Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…
News 11/7/14
Top News
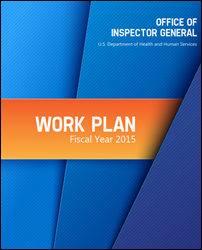
The 2015 work plan of HHS’s Office of Inspector General includes several EHR-related items beyond the usual Meaningful Use payment audits. OIG will audit the security of cloud-based service providers (including EHR vendors) and will review the downtime policies of hospitals. OIG’s future efforts “may consider the significant challenges that exist with respect to overseeing expenditures for health IT, the interoperability and effective sharing and use of health care data for medical care, and emergency preparedness and response.”
Reader Comments

From Zippy: “Re: Alameda Health System. The outgoing CEO removes the blame for its financial problems from Siemens Soarian.” The five-hospital system’s CFO told its board last month that its financial meltdown was caused by its $77 million Siemens/NextGen implementation, but the outgoing CEO says the system’s own managers — not Siemens — caused its problems. He specifically blamed two unnamed former health system executives.

From Sauerkraut: “Re: Siemens. The hearing aid business sold for more than twice the HIT business with lower revenues and the usual higher multiples of software businesses. Perhaps Ben Rooks can explain.” Singapore-based Siemens Audiology Solutions posted $860 million in 2014 revenue and just sold for $2.68 billion, or three times revenue. The healthcare IT business had about $1.2 billion in annual revenue and sold for $1.3 billion. I would guess the revenue multiples are based on profitability, market position, and future prospects rather than revenue. My impression is that Audiology is a turnkey business while Health Solutions is a slightly shabby fixer-upper with a reputation problem. There’s also the issue of having few qualified buyers, which would have kept the price down and given Cerner a clear shot at picking it up for a bargain basement price.
HIStalk Announcements and Requests
This week on HIStalk Connect: Microsoft and Jawbone unveil new fitness trackers, Microsoft in an attempt to capitalize on the digital health trend and Jawbone trying to differentiate itself in the emerging smartwatch market. Rock Health raises its next investment round and announces that it will fund accepted startups with a $250,000 seed round. Google revamps its Flu Trends platform to include CDC data in an effort to boost accuracy.
This week on HIStalk Practice: Healthcare buzzwords reach a "tipping point." DuPage Medical Group begins offering e-visits. The Eye Institute of Utah implements a new patient portal. Portland’s healthcare IT accelerator scene doubles. 5 O’clock Records rebrands. ONC launches a new innovation challenge. Thanks for reading.
I was clearing out space on my phone for an iOS upgrade, which forced me to decide which apps to delete since some are data hogs. My “can’t live without” survivors are below. What are yours?
- Yelp. Probably my most-used app.
- Motion-X GPS Drive. The best GPS I’ve used and the only paid app on my list, although it barely qualifies at 99 cents.
- Slydial. lets you call someone’s cell phone voicemail directly in case you just want to leave a message without talking to them.
- Airline apps. American is my most-used one.
- GateGuru. Helps me find decent airport food and check an airport’s flight board.
- OpenTable. I will sometimes make a restaurant reservation an hour before eating just to make sure there’s a table waiting, plus I trust the reviews and lists (I often also look at TripAdvisor).
- Uber. I use it occasionally, although I’ve been burned expensively a couple of times by the surge upcharge.
- Kindle. I don’t mind reading books on my phone’s small screen.
- Spotify. I subscribe to Premium so I can play music offline.
- Speedtest. I check Internet speed the moment I set foot in a hotel or house where I need to work, although usually I can’t do much more than swear and fret at Stone Age speeds (less than 3 Mbps down and 1 Mbps up).
Listening: new indie folk from Portland, OR-based The Decemberists, which sound a bit like R.E.M. Peter Buck has played on some tracks, although not on their pretty good cover of my favorite R.E.M. track, “Cuyahoga”.
Webinars
November 12 (Wednesday) 1:00 ET. Three Ways to Improve Care Transitions Using an HIE Encounter Notification Service. Sponsored by Audacious Inquiry. Presenters: Steven Kravet, MD, MBA, FACP, president, Johns Hopkins Community Physicians; Jennifer Bailey, senior director of quality and transformation, Johns Hopkins Community Physicians; Robert Horst, principal, Audacious Inquiry. Johns Hopkins Community Physicians reduced readmissions and improved quality by implementing a real-time, ADT-based encounter notification service (ENS) to keep the member’s healthcare team informed during transitions in care. Johns Hopkins presenters will describe the clinical, operational, and financial value of the ENS for care coordination along with its technology underpinnings.
November 18 (Tuesday) 1:00 ET. Cerner Takeover of Siemens, Are You Ready? Sponsored by HIStalk. Presenters: Frank L. Poggio, president and CEO, The Kelzon Group; Vince Ciotti, principal, HIS Professionals. The Cerner acquisition of Siemens impacts 1,000 hospitals that could be forced into a “take it or leave it” situation based on lessons learned from similar takeovers. This webinar will review the possible fate of each Siemens HIS product, the impact of the acquisition on ongoing R&D, available market alternatives, and steps Siemens clients should take to prepare.
November 19 (Wednesday) 1:00 ET. Improving Trial Accrual by Engaging the Digital Healthcare Consumer: How to Increase Enrollment with Online Consents and Social Marketing. Sponsored by DocuSign. Presenters: B. J. Rimel, MD, gynecologic oncologist, Cedars-Sinai Medial Center; Jennifer Royer, product marketing, DocuSign. The Women’s Cancer Program increased trial accrual five-fold by implementing an online registry that links participants to research studies, digitizing and simplifying a cumbersome, paper-based process. This webinar will describe the use of e-consents and social marketing to engage a broader population and advance research while saving time and reducing costs.
Acquisitions, Funding, Business, and Stock

