Top News

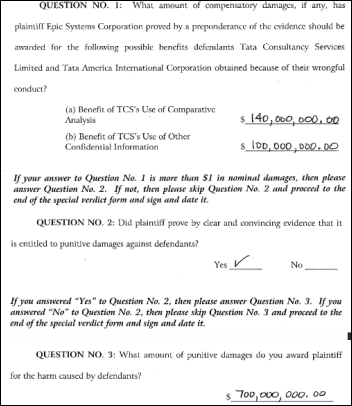
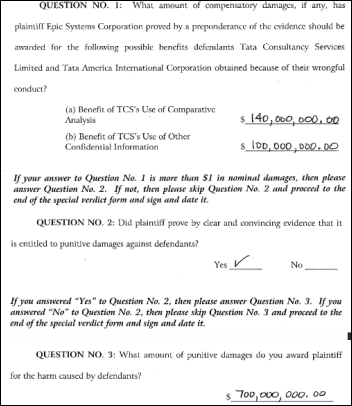
Epic’s trade secrets lawsuit against India-based Tata Group concludes with the Wisconsin jury awarding Epic $940 million in damages. The verdict calls for Tata to pay Epic $240 million for the benefits received by its subsidiary (Tata Consultancy Services) from stealing Epic’s trade secrets plus another $700 million in punitive damages. The lawsuit said employees of Tata posed as Kaiser Permanente employees to gain access to client-only Epic documentation that Tata planned to use to develop a competing product.
Tata says it will appeal, claiming it did not use Epic’s information in the development of its Med Mantra system. The company says its developers never saw Epic’s materials.
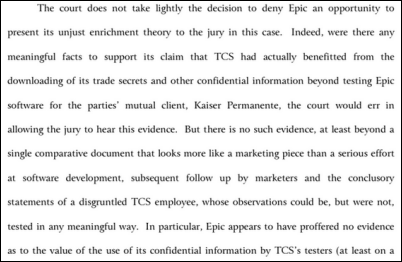
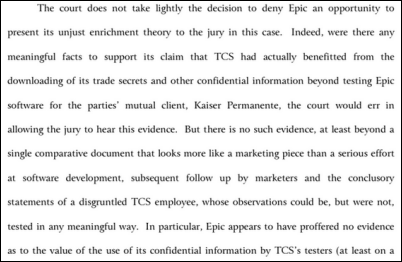
The $940 million judgment will certainly be reduced by the presiding judge, who chided Epic’s damage claims before the hometown jury’s verdict was announced. He observed:
- Epic didn’t provide the court with the method it used to calculate its damage claims until after the trial began, which could cause those claimed damages to be excluded.
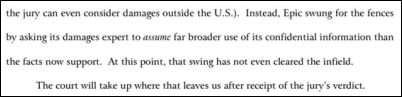
- Epic hasn’t proved that it was damaged to the extent claimed or that Tata benefited to that degree, explaining, “The complete lack of evidence tying the costs of Epic’s research and development efforts to any commensurate benefit to TCS dooms its methodology.”
- Epic claims that the biggest benefit to Tata wasn’t stealing development secrets or source code, but rather then value of “what not to do” that is “spread throughout the enterprise.”
- The only evidence provided of how Tata used Epic’s information was a side-by-side marketing graphic comparing Epic’s products and Tata’s Med Mantra, with the claimed damages “based on Epic’s speculation that the confidential information is sitting on a shelf somewhere to be used immediately after this trial ends.”
- The judge says such “future use” assumptions are more appropriately addressed via injunction to prevent such use rather than a speculative damage award. He also noted that Tata has mostly failed in its attempts to penetrate the US market and that an injunction would reduce its chances even further.
Reader Comments
From Verisimilitude: “Re: HealthTap access on Facebook Messenger. I’m not sure how much privacy protection people are given. I’m no HIPAA expert, but my guess is there’s a big fat release and arbitration clause buried in a EULA someplace.” Video visit vendor HealthTap offers a free chatbot Q&A service using Facebook Messenger rather than real-time access to actual human doctors. HealthTap’s terms of service are indeed voluminous and include an arbitration clause. I tried the Facebook service and it was worthless – all I received within several hours of asking a simple question was a list of previously answered similar questions (that weren’t similar at all) and a link to HealthTap’s site.

