Michael Nelson is CIO of Universal Health Services, a publicly traded, Fortune 500 hospital management company in King of Prussia, PA that is also the parent company of Crossings Healthcare Solutions, which offers advanced clinical decision support software for Cerner Millennium users.
Tell me about yourself and the company.
I’ve been with UHS for eight and a half years as a chief information officer. In those eight years, the company has doubled in size from $4 billion to $8 billion in revenue. We’re a healthcare provider-based organization with roughly 25 acute care hospitals and $4 billion in revenue for that division and 215 behavioral health facilities with roughly $4 billion in revenue for that organization.
UHS is the parent company of Crossings Healthcare Solutions. Crossings is where we’ve had the most clinical innovations that we sell to the market, but that functionality was all created and embedded for UHS use. We’re not trying to make a material profit with our Crossings subsidiary, but rather subsidize having a lot of clinicians involved in IT. That’s the real purpose.
You’ve worked for both non-profit health systems and now a publicly traded, for-profit one. How are those settings different?
Prior to working at UHS, I worked for the Carolinas Healthcare System in Charlotte, North Carolina, a well-run, large integrated healthcare delivery system of hospitals, physician practices, etc. They are a well-run not for profit. As I transitioned into the for-profit sector, I had curiosity as to what the differences may be.
The founder of UHS is still here 35 years later, Mr. Alan Miller. I think UHS is a little different from your standard for-profit company in that it has been established and it operates for the long haul. We insource and operate the majority of our IT. We pay Cerner to host our EMR platform, but we run our own help desk. We run our own help desk for the Cerner platform. The PC tech team is ours and not outsourced. We look to operate efficiently and effectively, providing good services from an IT perspective.
Even though we’re for-profit and publicly traded, we are operated for the long haul. In my eight years, I was never asked to decrease staffing due to a challenging financial market. If you think back to 2008 and 2009 when times were tough, we did not reduce head count because we’re very careful in what we add. We want to operate efficiently and continue to serve the customers and the physicians well.
I think UHS is a little different in that regard in the for-profit world. I’ve found that our goals are substantially the same — quality, patient safety, and have IT deliver effective services to the customers. A lot of those themes are exactly the same in the for-profit world, even though I would say there’s an incremental focus on expense management.
For-profit healthcare IT technology deployments seem to have been selective, with less investment in clinical and patient-facing systems. Did you find that to be the case at UHS?
When I got to UHS, they had a best-of-breed focus, as did many organizations back in the early 2000s. We had an opportunity to reconsider that approach.
As I joined the company, the revenue cycle was stable and effective. There had been a major investment in what used to be the Siemens Invision platform, which is now owned by Cerner. The corporation needed an improved clinical IT, so we went down and determined our strategy was going to be a more innovative approach.
As we started the Cerner EMR implementation, I advocated for – and the president of the company, Mark Miller, supported — adding a chief medical information officer. Until we started our Cerner deployment, we didn’t have that. We added that one physician. Then that physician was so effective for us that we added three other full-time physicians in IT.
As far as I know, we’re the only for-profit that has four physicians full-time embedded in IT that sit across from my informaticists and my programmers on the same floor in our building. Our cycle times to make modifications, customizations, and enhancements is reduced because of the close physical proximity and the alignment with IT.
I think your characterization of for-profits is generally accurate. Between the work that Tenet and Community and we at UHS have done in the last four or five years across those organizations, there has been a huge focus on clinicals. We added clinicians into IT and I think that’s the secret sauce to having enhancements that we’re able to sell to other people.
You mentioned that you have a lot of behavioral facilities. Is the technology deployment different there as it usually is outside of the hospital setting?
We have different IT in the two divisions. We run different registration and clinicals in behavioral health as opposed to our acute.
In the behavioral health division, we have been piloting a couple of different EMRs that are better adapted to that environment. They have some documentation requirements and clinical processes that are materially different than acute care. A standard acute care EMR has not worked well in the behavioral health division. Lately, we found a vendor that’s a pharmacy IT vendor that has CPOE, etc. and leveraging that specialty system into our behavioral health has produced the best result so far.