Aspen Advisors will be acquired by healthcare management consulting firm Chartis Group, with Aspen’s Managing Principal Dan Herman joining the board of Chartis.

Allscripts announces Q3 results: revenue up 4 percent, adjusted EPS $0.06 vs. $0.05, missing analyst expectations for both. Shares dropped sharply in after-hours trading following Thursday afternoon’s announcement, down around 15 percent to levels not seen since early 2013.
Meanwhile, activist hedge fund Blue Harbour Group increases its ownership in Allscripts to 7 percent of the outstanding company shares, up from 5 percent. Blue Harbour Group says it avoids public shareholder fights by investing only in companies that welcome its ideas for unlocking value, happy to make money from share price appreciation rather than selling off parts piecemeal. Its Allscripts ownership stake looks like around $170 million worth, right in line with its stated sweet spot of $100-$200 million. Allscripts shares have dropped 7 percent in the past year and 38 percent in the past five years.
Healthgrades acquires digital marketing form COCG to enhance its strategic marketing services for hospitals.

Siemens reorganizes its remaining healthcare lines into a separate business as it suggested it might do several months ago, which won’t do much to squelch the rumors that it wants to sell of the whole package and get out of healthcare completely. Siemens just announced that it will sell its hearing aid business for $2.7 billion. It previously sold the HIT business to Cerner and its microbiology line to Beckman Coulter. Like GE, Siemens is putting big money into energy-related product lines.
Francisco Partners invests an unspecified amount in medication benefits network provider CoverMyMeds.

Shares in Merge Healthcare hit a 52-week high Wednesday, having jumped 33 percent in the past two weeks. Above is the one-year MRGE share price (blue, up 23 percent) vs. the Nasdaq (red, up 18 percent).