From Nasty Parts: “Re: NextGen. A major re-org was announced as Rusty Frantz continues the Pyxis-ization. It has dissolved its silos into ‘One NextGen,’ and as a result, multiple senior execs are transitioning out.” Unverified. Nasty Parts named several VPs who are leaving and says there’s “much more change to come.” I’m not sure that’s a bad thing. Frantz has been CEO at Quality Systems for almost a year, so he’s had time to think through what needs to be done.

From Maury Garner: “Re: Sandlot Solutions. You reported their closing. I ran across this lawsuit filed by one of their customers to prevent Sandlot from destroyer their data immediately after copying it for them. The article describes Sandlot Solutions as insolvent and closing.” I don’t have a Law360 subscription to see the details, but your description of their article seems accurate.
From Rebuttal: “Re: IT departments. In the last 5-6 years, I’ve noticed that organizations I’ve interviewed with seem to care more about what I can bring rather than having a balanced interest in our mutual needs. It seems that complex vendor systems have turned IT departments into sweatshops.” It may well be that the high cost of vendor systems has raised provider expectations that new hires will immediately pay off in task-specific, product-specific ways with implementation and optimization. It’s also probably true that for-profit companies in particular aren’t as interested in investing in mutually satisfying long-term relationships with new hires who might bolt once they’ve built their resumes. Lastly, I would speculate that the rise of the 1099 economy has redefined the work environment on both sides to a “what have you done for me lately” mindset. I’ll invite readers to weigh in.
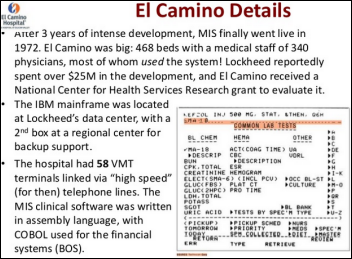
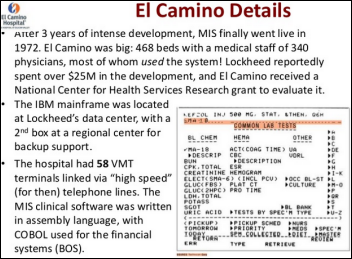
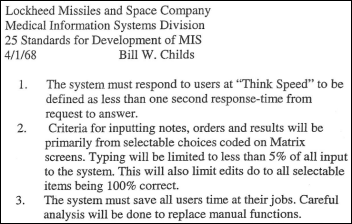
From Vince Ciotti: “Re: Bill Childs. Just to make sure readers appreciate how progressive Bill and the pioneering team at Lockheed were, they also came up with:
- CRTs (cathode ray tubes). They called them VMTs (Video Matrix Terminals) in an era when most systems relied on keypunch cards and green bar paper reports for input and output.
- Light pens. The precursor (punny?) to today’s mice, an idea Jobs and Wozniak copied from Xerox PARC. Clinicians using MIS only had to click on the VMT screen instead of trying to learn touch typing.
- Screen building. Lockheed (later TDS) called it matrix coding, but teams of clinicians designed their own order screens rather than implementing a model designed by programmers who never saw a patient.
Feeling nostalgic? You can read more in Vince’s HIS-tory series that ran on HIStalk for several years. I immersed myself back into them over the weekend as a guilty pleasure.

From Rocket J. Squirrel: “Re: Erlanger. A rocky start to the Epic project. The consultant evaluation ignored the lowest-cost option and the CTO who made the decision is gone after eight months. Totally behind on project staffing and already six months delayed.” Unverified.
From Alpha Surfer Dude: “Re: Dr. Brink’s article on radiology benefits managers. See what’s going on in Hawaii if you want to learn why this is so topical.” A Readers Write article by James A. Brink, MD, vice chair of the American College of Radiology and Mass General radiologist in chief, criticized plans to require pre-authorization of advanced imaging. He says electronic guidelines can help ensure the appropriateness of such orders in real time. Insurer Hawaii Medical Service Association (HMSA) made outpatient imaging pre-authorization mandatory in December 2015, leading doctors to complain that care is delayed and that tests are often denied. Newly proposed legislation would hold insurance companies rather than providers liable for any civil damages resulting from pre-authorization delays. HMSA requires doctors to contact Arizona-based radiology benefits management company National Imaging Associates (a subsidiary of publicly traded Magellan Health), leading one Hawaii doctor to complain, “Do you want those decisions to be made by offshore non-experts?” Taking the counterpoint, it was widespread ordering of medically questionable imaging studies – sometimes by doctors with a financial interest in the machines used to perform them — that created the need for such restrictions in the first place. As they say, one person’s excess cost is another’s livelihood.
HIStalk Announcements and Requests

