S. Claiborne “Clay” Johnston, MD, PhD is dean of Dell Medical School at the University of Texas at Austin. Campus construction will be completed in May 2016 and the first medical school class will begin studies in June 2016.

How have medical schools have changed over the last 20 years and how will the Dell Medical School will be even more different?
Medical schools are changing, and I think a little more rapidly now. They certainly haven’t changed as much as they should have.
The one realization is that lectures don’t work so well. There’s a lot more emphasis on flipped classroom type approaches to teaching, small group learning, that kind of thing.
More recently, too, there’s a greater appreciation of the fact that – the way I learned was memorization focused, just cram all this knowledge. The reality is that information is cheap today. The resources available to physicians are much more accessible and are generally more accurate than memory for things that aren’t used frequently. Therefore, the need to memorize so much stuff is really not there.
There’s been some de-emphasis of that memorization task and more about how we find the data that we need, how we integrate that data, and how we use it solve problems. Those are some of the broader trends that are going on.
Obviously we want to take advantage of those, but also we’re coming without an existing curriculum. We have a lot more freedom than existing schools, where you always have people who defend the status quo and created that beautiful lecture set on the Krebs cycle and they’re just not going to let it go. We don’t have that, so that gives us a different perspective.
For us, it’s more about, what is it that we want from health and from healthcare as a society? Then, what is the appropriate role of the physician in that ideal vision of what the health system should look like? Then, how do we provide the best training to meet those needs, particularly given the problems in the health system? That completely opens your eyes in terms of thinking about, what is the skill set?
From our perspective, physician leadership is a big problem. Being able to look at system-level problems, work in teams, and use technologies and other new approaches to solving these system problems creatively. Those are some of the key things that physicians ought to be involved in. Not just to not resist them, which is a common problem now, but to actually help to lead them.
That’s what we’re doing. We’ve got a curriculum that’s very much designed around training these physician leaders of the future.
A significant percentage of medical school graduates either don’t follow with a residency or they take a non-patient care role after using up a class spot and the educational subsidy. How do you set reasonable expectations, especially as prospective students hear about burnout among practicing physicians?
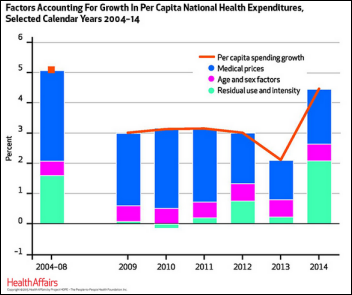
We need to focus on why those physicians are burned out and look at the systems that have been put in place that have led to that burnout. One of the dysfunctions of the fee-for-service system is that it does not compensate people well for things like office visits or the cognitive aspects of medicine. It does compensate well for procedures. Over time, the cognitive aspect reimbursements have been ratcheted down for physicians, so they’ve had to see more and more patients.
Then electronic health records were introduced. Their primary function today is billing. They have eroded even further the meaningful time that doctors spend with their patients.
Those are just a couple of examples, but important ones for how we’ve made jobs like primary care really unpleasant. There’s very short visits — the average office is now 12 minutes. Up to half of that could be spent just documenting the visit in a very dysfunctional electronic health record.
The reasons that docs go into medicine have been lost. Having those meaningful, important discussions and time with patients is much more difficult today.
How, then, do we change the system so that docs can spend more time with patients and maybe work with patients in whole new ways, you know, like email? It’s used in every industry. Why not allow patients to email their docs and make that part of the job of a physician to manage patients by whatever technologies make the most sense?
What do we tell our students? Well we tell our students, it’s your job to keep people healthy and to get them healthy again when they’re not. In the traditional approach, that was to be done in clinic visits and in ORs and emergency rooms. Now, open your eyes up and think about how you could do that best. If I gave you a panel of 3,000 patients to take care of, what would you put in place to make sure that they’re as absolutely healthy as they could possibly be and that you have meaningful discussions with them?
You probably build a team around yourself. You would use technologies. OK, show me what that looks like. Tell me how we can build that and that there are ways to get paid for it.
Medicine needs to evolve that way. Then the physician burnout also can go away because that perspective is just as important to fixing the health system.
Texas makes a lot of headlines related to telemedicine. Will telemedicine and other non-face-to-face technologies be part of your curriculum?
Yes. They need to be. To say that those technologies shouldn’t be important in the delivery of healthcare is just so short-sighted.
So many of the things that are currently addressed in office visits could be addressed much more readily by email. That opens up the possibility of more frequent interactions that can help patients who wonder, for example, whether a side effect they’re having is related to a new medicine they started. If we do that, then the office visits can be much more meaningful because you don’t need as many.