They’re not running ORs, typically. They don’t have a lab. They’re not running radiology. Finding a good niche pharmacy system that has a CPOE component that allows the behavioral health to be effective with patient medication management — that’s really been the right piece for them. But we do have EMRs in select facilities. Then our acute care division is very standard with the rest of the acute industry.
There is separation differentiation at some of our large acutes. We have behavioral health pavilions, large inpatient units. At those locations, they use Cerner. We’ve worked to enhance Cerner so that it can meet the majority of their needs. We’ll continue to do it as we go forward.
What can you do with Cerner’s MPages and Advisors?
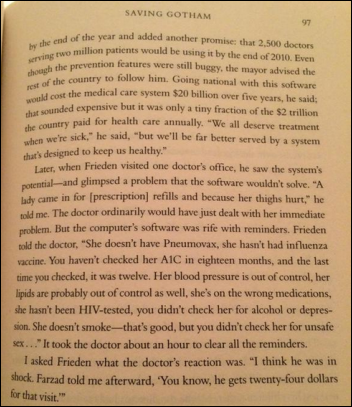
We can aggregate data that are on multiple screens within the system into one unified view. Instead of a physician having to go through seven clicks to renew a medication order that’s about to expire, we can have an MPage that displays all the med orders or any other orders, such as restraints, that are going to expire. Basically in one click to two clicks, they can renew all those orders when typically they would have to navigate to the orders page, review all the orders, determine which ones might expire, select those individual ones, and approve them.
Our goal using the Cerner tools has been to reduce the clicks for the physician and present information that they can take immediate action on and solve the conundrum of "Yes, the EMR has what needs to be done, but it’s not easy to get to it, it’s not easy to take that action, and IT, you guys aren’t providing me any value with the out-of-the-box EMR."
Do inpatient EHR vendors offer enough tools and technologies to allow users or third parties to extend or modify their basic functionality?
I can speak from my experience with the Cerner EMR, having implemented that at the Carolinas and at UHS. The MPages functionality, the Cerner Command Language CCL Programming tool set, has allowed us to extend the functionality of Cerner and address workflow issues that we see. That’s been good technology that when properly leveraged, adds real value.
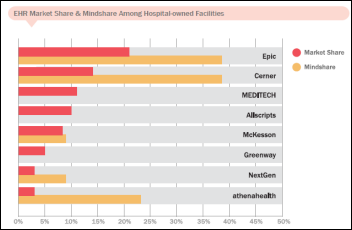
Other vendors might not have been flexible enough early, but you’ve seen Epic adapt to that. They’ve rolled out equivalent functionality from what I understand, but I haven’t used it directly. How much or little Meditech does, I don’t know.
A lot of vendors that are smart realized that healthcare is not one size fits all. You don’t want to just let them have configuration choices — you want to let them enhance the tool. The direction is more positive as opposed to less. I’m pleased with Cerner. We’ve been able to get real value from that.
Are you hungry for additional capabilities to the point that you’re asking Cerner for more openness or APIs? Do they see that as competitive with what they want to offer the market in general?
We are actively working with them on some technical tools that are going to provide better alerting and information from a technology perspective.
I worry about end-to-end response time. Our end users in the hospitals are on a PC. They’re going through a Citrix session. They’re connecting across our wide area network to the Cerner data center. There’s an application set of functionality and there’s a database server. I care about that end-to-end response time. Cerner has got great tools to manage the database and tell us what the database response is, but they can’t tell us Citrix session response times front to end in our facilities. We’re working on trying to get them to allow us to do some different things and installing tool sets in their managed services environment.
We’re pushing and advocating for the things that we need from an IT service delivery perspective and I think they’ll react to that. It will take a while. There’s still continued tools that we need, but it’s a step at a time. It’s a journey with the EMR stuff. Nothing is ever done overnight. if you think about client-server, that was the rage, but eventually people wanted to push everything to the cloud. You go through technical changes, but what you want is effective IT delivery for your end users.
Was it different to have to take a vendor mindset when developing something new that could be used, hopefully in shrink-wrapped fashion, by another health system?
Absolutely. We added several technical staff members to help package up code sets so that it would be deployable to other organizations. Cerner’s EMR and other vendor EMRs have configuration choices. Based on those configuration choices, our enhancements may work more straightforward –out of the box, if you will — or we may have to modify those enhancements to meet the configuration choices that a customer made.