Only 12 percent of poll respondents have had a virtual visit in the past year, although 81 percent of those who did were satisfied. New poll to your right or here: would you be worried about your privacy if you were being treated for depression by an EHR-using provider? Please explain after voting.

Mrs. May, a first-year teacher from Florida, says her special education classes are using the STEM and engineering kits we provided in funding her DonorsChoose grant request not only to learn about science, but also “how important communication is to get to the finish line.”
Also checking in is Mrs. Johnson from Oklahoma, who says her elementary school students “are loving the hands-on materials that you have provided for us. I no longer hear any complaints when I ask them to go to their math stations because they are not only enjoying them, but they are practicing their skills.”
Last Week’s Most Interesting News
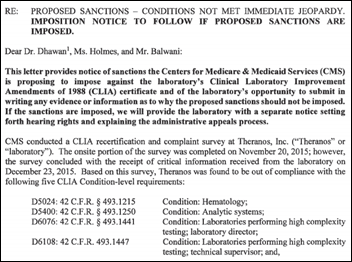
- CMS threatens to ban Theranos CEO Elizabeth Holmes from the blood testing business for failing to correct problems that CMS had previously called to the company’s attention.
- Kaiser Permanente launches a database of data contributed by its members that researchers will use to study how genetic and environmental factors affect health.
- CMS announces a five-year pilot of CPC+, a medical home model that requires the use of a certified EHR, and for one of the two tracks, a signed agreement from the practice’s EHR vendor that it will support the capabilities needed.
- Kaiser Permanente releases a summary of what it has learned from having a large number of its patients use a portal, disclosing that one-third of its PCP encounters are now conducted by secure email with expectations that the percentage will increase significantly.
Webinars
April 26 (Tuesday) 1:00 ET. “Provider-Led Care Management: Trends and Opportunities in a Growing Market. ”Sponsored by HIStalk. Presenter: Matthew Guldin, analyst, Chilmark Research. This webinar will provide a brief overview and direction of the provider-led care management market. It will identify the types of vendors in this market, their current and longer-term challenges, product capabilities, partnership activity, and market dynamics that influence adoption. It will conclude with an overview of key factors for vendors and solutions moving forward.
Contact Lorre for webinar services. Past webinars are on our HIStalk webinars YouTube channel.
Acquisitions, Funding, Business, and Stock

Cardinal Health-owned NaviHealth, which offers post-acute care utilization management services, will acquire care transition software vendor Curaspan Health Group.
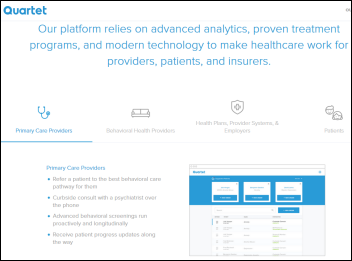
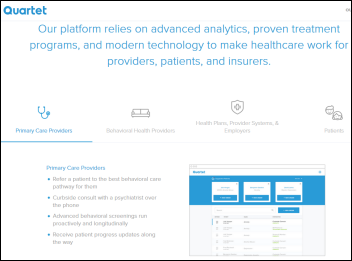
Behavioral health software vendor Quartet Health raises $40 million in a Series B funding round led by GV (the former Google Ventures), increasing its total to $47 million.
People

Mark Cesa, whose long healthcare IT sales career included stints with Baxter Healthcare, GTE Health Systems, Eclipsys, Tamtron, QuadraMed, Allscripts, and Napier Healthcare, died of cancer April 1. He was 61.
Announcements and Implementations