There are definitely ways to easily imagine to push things forward, including telemedicine. Yes, we need to then engage our students in that.
Do you think the low-pay, high-workload model of medical residency that’s funded by federal taxpayers still makes sense?
It’s a strange model, but the reality is that the residents have two functions. They provide real work and help, which is why we feel like they deserve some salary, but they are primarily learners. They’re there to finish up their training. That’s in the best interest of society, to have that.
Who should pay and how? It ends up the federal government actually pays for the minority of residents. Most are paid for through the hospital system. So it’s really, truly a strange, hybrid system. Could there be a better system? Probably. We do need to pay them something, but they don’t justify getting paid at the same level as physicians who have finished their residency.
Where in a physician’s career are the majority of concepts and treatment methods developed? How can a physician who has been out of school for 20 years remain as current as one who graduated five years ago?
I think that’s a learned behavior, not a deterministic one. I don’t think there is a point at which physicians are more difficult to teach.
Physicians in general love their independence and love to be the final say in whatever it is that they work in. Traditionally, they’ve not been so comfortable changing over time. But honestly, if you look at systems, there have been some systems that have changed dramatically and pushed more to evidence-based medicine quite comfortably, where the physicians — a whole variety of different types within that system — move forward in lock step with the evidence. A good example is Kaiser Permanente.
I think there are processes and ways of working together and teaching each other and continuing to focus on education that can encourage those behaviors.
How much of medical practice is based on evidence and whose job is it to incorporate it ongoing?
Most of what we do in medicine, there’s not solid, high-quality evidence to support. It’s done because it seems reasonable, or it’s done because it’s always been done, that way or it’s done because the science underneath it seems to probably make sense, or it’s done because another patient was treated that way and did fine so it’s probably fine to continue. High-quality evidence — where you’ve got, for example, randomized trial data — that’s a minority of the decisions and weighty decisions that physicians make.
Currently it isn’t clear whose responsibility that is. I would say that physicians ultimately have the responsibility to practice based on the evidence, to stay current and to stay true to the evidence. But it is extremely difficult to do that in standard independent practice because things move so quickly and because it requires more adjudication than just reading papers. You have to really look at the papers in light of other evidence. You have to read the papers deeply. You have to think of the alternatives.
That works better when groups of physicians and others come together to decide what standards they will practice under. Then the system really does have some responsibility for making sure that this can happen better.
In our case, we do feel like this is a responsibility that we have back to this community — to work with the excellent physicians here, but help them to stay excellent forever. How will we do that? We’re looking at ways. They need incentives to stay current. How do we work in creating those and then create those educational opportunities and also those arenas in which they can review and judge and decide on evidence that they should all follow.
How will you teach students to respect both traditional, large-scale, well-developed studies –which are often published only if the for-profit company sponsoring them likes the results — versus self-interpreted smaller data sets that will be available almost everywhere?
Obviously you have to teach them a lot more about how you look at data and what the issues are with it. The spectrum that you just described — be suspicious about Phase 2 clinical trials. Phase 3 clinical trials, those are so expensive that you have to publish it results from a Phase 3 clinical trial. That’s less likely, but the early-phase clinical trials — that is an important source of bias, as you say.
The individualization of care is the thing that was implied by your second question, you know, "These 10 people who look like you did well" — you don’t get that information necessarily from a clinical trial. You get it from a broader spectrum of folks who are eligible. They might do some sub-group analysis, but they’re never powered to adequately show a difference by sub-group.
Then obviously the problem with that evidence is that it’s weak. Maybe it’s luck that they all did well. Maybe doing well is an expected outcome, so it would be rare to actually have something bad happen. Maybe they were selected in a certain way that made them all do well. You can’t know.
How do you teach that? Data is going to be all around us and that’s a wonderful thing, because it gives us all kinds of additional information that if we’re careful, can be extremely useful in improving care, improving outcomes for our patients, keeping people healthier.
We have to expose our students to that throughout the curriculum and get them involved in projects in which they’re using data to solve critical health problems. That’s what we do. We take them out of their rotations and they work for nine months in innovation and leadership blocks. They solve real health problems.
If the goal is to make our overall population healthier, what’s the right blend of what you teach doctors to do as physicians in practicing medicine versus the public health approach that might include areas such as housing, education, income, or personal behavior?
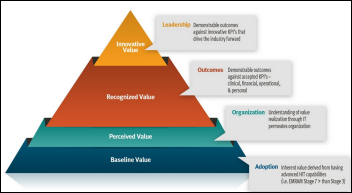
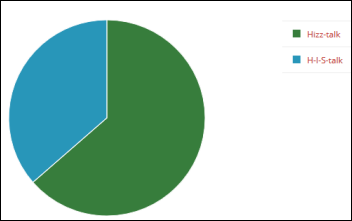
It’s important for physicians to understand the full spectrum. Healthcare only accounts for 20 percent of the potential to improve health. Eighty percent of it comes from all that other stuff that you mentioned. If the goal of the physician is to keep people healthy, they need to be aware of that 80 percent and also understand how to integrate that into their practice or into their broader, system-level solutions to health problems.