The Department of Defense awards Fulcrum a five-year, $13.9 million contract to update the systems used by DoD’s year-old Richmond, VA EHR testing facility and to open a second health IT testing center in West Virginia. Both will support DoD’s DHMSM EHR replacement project.
Global Healthcare Exchange will acquire Atlanta-based procurement software vendor Vendormate.
Etransmedia wins a multi-million award in its deceptive trade practices lawsuit against Allscripts. An arbitration panel ruled that Allscripts convinced Etransmedia to buy MyWay EHR licenses in advance to improve its own financial performance, but then “deliberately sabotaged” MyWay sales by retiring the product in October 2012, leaving Etransmedia holding millions of dollars in unsold licenses. Etransmedia has since developed its own Connect2Care product.
Sales
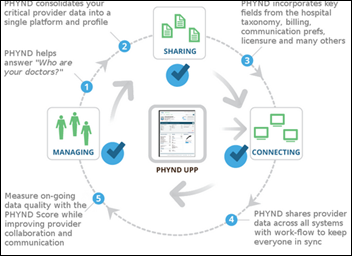
Beaumont Health System (MI) chooses PHYND’s Provider Population Management Platform for 20,000 physicians.
Rhode Island awards 3M the analytics contract for its All-Payer Claims Database that will aggregate claims and provider data to publish consumer-facing quality and cost information.
The VA will add two service networks to its Philips eICU program, expanding its ICU remote monitoring service to 1,800 beds.
People

Prison health provider Corizon Health names Andy Flatt (HealthSpring) as CIO.

Fogo Data Centers hires William Esslinger, Jr. (Esslinger Tech Law) as CEO and board member.

Peter Dolphin (PatientKeeper) joins Advanced Practice Strategies as EVP of sales.

National Library of Medicine Director Don Lindberg, MD will retire in March 2015 after more than 30 years on the job. He was also the first president of AMIA.
Announcements and Implementations
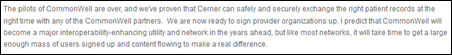
Cerner CEO Neal Patterson says in a blog post that the company will provide CommonWell services to its clients at no charge (after a “nominal setup fee”) through January 1, 2018. He adds that CommonWell will make its interoperability services available at a low cost, passed through from participating vendors to their clients. He emphasizes that CommonWell will never sell data.
A new startup, MD Revolution, launches RevUp, which allows providers to collect Medicare’s new $40 per month chronic care management payment through team-based monitoring of a user’s fitness device data. The HealthKit-enabled RevUp supports provider-user messaging, personal health coaching, and an unspecified level of integration with EHRs. It appears that the company provides all of the coaching services. Founder Samir Damani, MD, PharmD is a Scripps cardiologist. Also on the executive team is CIO Jean Balgrosky (former Scripps SVP/CIO) and SVP of Business Development Parker Hinshaw (founder of maxIT). The company’s page also neatly summarizes the requirements to collect the monthly payment that starts in January 2015 — 20 minutes of non face-to-face care of Medicare patients with two or more chronic conditions. .

Blood Bank of Alaska implements Mediware’s blood center management and donor recruitment systems.
Government and Politics
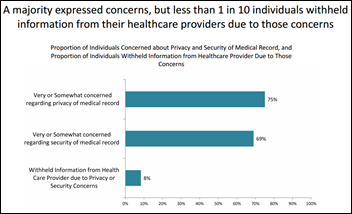
An ONC survey finds that most consumers (75 percent) are concerned about the privacy of their medical records whether paper or electronic, but few (less than 10 percent) are worried enough to withhold information. Three-quarters of respondents want their providers to use EHRs and share their information with their other providers. Survey pluses: it was a random-dial telephone survey that removes online-only and self-selected participant bias and it had a good number of responses, but the folks willing to take a cold-call survey may not be representative. Survey minus: it was conducted last year.
CMS postpones its eHealth Summit, scheduled for December 5, until further notice.
Innovation and Research
The Wall Street Journal highlights companies that are working on diagnostics that can detect Ebola quickly, including BioFire Defense (which I wrote about quite a bit last week), CorGenix Medical (a $15 non-instrument system that works like a home pregnancy test), Chemnio Diagnostics Systems (a $10 finger-stick test), and OraSure Technologies (which is considering development of a mouth swab-based test like the one it offers for HIV).
A nine-hospital study finds that use of a structured patient handoff procedure among medical residents was associated with a 23 percent reduction in medical errors and a 30 percent drop in preventable adverse events. Residents used a mnemonic-driven checklist for both oral and written handoffs.
Technology

Microsoft announces free versions of Office for the iPhone and updated versions for the iPad, with Office for Android coming soon.
Qualcomm Life Director of Business Development Kabir Kasargod urges wearables developers to move from activity trackers to the real healthcare industry:
Go from the children’s table to the grown-up table. If you’re serious about this, embrace the FDA. Learn how HIPAA works. Make sure it’s connected to the [electronic medical record] and that all the health laws are observed. There’s a tremendous dearth of innovation here. I would move away from fitness and go hardcore into health. That’s where the money is.
A Pennsylvania business paper profiles Pittsburgh-based Health Monitoring Systems, whose service monitors hospital EHR information to provide real-time outbreak information to public health departments.

