitalWare is named to the Inc. 500/5000.
- Impact Advisors is recognized by KLAS for service performance.
- InstaMed offers “In Healthcare Payments, EMV May be a Driver, But Dodging PCI is the Benefit.”
- InterSystems and Leidos Health will exhibit at the Defense Health Information Technology Symposium August 18-20 in Orlando.
- Liaison Technologies is named a finalist in the 2015 North Carolina Healthcare Information and Communications Alliance Health IT Transformation Awards.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us or send news tips online.



































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…