The question is, where you draw the line? Are physicians going to be proponents of income equality because income differences lead to health issues? No, probably not. It’s not about getting to the political and the governmental aspects of the predictors.
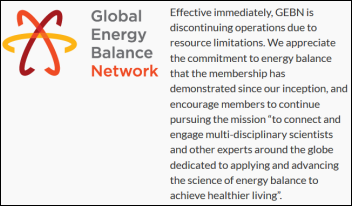
What if it is about diet and exercise? Those behaviors, or taking your meds — those are important things in which physician interventions or system-level interventions that could include a physician on the team are important things for the health system to focus on. It makes sense for physicians to have roles in those areas.
That stuff becomes critical to our curriculum. It is far more effective and can be cost saving to keep people healthier than it is to treat them once they are sick. The highest paid health professionals are physicians. Why shouldn’t they be engaged in that? Why shouldn’t they be helping to guide it rather than just been focused on the patch-up work?
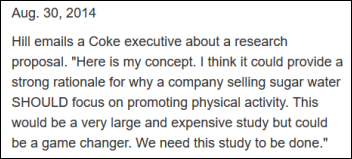
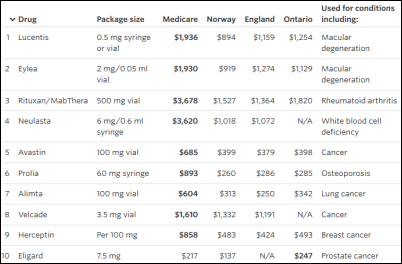
Being in Austin and being associated with Dell suggests a focus on drug and technology research, but the product of such research is usually commercialized expensively without necessarily improving overall outcomes. How do you balance the human need for research with the desire of medical companies to make big profits and raise healthcare costs even more?
That’s one of the key reasons I’m here. I was the associate vice-chancellor of research and responsible for the Clinical and Translational Science Institute at UCSF. Our job was to accelerate discoveries from the laboratory out into health improvement.
The reality was just as you said. We could keep doing that, but they’re going to be always maximally priced. They never lower cost, but they always elevate cost of care. That’s true — they have control of the pricing, so they price it to the point that it’s somewhere between $50,000 and $200,000 per quality-adjusted life year. That makes sense from their perspective to do that, but it just contributes to the problem where you’ve got so much cost that you can’t really afford innovation any more.
That to me suggested, gosh, we’ve got to find a new way. What we’re trying to do is set up the health system to embrace and look for solutions that drive down cost. I think that we’ve left a lot of fruit low hanging on the trees because we haven’t had that perspective.
One example is antipsychotics. We know, as we’re looking at expensive health problems in Austin, the homeless — some of whom are schizophrenic — are a huge burden. Their outcomes are just terrible. It’s hard to get them to take their meds. It’s part of their disease. But if we had long-acting drugs, that could dramatically reduce the cost compared to what we pay today, with drugs that have to be given daily and are probably taken weekly if you’re lucky. That is an example of how taking a different perspective opens up new approaches, also for research.
Our hope is to integrate those perspectives throughout the research channels that we’re developing . We know we’ll have discoveries that come out and cost $200,000 per quality-adjusted life year, but our focus is to really concentrate on those that actually can reduce cost and improve outcomes.
It’s easy in the medical trenches to become disillusioned with what physicians are being asked to do, what issues they face that are beyond their control, and how the US healthcare system compares to countries that structure things differently. What will you tell students they need to do to improve it?
This is the absolute best time to go into medicine. We’ve gotten a point where we’re at the precipice — where physicians are unhappy, patients are unhappy, and we’re still costing the country a huge amount, 40 percent more than Switzerland and that’s the next closest country. We’re at this crisis point. That means this is the time at which we can really push forward the creative solutions to healthcare.
What are those solutions? Some are easy to imagine, and as soon as we change the payment schemes, they become obvious and we’ll catch on. The payment schemes are changing. Some are not so obvious. It’s early days in what will be a really exciting point in medicine. I don’t think practicing medicine will look like it does today even 10 years from now. I think it will be much more technology enabled, much more data enabled. The physician will be a true partner in improving health. That transition will be wonderful for those in practice and for the population.














































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…