PayPal co-founder and early Facebook investor Peter Thiel says he is skeptical about healthcare IT, big data, and cloud computing.
Epic responds to Cerner CEO Neal Patterson’s calling the company “immoral” for being an interoperability “black hole” among EHR vendors at Cerner’s user group meeting. Epic’s statement:
Epic is No. 1 for interoperability performance as ranked by actual users surveyed by the highly respected firm KLAS. Epic can interoperate with any other electronic health record that meets government standards, regardless of vendor. We support open standards rather than private platforms such as CommonWell that further privatize and monetize exchange of health information.

A Health Affairs blog post by MedStar Health’s influential informatics expert Peter Basch, MD says the Meaningful Use program is impeding interoperability by its rigid, metric-driven approach that fails to meet the needs of providers and patients. He adds that EHRs don’t work well for advanced primary care models that emphasize chronic disease management and care coordination and observes that today’s version of interoperability makes matters worse by more widely spreading clutter-filled summary of care and visit summary documents.

S&P downgrades the bonds of Wake Forest Baptist Medical Center (NC) because of large receivables write-offs and the high ongoing expense of its Epic system.

PeaceHealth (WA) ends affiliation talks with Ocean Beach Hospital (WA), with PeaceHealth’s CEO saying his organization is too busy and too far over budget on its Epic implementation to take on a new hospital.

The tweets of Scripps cardiologist Eric Topol, MD have the highest signal-to-noise ratio of just about anybody even though he gets a bit app-happy at times, so I enjoyed this interview, in which he made some interesting points. He’ll be delivering a keynote presentation at the Digital Health Conference 2014 November 17-18 in New York City.
- Patients will help diagnose and monitor themselves using algorithms, leaving doctors to focus on treatments.
- Continuous monitoring will allow patients to stay at home, reducing hospital usage.
- Virtual visits can help with the difficulty involved in getting a PCP appointment, which he says requires a six-week lead time in Boston.
- A major shift to virtual visits will reduce trips to the doctor’s office.
- Patients will bear much of the responsibility and cost of their health.
Weird News Andy expects this story to fill a void. A bus driver in Egypt attempts to dodge a mandatory urine drug screen by submitting a sample from his wife and is surprised to hear from officials, “Congratulations, you’re pregnant.”
Sponsor Updates
- RazorInsights publishes a company video, a brilliantly done history that includes founder interviews.
- Surgical Information Systems names Indiana Orthopaedic Hospital (IN) as a Center of Excellence.
- HCI group posts “Meaningful Use to Meaningful Care” by William Bria, MD and Robert Steele, RN.
EPtalk by Dr. Jayne

The November 30 deadline for eligible hospitals to report for the 2014 Medicare EHR Incentive Program is fast approaching. I haven’t been on the attestation site lately, but I am told that the 2014 Flexibility Rule options are available. If that doesn’t work, you can still apply for a hardship exception, but if you’re just now figuring out that you need one, I feel for you.
Speaking of Meaningful Use, several providers at my hospital forwarded links to articles about the dismal attestation statistics, demanding that we consider “stopping this nonsense” and “get back to practicing real medicine.” They’re not alone, although most national groups are focusing on shortening the reporting period for 2015 and adding additional flexibility. CHIME, the AMA, MGMA, and of course HIMSS are among the loudest voices.
With the Flexibility Rule slowing some organizations’ upgrade schedules, CMS also made some updates to the final 2015 Medicare fee schedule. Primary care practices can report Chronic Care Management codes on whatever certified EHR they were on as of December 31 of the previous calendar year, rather than being required to use 2014 CEHRT. Additionally those services can be billed using a CPT code instead of a G code. I’m not sure why that’s an advantage, but provider groups seem happy about it.
If you have nothing else to do this weekend, it’s 1,185 pages of glory and includes summaries of comments received while it was under consideration. Comments are being accepted through December 30 and it goes into effect January 1, so read up. Any document that includes five and a half pages of acronym explanations is bound to be a hit.