Voalte announces that it signed 125 hospitals in its fiscal year ending March 2016, increasing its customer base by 83 percent.
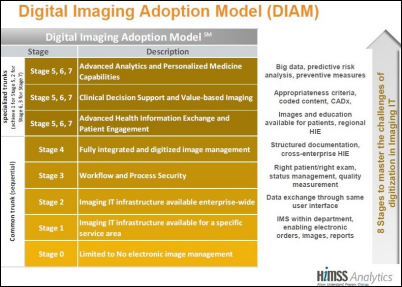
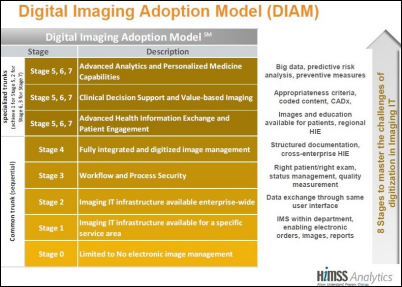
Imaging IT expert Herman Oosterwijk posts the Digital Imaging Adoption Model that was announced a few weeks ago by the European Society of Radiology and HIMSS Analytics.
Government and Politics

VA CIO LaVerne Council says in Congressional testimony that the VA needs “a new digital health platform” and seems to suggest it will pursue a custom-developed system rather than buy a commercially available product or upgrade VistA. Council says a working prototype will be available in a few months that “is aligned with the world-class technology everyone’s seen today and using in things like Facebook and Google and other capabilities. But it also is agile and it leverages what is called FHIR capability, which means we can bring things in, we can use them, we can change them, we can respond.” Lawmakers are justifiably concerned that the history of the VA specifically and government agencies in general suggests a high likelihood of expensive failure and lack of interoperability with the DoD, but Council says the cost-benefit analysis is solid. She also reiterated previous statements that the VA is putting its $624 million Epic patient scheduling system rollout on hold while it tests its own self-developed system that will cost just $6.4 million. The VA and Congress, anxious to deflect bad publicity about the VA’s wait time scandal, quickly threw IT money at the patient scheduling problem last year despite scant evidence implicating technology as the problem.
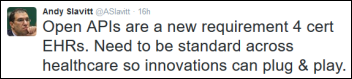
CMS Administrator Andy reiterates that EHR certification will require vendors to provide open APIs for interoperability.
Privacy and Security

The Department of Homeland Security’s US-CERT urges Windows PC users who have Apple’s QuickTime installed to de-install it immediately after a security firm finds major vulnerabilities and Apple quickly drops QuickTime for Windows support. It’s fine on Apple devices.
A federal appeals court rules that a healthcare company’s general liability insurer must defend it against security breach claims even when the policy doesn’t specifically include cyberbreach wording. .
Other
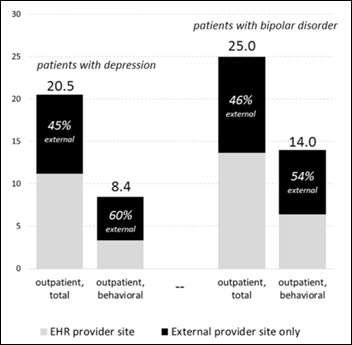
Jenn covered for me Thursday and mentioned the JAMIA-published study that found missing information about patients with diagnoses of depression or bipolar disorder, about which I will opine further. The authors try to make the case that primary care EHRs suffer from “data missingness” that indicates that “federal policies to date have tilted too far in accommodating EHR vendors’ desire for flexible, voluntary standards” that “can lock providers in to proprietary systems that cannot easily share data.” Underneath that big (and preachy) conclusion is a little study with a lot of problems:
- It analyzed data from 2009 only, eons ago in HITECH years (in fact, that was the same year that HITECH was passed, well before it had significant EHR impact).
- It covered patients from a single insurance plan’s patients, treated by a single medical practice, using a single EHR (Epic).
- The “data missingness” it claims involves only two behavioral health diagnoses that were likely treated by specialty providers (LCSW, PhD, psychiatrists) who weren’t HITECH-bribed to adopt EHRs and who often don’t use them because of privacy concerns and lack of benefit.
- The study matched EHR information to claims data in finding that 90 percent of acute psychiatric services were not captured in the EHR. The authors should have noted that many patients seeking behavioral health services pay cash to avoid creating a claims history, seek help from public services, or travel out of their own area for them to maintain privacy, all of which could impact their conclusions.
- It’s likely that some or even most of the patients with missing information would have opted out of automatic sharing of their behavioral health information given the chance.
- The authors blame EHR vendors for the lack of interoperability, but give the organization they studied a free ride in assuming that it freely exchanges information with any other provider who expresses interest.
- The study seems to state an expectation that every primary care provider’s EHR have a complete patient record from all sources of care, which is a nice dream, but as they correctly conclude is not today’s reality for many reasons, most of them unrelated to EHR vendors. That doesn’t necessarily mean the information isn’t available (via an HIE, records request, patient history, etc.) but only that it isn’t updated in real time across EHRs everywhere.
- Lack of information doesn’t necessarily change the treatment plan or outcome. Doctors have never had that information, electronic or otherwise, so it’s not like EHRs caused a new problem.
- The best conclusion is this: if you want the most nearly complete patient information available, use both EHR information and individual patient claims data across all commercial and governmental payers and present it from within the patient’s EHR record. That’s not how the system works for most PCPs, however.