We invested resources and time to package up the enhancements so that they were more readily usable. We worked to add some user admin tool sets so that they could modify some functionality without having it have to be hard coded and programmed into those solutions.
Absolutely, you cannot just take an enhancement we’ve made and plug and play it somewhere else. You need to think through that commercialization and how do you package that up and get it ready with release notes, etc. We went into with a mindset that we would have to, for our Crossings subsidiary, invest in commercializing the software, which meant packaging it up, making it ready for deployment, and usable. We’ve worked hard to make that effective at our first customers.
Vendors are announcing customer partnerships, like the Cerner-Intermountain one, where they’ll work together to develop intellectual property that will be added to the vendor’s base product. Is that a growing practice? How will it affect the industry?
Through the years, you’ve seen an increase in that. Cerner previously had a relationship, I believe, with the Chicago Institute of Rehabilitation. They had a rehab-specific module that Cerner customers could purchase. Other vendors have had different types of announcements with third-party organizations. I think that will continue in a limited fashion, where that third party can help the vendor create functionality that would have otherwise taken the vendor too long or they might not have gotten to and lost a market opportunity.
Cerner has worked with Advocate on the population health side. I think that’s helped Cerner move more rapidly than perhaps they could have on their own. I think it’s a smart move from the vendors. They’ve got to pick the right organization that has similar business needs to other possible customers to create products that offer real viability in the market. It makes sense on a limited basis where they can control and manage the scope. It keeps them ahead of what customers are demanding.
I think it’s in my personal best interest that Cerner has as many products as I might want. It’s my personal opinion. Some of it will apply to us, others of it may not, but I think you’ve definitely seen a continued trend to do that in a focused manner.
It’s disillusioning to a clinician who moves to the vendor side to realize that what’s holding innovative functionality back isn’t always a shortage of good ideas, but rather navigating through convoluted internal development, testing, and release processes. Have technologies changed so that a good idea be turned into a software enhancement quickly and reliably?
Technology has given us capabilities to decrease the time for that development cycle. But there is still idea generation and requirements definition and modification that still takes time. That human side of coming up with a better idea, working through how it could function, going from a verbal design discussion to a technical set of specifications that you can program for. I think there’s still real time in that.
Once you get to the programming side of the house, there are some tool sets, testing tools, testing environments, and repeatable test data. That technology has shrunk down that total development time, but I don’t think it can necessarily eat into that timeframe that’s on a front end, to come with the idea and create something that’s viable that then you can handle the technical life cycle on. I think we’ve made some progress.
Within our organization, there are more good ideas than we have people. Most IT shops probably have that problem. You prioritize them and work through them in as smart a manner as you can.
What will be most important for you to accomplish for UHS in the next five years?
For IT, I want us to be flexible and responsive to the organization, which everybody certainly wants. But where I see our business and clinical priorities are increasing are focused on population health. We as an organization purchased an insurance plan. We are offering Medicare Advantage plans. We are working to provide narrow networks.
As we in the IT realm move from having an EMR deployed that we believe is relatively effective and physicians inside the four walls of our hospital using that relatively well, we need to then look outside of those four walls to the post-acute world. We need to look to managing that population health, providing the quality, and having the data and information to do all those things.
I don’t believe that’s necessarily materially different than other large providers. Working to align IT and making sure that we can effectively support good decision-making, quality improvement, and quality patient care delivery. Those are probably the most important things at the top of our list while continuing to be effective inside the four walls of the hospital.
Do you have any final thoughts?
I’ve enjoyed reading HIStalk for a long time. I think you bring a nice breadth of practical and honest information-sharing across the healthcare IT space. I appreciate what you’ve done. We hire kids out of college. We work to train them and grow them and try to create their interest in healthcare IT and you are a great source of information for that. I know a lot of others read what you have. You know I’m a long-term reader and I appreciate what you’ve done. You’ve made it very practical for people and cut through the BS, which is great.














































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…