I’ve been recovering this week from a Continuing Medical Education conference. I’m not a huge fan of Las Vegas, but it seems like a lot of conferences are held there. After learning about dermatological diseases in a drab hotel ballroom for two days, a conversation in the row ahead jogged my memory that the NextGen One user group meeting was starting at the tail end of my trip. A quick call to Bianca Biller confirmed that she was also in town, which improved my spirits. In addition to being one of the smartest revenue cycle experts I know, she is also the most fun.
She warned me that tight security was keeping non-registered people out of the conference center, but was able to score me a pass to the Navicure client event on Monday at the Hard Rock Live. I was feeling a little giddy when I got carded at the door until I realized they were carding everyone. We arrived fairly early, but the party was already in full swing. The Atlanta-based band was fantastic and it was fun to watch medical practice folks kick back to Journey and James Brown covers. Since MGMA had wrapped up a few days earlier, she said there were a lot of vendors staying over, so we headed out to hit a couple more get-togethers. We ended up with the obligatory wild and crazy taxi ride, during which Bianca received a marriage proposal from the cabbie.
We dialed it down a notch and stopped by the Intelligent Medical Objects suite at Mandalay Bay for a glass of wine and some much-needed time off our feet. There we ran into one of Bianca’s nurse informaticists, who lured us to the casino with the promise of riches to come. I was content to watch others gamble and to do some people watching – the number of folks still in Halloween costumes several days after the fact was pretty entertaining. Although I missed MGMA this year, I felt like I at least got my party fix and that will hold me until HIMSS.
My new nurse friend was the big winner of the night, where I was lucky to walk away with the same $20 I started with. The Cerner conference was also this week, but I haven’t heard anything about it.
Do you have conference pictures or a crazy taxi story? Email me.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.