Kansas City tax authorities approve reimbursing Cerner for $1.75 billion of the $4.45 billion construction cost of the company’s new The Trails campus. Cerner says the new space will allow it to add 16,000 jobs within 10 years and the increased post-construction assessment should generate $2.6 million of additional property taxes per year.
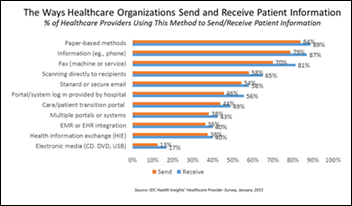
In Canada, Nova Scotia has spent $30 million on incentives for practices to use EHRs, but faxing is still the most common way for practices to communicate with each other because the government-approved systems aren’t interoperable.

Lee Memorial Health System (FL) comes up with creative excuses for earning a one-star quality rating from CMS: (a) the hospital converted to Epic just three years ago; (b) incomplete EHR coding caused the health system to be compared unfairly; (c) CMS doesn’t take into account tourist-driven seasonality; and (d) CMS doesn’t take socioeconomic factors into account and therefore penalizes hospitals that treat poor patients who are sicker (a minor variant of the “our patients are sicker” explanation). The hospital didn’t suggest that it will actually treat patients any differently even though its largest customer gave it the lowest possible quality score.
Weird News Andy notes that “even junkies are logical” as evidenced by this story, in which drug abusers are injecting themselves in the bathrooms and parking garages of Massachusetts General Hospital so they can get medical help quickly if they overdose. MGH says people are even tying themselves to the emergency pull cords in its bathrooms so the alarm will go off if they keel over in a narcotic stupor.
Sponsor Updates
- A Spok case study describes the 50 percent of University of Utah Health Care’s incoming residents and medical students who choose to communicate using Spok Mobile for secure text messaging.
- Medecision President and CEO Deborah M. Gage is named as one of the most powerful women in healthcare IT.
- T-System will exhibit at the UCAOA National Urgent Care Convention April 17-20 in Orlando.
- Huron Consulting Group is named by Forbes as one of America’s Best Employers for the second consecutive year.
- Wellsoft will exhibit at TCEP Connect 2016 April 21-24 in Galveston, TX.
- ZirMed will exhibit at the California MGMA Conference April 21-23 in Sonoma.
- Zynx Health will exhibit at the ANIA 2016 Conference April 21-23 in San Francisco.
- PatientPay shows commitment to rid paper from healthcare billing in support of The Nature Conservancy.
- QPID Health CMO Mike Zalis will speak at the North Carolina Association for Healthcare Quality Annual Conference April 21-22 in Durham.
- Huffington Post interviews Red Hat CEO Jim Whitehurst.
- The SSI Group will exhibit at the Healthcare Finance Institute April 17-19 in Tysons Corner, VA.
- Streamline Health will exhibit at the 2016 California MGMA Annual Conference April 21-23 in Sonoma.
Blog Posts
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Send news or rumors.
Contact us.


















































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…