I stopped using Yelp after too many examples of them trying to extort my clients, a business model which they deny or brag about depending on whether they are talking to small businesses or investors.
As for travel apps, I love Hipmunk and TripIt. Both on the front page of my phone.
WNA. Fill a void. Cute.
Tim, I think you totally nailed the reasons for the pricing differential. Audiology likely had better growth and, given the world’s aging population, better growth projections. Health Solutions, in contrast, had minimal growth during the biggest boom the sector had ever seen. A business is ultimately worth the present value of its future cash flows, and growth is the most important variable in that analysis. By the way, the app I’d add to your list is Pocket, to save articles for easy off-line reading.
Ben
Neal is attempting to create a false narrative about Epic. He could have easily put his energy behind the NwHIN protocols managed by HealtheWay and been exchanging 10s of millions of transitions of care documents like Epic currently is had he wanted to.
Neal should come clean and explain why he waited so long to “discover the value of interoperability”.
Foreign data exchange is free for epic clients? I’ll be.
How can CommonWell say they won’t sell data when RelayHealth’s own business plan and legal terms say they can do exactly that? McKesson isn’t giving this stuff away for free. Sounds like the CommonWell membership either doesn’t understand what’s going on or are trying to intentionally mislead.
Looks like Allscripts while requiring their staff share rooms at ACE due to their worsening financial picture might need to consider bus passes instead of airline tickets for travel next year.
It’s also interesting that Cliff Robins the CEO of Blue Harbor ” is a member of the Board of Overseers and Managers of Memorial Sloan Kettering Cancer Center and currently chairs its Finance and Funding Committee”. It would seem like a difficult conflict of interest if Allscripts were to come up in any decisions. It’s pretty unclear what Blue Harbor sees in Allscripts given how much Allscripts’ shares continue to drop, but it may have to do with their very large backlog..
Personally, I think Allscripts is well on their way to bankruptcy, but it’s for the right reasons. They don’t deliver on their commitments. Ironically, it’s not that they don’t have a solution. It’s that they have far too many solutions and they can’t afford to maintain so many of them. They can’t push clients to change or they’ll go find the other better solutions out in the marketplace. Their large amount of looming debt will be the end of Allscripts, but it might take a few years and their zombie EHRs can survive on.
Hey #NotSoFast, I work for Cerner and usually try to stay out of this stuff, but I feel like I have to respond to your comments. NwHIN was evaluated and had strengths and weaknesses. There were serious concerns about how it would match patient identity across providers, how it would locate the patient’s external records, and there was no easy way to manage state-by-state consent rules. I believe CommonWell was specifically designed to address those three things – identity, record location and consent.
I also feel like I need to speak up about your false implication that Neal has only recently developed an interest in interoperability. Neal has done a lot to promote interoperability over the past 10 years. I remember ~2005 when he invited practically every vendor in the industry to co-fund a study on identity issues relative to interoperability. You know who didn’t join in? Three guesses. If Neal isn’t interested in interoperability, why would he let David McCallie serve on the HITSC for years and actively promote it? Why would he allow Cerner programmers to donate more than 180,000 lines of open source code to the Direct Project? Why would he offer personal testimony on Interop? Why would he help start CommonWell? Like it or not, he has a serious, personal interest in interoperability. You may not believe it, but I do because I’ve seen it first hand.
On the other hand, you have Judy Faulkner commenting to Bloomberg Business Week in 2009 that it “doesn’t work when you mix and match vendors.” What did she mean by that? Then she tells the New York Times this year that she’s been seriously pursuing interoperability since 2004. Who is revising history? Care Everywhere (Epic to Epic) was developed around that time as a creative way to help Kaiser sites talk to Kaiser sites because they couldn’t scale to a single instance. Kudos for the creative solution, but don’t make it sound like you were trying to create vendor to vendor interoperability back then.
“Dubious” information indeed. CommonWell’s contract with RelayHealth specifically prohibits them from reselling any CommonWell data. CommonWell’s members fund the service directly, not from selling of any data.
And CommonWell was created to address many of the shortcomings of the NwHIN’s constrained architecture, including the lack of a robust way to identity patients, and the lack of any automatic way to know where a patient’s record exists.
Re:…OIG will audit the security of cloud-based service providers (including EHR vendors) and will review the downtime policies of hospitals
I’d be laughing silly if this wasn’t just pathetic. OIG wants to review hospital downtime? I think we all would be better off if they focused on the FAA. The Chicago system gets knocked out and it takes two weeks to bring it back up!
…and since the big topic of the season seems to be interoperability…do you know that the each major FAA center runs different systems that do not talk to each other, and they are so different that you can’t take a flight controller from NY and have him work in Chicago without weeks or retraining!
Interoperability will be much easier when we are all on ICD-10-CM late next year. To get an idea of what’s to come go to:
http://www.slideshare.net/BobRudy
Yes, TPD is now out of the closet but not available for interviewing until after 10/1/2015!
@Reader Beware. “What did she mean by that?” Let’s reference the article instead of just quoting without context:
http://www.businessweek.com/stories/2009-04-22/the-dubious-promise-of-digital-medicine
The quote “doesn’t work when you mix and match vendors” (which is common ammunition in this debate) was specifically in reference to inpatient medication orders to an inpatient pharmacy system. The concern is with patient safety and not a stance against interoperability.
@David McCallie – Post the contract terms. Following dubious comments, RelayHealth’s online terms certainly suggest that they can sell aggregate data, provider prescribing information, etc. (see, https://app.relayhealth.com/legal/LegalContent.aspx?docID=privacy&lang=en-US). There are also big holes that would let them seemingly market to subscribers and providers.
@mmm – because RH can sell data as it relates to ePrescribing, does not mean it governs all their contracts. Last I checked, linking terms across different contracts is not legal business practice. Thinking logically, why would CommonWell ever allow that to occur, knowing that even a glimpse of that kind of business model would sink it? It is not logical, so stop inserting FUD.
Also, why be so negative on CommonWell? If it is success, a longtime industry problem might be solved. If it is not, then you can brag about how you knew it would be all along.
Personally, i would like to try to solve a problem and fail vs. sitting on the sideline and trying to put sticks in the spokes.